J Korean Diabetes Assoc.
2006 Jan;30(1):64-72.
Prevalence of Fungal Infection on Foot in Diabetic Patients and Correlation between Diabetic Ulcer and Fungal Infection on Foot
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, The Catholic University of Korea.
Abstract
-
BACKGROUND: The purpose of this study was to determine the prevalence of fungal infection and ulcer on the feet of diabetic patients and the existence of correlation between ulcer and fungal infection.
METHODS
A total of 21,693 outpatients diagnosed as diabetes mellitus at the department of endocrinology of 32 hospitals were examined. The diabetic patients with foot problems were consulted to the department of dermatology. Physical examination and KOH preparation were performed by a dermatologist.
RESULTS
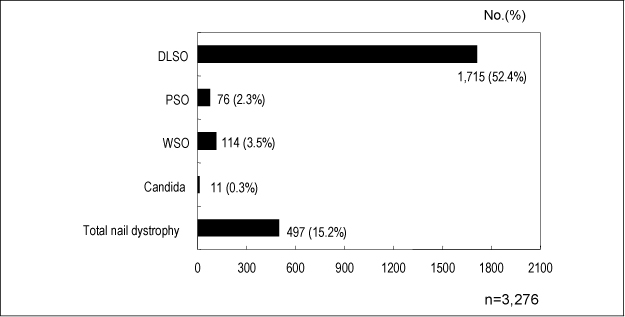
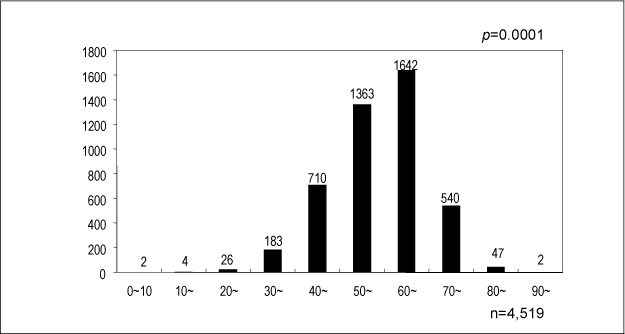
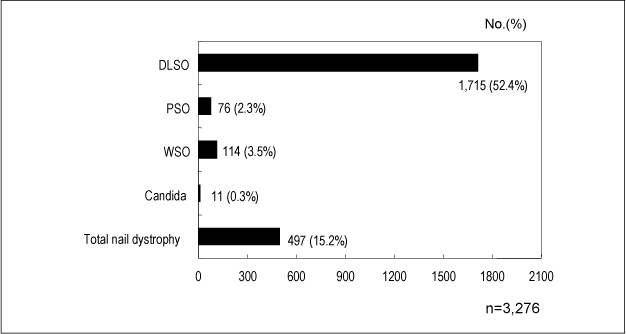
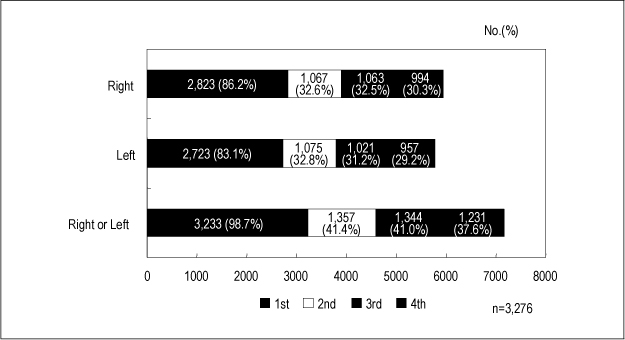
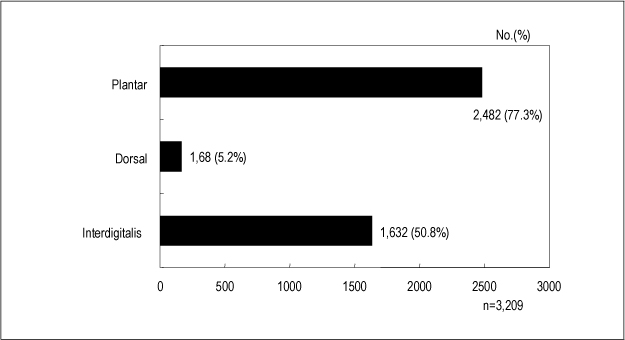
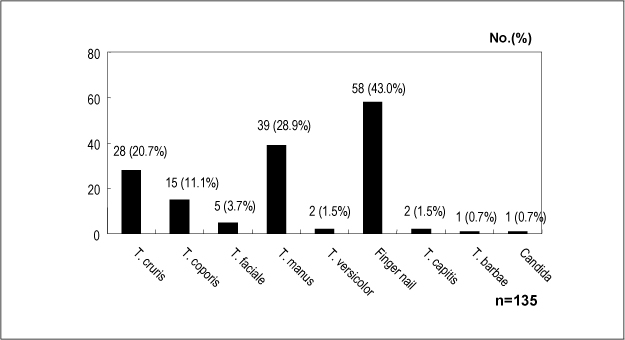
13,271 patients had certain kinds of foot problem, accounting for 61.2% of 21,693 diabetics examined. Of these, fungal foot disease was found in 10,403 patients that constituted 78.4%(48.0% of the entire diabetic population). Tinea pedis was the diagnosis in 6,496(29.9%), onychomycosis in 7,783(35.9%), and coexistence was in 3,883(17.9%). Foot deformity was in 1,346(6.2% of diabetics; 10.1% of foot disease), nonpalpable pulse in 1,051 (4.8%; 7.9%), and foot ulcer was in 425(2.0%; 3.2%), following in a descending order of frequency. Odds ratios for diabetic foot ulcer were 2.5 in patients with the foot deformity, 1.6 with fungal foot disease and 2.2 with non-palpable pulse. Conversely, odds ratios for fungal foot disease were 2.5 with foot deformity, and 1.6 with foot ulcer. A total of 5,486 patients paid visit to the department of dermatology. Of these, 4,519 patient were diagnosed with fungal infection through physical examination and KOH smear by dermatologists. The population were comprised of 2,272 males and 2,247 females, showing similar prevalences between sexes. However, age did have positive correlation regarding prevalence of fungal foot disease. The number of diabetic patients with toenail problems was 3,847(70%) and onychomycosis was proven mycologically in 3,276 patients. Onychomycosis of distal subungal type was the most common clinical finding, most frequently involving the great toenails. Abnormal skin findings of the foot were seen in 3,885 (70.8%) and tinea pedis was found in 3,209(58.5%), most commonly involving the soles.
CONCLUSION
