J Menopausal Med.
2014 Apr;20(1):43-46.
Perimenopausal Ovarian Carcinoma Patient with Subclavian Node Metastasis Proven by Immunohistochemistry
- Affiliations
-
- 1Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea. minkyukim@skku.edu
- 2Division of Gynecologic Oncology, Department of Pathology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
Abstract
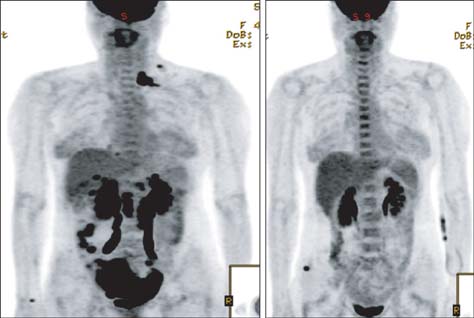
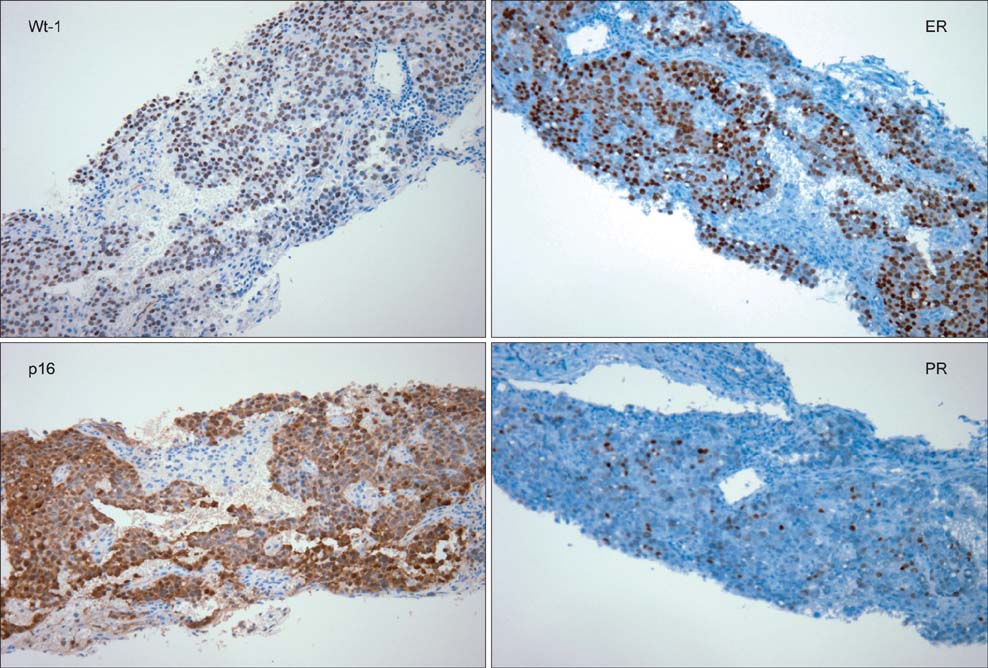
- Ovarian cancer is the seventh most common cancer in the world and the fifth most common cause of death from cancer; it is responsible for over half of all deaths related to gynecological cancers. The presence of lymphatic metastasis is an important prognostic factor in ovarian cancer. Nodal metastases to the pelvic and the para-aortic lymph nodes are common, particularly in an advanced of the disease (stages III-IV). The finding of distant nodal metastasis, especially subclavian lymph node metastasis, from ovarian carcinoma is very uncommon. 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) or FDG-PET/computed tomography (CT) provides an improved imaging for detecting metastatic lymph nodes in patients with ovarian cancer. Immunohistochemically, ovarian carcinoma cells are positive for estrogen receptor, progesterone receptor, cancer antigen 125, Wilms' tumor 1 protein, and p53; they are negative for thyroid transcription factor (TTF-1) and caudal-related homeobox 2 (CDX-2). This report describes a Korean woman diagnosed with ovarian cancer with subclavian lymph node metastasis revealed by FDG PET/CT and verified by an immunohistochemical staining. Differentiating between the primary ovarian lesion and the metastatic lesion will allow the initiation of an appropriate treatment and help predict the prognosis.
