J Korean Orthop Assoc.
2010 Aug;45(4):314-320.
The Revision Operation Rate for Adjacent Segmental Degeneration by Survival Analysis in Mono-segment Lumbar Fusion
- Affiliations
-
- 1Seoul Spine Institute, Inje University Sanggye Paik Hospital, Seoul, Korea. kjh1026@paik.ac.kr
Abstract
- PURPOSE
To analyze survival rates of patients after mono-segmental lumbar or lumbosacral fusion and to evaluate factors affecting the revision operation due to adjacent segmental degeneration. MATERIALS AND
METHODS
This study enrolled 1,206 patients who had mono-segmental lumbar or lumbosacral fusion between March 1997 and December 2006 at the Seoul Spine Institute. The survival rates for the revision operation due to adjacent segmental degeneration were analyzed retrospectively. The age at index operation, sex, etiologic diagnosis, fusion method, fusion level, substance of bone graft, operator, body mass index (BMI), and smoking were considered as risk factors for the revision operation.
RESULTS
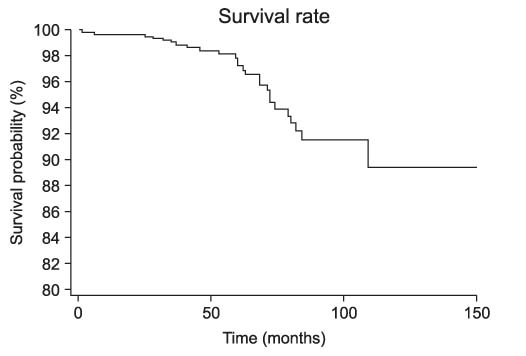
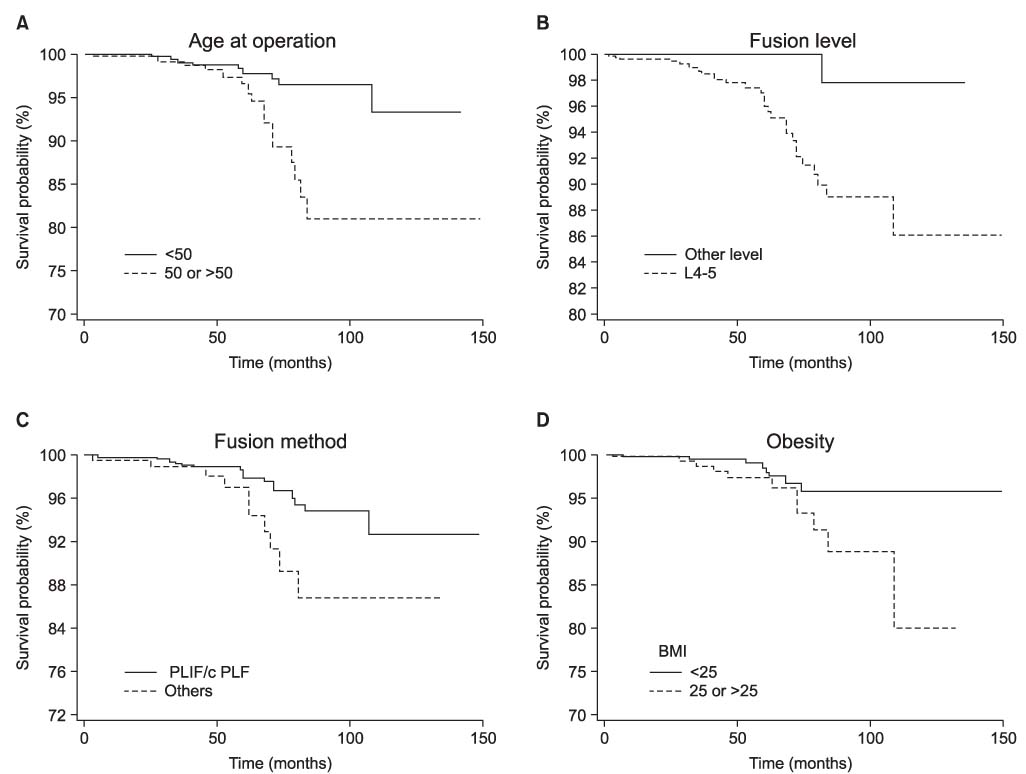
There were 27 patients with a revision operation for adjacent segmental degeneration (2.24%). The average follow-up period was 39.0 months (6 months to 12 years 6 months) and the average age at operation was 47.0 years (13 to 85 years). The survival rate at 5 years was 97.3%, and at 10 years it was 89.4%. Patients less than 50 years old had a significantly lower revision operation rate than those aged 50 or more (p=0.002). When fusion between the 4th lumbar and the 5th lumbar spinal vertebrae was done, the revision operation rate was significantly higher than for other levels (p=0.003). Obese patients with BMI> or =25 had a significantly higher revision rate than did patients with BMI<25 (p=0.040). In a comparison of circumferential fusion versus other types of fusion, circumferential fusion had a lower revision rate and the difference was significant (p=0.021). Other factors such as diagnosis, sex, surgeon, substance used for the bone graft, and smoking were not significant for revision rate (ps>0.05). In multivariate analysis, age alone was a significant risk factor (p=0.048, Hazard ratio=2.50).
CONCLUSION
The most important factor for survival without revision surgery for adjacent segmental degeneration following instrumented mono-segment lumbar or lumbosacral fusion is the age at index operation. Patients 50 year-old or older should be informed of the possibility of adjacent segmental disease after instrumented mono-segment lumbar or lumbosacral fusion.
Keyword
MeSH Terms
Figure
Reference
-
1. Cho JL, Park YS, Han JH, Lee CH, Rho WI. The changes of adjacent segments after spinal fusion, follow-up more than three years after spinal fusion. J Korean Soc Spine Surg. 1998. 5:239–246.2. Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999. 90:163–169.