This study showed that fungal infection might be regarded as a risk factor of foot ulcer. Treatment of fungal infection in diabetic patients might prevent diabetic foot disease such as ulcer and reduce the disability, morbidity and mortality in diabetic patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Barcelo A. Monograph series on aging-related diseases. VIII: non-insulin-dependent diabetes mellitus (NIDDM). Chronic Dis Can. 1996. 17:1–20.2. Gupta AK, Konnikav N, MacDonald P, Rich P, Rodger NW, Edmonds MW, McManus R, Summerbell RC. Prevalence and epidemiology of toenail onychomycosis in diabetic subjects: a multicentre survey. Br J Dermatol. 1998. 139:665–671.3. Harris MI. Descriptive epidemiology of diabetes mellitus. Diabetes in America. 1995. 2nd ed. Bethesda: Diane publishing;46.5. Rich P. Special patient populations: onychomycosis in the diabetic patient. J Am Acad Dermatol. 1996. 35:S10–S12.6. Most RS, Sinnock P. The epidemiology of lower extremity amputation in diabetic individuals. Diabetes Care. 1983. 6:87–91.9. Wilson RM. Neutrophil function in diabetes. Diabetic Med. 1986. 3:509–512.10. Rayfield ES, Ault M. Infection and diabetes: The case for glucose tolerance. Am J Med. 1982. 72:439–443.11. Roseeuw D, Katsambas A, Burzykawski T, Molenberghs G, Marynissen G. The risk of fungal foot infections in diabetic patients. J Eur Acad Dermatol Venereol. 1999. 12:S220.14. Gupta AK, Humke S. The prevalence and management of onychomycosis in diabetic patients. Eur J Dermatol. 2000. 10:379–384.15. Rich P, Hare A. Onychomycosis in a special patient population: focus on the diabetic. Int J Dermatol. 1999. 38(Suppl 2):17–19.16. Boyko WL, Doyle JJ, Ryu S, Gause D. Onychomycosis and its impact on secondary infection development in the diabetic population. Presented at the 4th Annual International meeting of the International society for pharmacoeconomics and outcomes research (ISPOR). 1999. May 23-26.17. Lugo-Somolinos A, Sanchez JL. Prevalence of dermatophytosis in patients with diabetes. J Am Acad Dermatol. 1992. 26:408–410.18. Buxton PK, Milne LJR, Prescott RJ, Proudfoots MC, Stuart FM. The prevalence of dermatophyte infection in well-controlled diabetics and the response to Trichophyton antigen. Br J Dermatol. 1996. 134:900–903.19. Romano C, Massai L, Asta F, Signorini M. Prevalence of dermatophytic skin and nail infections in diabetic patients. Mycoses. 2001. 83–86.20. Boulton AJM. The diabetic foot: Neuropathic in aetiology? Diabet Med. 1990. 7:852–858.21. Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation: Basis for prevention. Diabetes Care. 1990. 13:513–521.22. Veves A, Murray HJ, Young MJ, Boulton AJM. The risk of foot ulceration in diabetic patients with high foot pressures: a prospective study. Diabetologia. 1992. 35:660–663.23. Albreski DA, Gross EG. The safety of itraconazole in the diabetic population. J Am Pediatr Med Assoc. 1999. 89:339–345.24. Rich P. Onychomycosis and tinea pedis in patients with diabetes. J Am Acad Dermatol. 2000. 43:S130–S134.