Keyword
MeSH Terms
-
Cause of Death
Estrogens
Female
Genes, Homeobox
Humans
Immunohistochemistry*
Lymph Nodes
Lymphatic Metastasis
Neoplasm Metastasis*
Ovarian Neoplasms
Positron-Emission Tomography and Computed Tomography
Prognosis
Receptors, Progesterone
Thyroid Gland
Transcription Factors
Wilms Tumor
Estrogens
Receptors, Progesterone
Transcription Factors
Figure
Reference
-
1. Bristow RE, Duska LR, Lambrou NC, Fishman EK, O'Neill MJ, Trimble EL, et al. A model for predicting surgical outcome in patients with advanced ovarian carcinoma using computed tomography. Cancer. 2000; 89:1532–1540.2. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012; 62:10–29.3. Burghardt E, Girardi F, Lahousen M, Tamussino K, Stettner H. Patterns of pelvic and paraaortic lymph node involvement in ovarian cancer. Gynecol Oncol. 1991; 40:103–106.4. Onda T, Yoshikawa H, Yokota H, Yasugi T, Taketani Y. Assessment of metastases to aortic and pelvic lymph nodes in epithelial ovarian carcinoma. A proposal for essential sites for lymph node biopsy. Cancer. 1996; 78:803–808.5. Chen SS. Survival of ovarian carcinoma with or without lymph node metastasis. Gynecol Oncol. 1987; 27:368–372.6. Scarabelli C, Gallo A, Zarrelli A, Visentin C, Campagnutta E. Systematic pelvic and para-aortic lymphadenectomy during cytoreductive surgery in advanced ovarian cancer: potential benefit on survival. Gynecol Oncol. 1995; 56:328–337.7. Tsuruchi N, Kamura T, Tsukamoto N, Akazawa K, Saito T, Kaku T, et al. Relationship between paraaortic lymph node involvement and intraperitoneal spread in patients with ovarian cancer--a multivariate analysis. Gynecol Oncol. 1993; 49:51–55.8. Parazzini F, Valsecchi G, Bolis G, Guarnerio P, Reina S, Polverino G, et al. Pelvic and paraortic lymph nodal status in advanced ovarian cancer and survival. Gynecol Oncol. 1999; 74:7–11.9. Yuan Y, Gu ZX, Tao XF, Liu SY. Computer tomography, magnetic resonance imaging, and positron emission tomography or positron emission tomography/computer tomography for detection of metastatic lymph nodes in patients with ovarian cancer: a meta-analysis. Eur J Radiol. 2012; 81:1002–1006.10. Castellucci P, Perrone AM, Picchio M, Ghi T, Farsad M, Nanni C, et al. Diagnostic accuracy of 18F-FDG PET/CT in characterizing ovarian lesions and staging ovarian cancer: correlation with transvaginal ultrasonography, computed tomography, and histology. Nucl Med Commun. 2007; 28:589–595.11. Nam EJ, Yun MJ, Oh YT, Kim JW, Kim JH, Kim S, et al. Diagnosis and staging of primary ovarian cancer: correlation between PET/CT, Doppler US, and CT or MRI. Gynecol Oncol. 2010; 116:389–394.12. Risum S, Høgdall C, Loft A, Berthelsen AK, Høgdall E, Nedergaard L, et al. Does the use of diagnostic PET/CT cause stage migration in patients with primary advanced ovarian cancer? Gynecol Oncol. 2010; 116:395–398.13. Hynninen J, Auranen A, Carpén O, Dean K, Seppänen M, Kemppainen J, et al. FDG PET/CT in staging of advanced epithelial ovarian cancer: frequency of supradiaphragmatic lymph node metastasis challenges the traditional pattern of disease spread. Gynecol Oncol. 2012; 126:64–68.14. Skagias L, Ntinis A, Vasou O, Kondi-Pafiti A, Politi E. Ovarian carcinoma presenting with axillary lymph node metastasis: a case diagnosed by fine-needle aspiration and brief review of the literature. Diagn Cytopathol. 2008; 36:891–893.15. Hecht JL, Pinkus JL, Weinstein LJ, Pinkus GS. The value of thyroid transcription factor-1 in cytologic preparations as a marker for metastatic adenocarcinoma of lung origin. Am J Clin Pathol. 2001; 116:483–488.16. Hershlag A, Schuster MW. Return of fertility after autologous stem cell transplantation. Fertil Steril. 2002; 77:419–421.17. Kim TH, Lee HH, Chung SH, Kwak JJ, Lee BI, Hong YP. Serous adenocarcinoma arising from ovarian endometriosis after menopause. Korean J Obstet Gynecol. 2010; 53:365–370.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Recurrence of Ovarian Carcinoma Presenting as Only Axillary Lymphatic Metastasis: A Case Report
- Solitary Axillary Lymph Node Metastasis without Breast Involvement from Ovarian Cancer: Case Report and Brief Literature Review
- Clinical Characteristics of Ovarian Metastasis from Colorectal Cancer
- A case of minimal uterine serous carcinoma with distant lymph node metastasis without peritoneal dissemination
- Primary Squamous Cell Carcinoma of the Ovary: A Case Report