Article3. Ha KY, Kim KW, Park SJ, Lee YH. Changes of the adjacent-unfused mobile segment after instrumental lumbar fusion, more than 5-years follow-up. J Korean Soc Spine Surg. 1998. 5:205–214.4. Shono Y, Kaneda K, Abum K, McAfee PC, Cunningham BW. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine (Phila Pa 1976). 1998. 23:1550–1558.
Article5. Frymoyer JW, Hanley EN Jr, Howe J, Kuhlmann D, Matteri RE. A comparison of radiographic findings in fusion and nonfusion patients ten or more years following lumbar disc surgery. Spine (Phila Pa 1976). 1979. 4:435–440.
Article6. Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976). 1988. 13:375–377.
Article7. Schlegel JD, Smith JA, Schleusener RL. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar and lumbosacral fusion. Spine (Phila Pa 1976). 1996. 21:970–981.8. Grouw AV, Nadel CI, Weierman RJ, Lowell HA. Long term follow-up of patients with idiopathic scoliosis treated surgically: a preliminary subjective study. Clin Orthop Relat Res. 1976. 117:197–201.
Article9. Hambly MF, Wiltse LL, Raghavan N, Schneiderman G, Koenig C. The transition zone above a lumbosacral fusion. Spine (Phila Pa 1976). 1998. 23:1785–1792.
Article10. Aota Y, Kumano K, Hirabayashi S. Postfusion instability at the adjacent segments after rigid pedicle screw fixation for degenerative lumbar spinal disorders. J Spinal Disord. 1995. 8:464–473.
Article11. Guigui P, Lambert P, Lassale B, Deburge A. Long-term outcome at adjacent levels of lumbar arthrodesis. Rev Chir Orthop Reparatrice Appar Mot. 1997. 83:685–696.12. Frymoyer JW, Hanley E, Howe J, Kuhlmann D, Matteri R. Disc excision and spine fusion in the management of lumbar disc disease. A minimum ten-year follow-up. Spine (Phila Pa 1976). 1978. 13:1–6.13. Brunet JA, Wiley JJ. Acquired spondylolysis after spinal fusion. J Bone Joint Surg Br. 1984. 66:720–724.
Article14. Cunningham BW, Kotani Y, McNulty PS, Cappuccino A, McAfee PC. The effect of spinal destabilization and instrumentation on lumbar intradiscal pressure: an in vitro biomechanical analysis. Spine (Phila Pa 1976). 1997. 22:2655–2663.15. Lee CK, Langrana NA. Lumbosacral spinal fusion. A biomechanical study. Spine (Phila Pa 1976). 1984. 9:574–581.
Article16. Weinhoffer SL, Guyer RD, Herbert M, Griffith SL. Intradiscal pressure measurements above an instrumented fusion. A cadevaric study. Spine (Phila Pa 1976). 1995. 20:526–531.17. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 2004. 29:1938–1944.
Article18. Miyakoshi N, Abe E, Shimada Y, Okuyama K, Suzuki T, Sato K. Outcome of one-level posterior lumbar interbody fusion for spondylolithesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine (Phila Pa 1976). 2000. 25:1837–1842.19. Etebar S, Cahill DW. Risk factors for adjacent-segment failure following lumbar fixation with rigid instrumentation for degenerative instability. J Neurosurg. 1999. 90:2 Suppl. 163–169.
Article20. Rahm MD, Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord. 1996. 9:392–400.21. Gardner VO, Amstrong GW. Long-term lumbar facet joint changes in spinal fracture patients treated with Harrington rods. Spine (Phila Pa 1976). 1990. 15:479–484.
Article22. Nagata H, Schendel MJ, Transfeldt EE, Lewis JL. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine (Phila Pa 1976). 1993. 18:2471–2479.
Article23. Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine (Phila Pa 1976). 2004. 29:1535–1540.
Article24. Goel VK, Voo LM, Weinstein JN, Liu YK, Okuma T, Njus GO. Response of the ligamentous lumbar spine to cyclic bending loads. Spine (Phila Pa 1976). 1998. 13:294–300.
Article25. Lehmann TR, Spratt KF, Tozzi JE, et al. Long-term follow-up of lower lumbar fusion patients. Spine (Phila Pa 1976). 1987. 12:97–104.
Article26. Ha KY, Kim YH, Kang KS. Surgery for adjacent segment changes after lumbosacral fusion. J Korean Soc Spine Surg. 2002. 9:332–340.
Article27. Aiki H, Ohwada O, Kobayashi H, et al. Adjacent segment stenosis after lumbar fusion requiring second operation. J Orthop Sci. 2005. 10:490–495.
Article28. Ahn DK, Lee S, Jeong KW, Park JS, Cha SK, Park HS. Adjacent segment failure after lumbar spine fusion: controlled study for risk factors? J Korean Orthop Assoc. 2005. 40:203–208.
Article29. Penta M, Sandhu A, Fraser RD. Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion. Spine (Phila Pa 1976). 1995. 20:743–747.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revision Arthrodesis After Lumbar Fusion in Degenerative Lumbar Disease
- The Causes of Revision Arthrodesis for the Degenerative Changes at the Adjacent Segment after Lumbosacral Fusion for Degenerative Lumbar Diseases
- A Comparison of Adjacent Segment Diseases Above One Versus Above Two Vertebral Segment after Spinal Fusion of the Degenerative Lumbar Disease
- Surgical Treatment of Adjacent Segment Degeneration after Spinal Fusion in Degenerative Lumbar Disc Disease
- Revision Surgery for Spinal Stenosis Developed at the Adjacent Segment after Lumbar Fusion