Tuberc Respir Dis.
2014 Jul;77(1):34-37.
Multiple Hypercoagulability Disorders at Presentation of Non-Small-Cell Lung Cancer
- Affiliations
-
- 1Department of Internal Medicine, Inha University College of Medicine, Incheon, Korea. jsryu@inha.ac.kr
Abstract
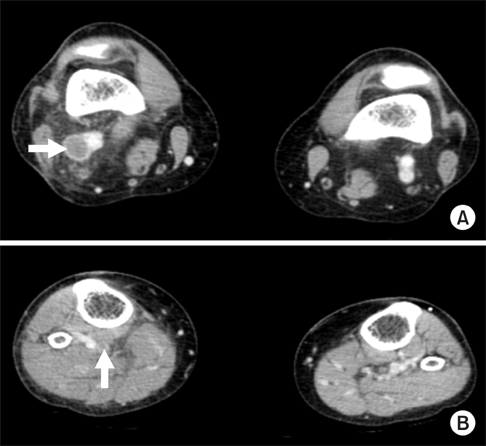
- Hypercoagulability disorders are commonly encountered in clinical situations in patients with a variety of cancers. However, several hypercoagulability disorders presenting as first symptoms or signs in cancer patients have rarely been reported. We herein described a case of a woman with adenocarcinoma of the lung presenting with deep vein thrombosis, nonbacterial thrombotic endocarditis, recurrent cerebral embolic infarction, and heart failure.
Keyword
MeSH Terms
Figure
Reference
-
1. Falanga A, Ofosu FA, Delaini F, Oldani E, Dewar L, Lui L, et al. The hypercoagulable state in cancer patients: evidence for impaired thrombin inhibitions. Blood Coagul Fibrinolysis. 1994; 5:Suppl 1. S19–S23.2. Dipasco PJ, Misra S, Koniaris LG, Moffat FL Jr. Thrombophilic state in cancer, part I: biology, incidence, and risk factors. J Surg Oncol. 2011; 104:316–322.3. Glassman AB. Hemostatic abnormalities associated with cancer and its therapy. Ann Clin Lab Sci. 1997; 27:391–395.4. Falanga A, Rickles FR. Pathophysiology of the thrombophilic state in the cancer patient. Semin Thromb Hemost. 1999; 25:173–182.5. Gross L, Friedberg CK. Nonbacterial thrombotic endocarditis: classification and general description. Arch Intern Med. 1936; 58:620–640.6. el-Shami K, Griffiths E, Streiff M. Nonbacterial thrombotic endocarditis in cancer patients: pathogenesis, diagnosis, and treatment. Oncologist. 2007; 12:518–523.7. Lopez JA, Ross RS, Fishbein MC, Siegel RJ. Nonbacterial thrombotic endocarditis: a review. Am Heart J. 1987; 113:773–784.8. Borowski A, Ghodsizad A, Cohnen M, Gams E. Recurrent embolism in the course of marantic endocarditis. Ann Thorac Surg. 2005; 79:2145–2147.9. Chino F, Kodama A, Otake M, Dock DS. Nonbacterial thrombotic endocarditis in a Japanese autopsy sample: a review of eighty cases. Am Heart J. 1975; 90:190–198.10. Taniyama D, Yamamoto R, Kawasaki M, Kamata H, Miyamoto K, Mashimo S, et al. Nonbacterial thrombotic endocarditis leading to acute heart failure due to aortic stenosis in a patient with lung cancer. Intern Med. 2013; 52:1617–1620.11. Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. N Engl J Med. 2000; 343:1846–1850.12. Caine GJ, Stonelake PS, Lip GY, Kehoe ST. The hypercoagulable state of malignancy: pathogenesis and current debate. Neoplasia. 2002; 4:465–473.13. Connolly GC, Dalal M, Lin J, Khorana AA. Incidence and predictors of venous thromboembolism (VTE) among ambulatory patients with lung cancer. Lung Cancer. 2012; 78:253–258.14. Young A, Chapman O, Connor C, Poole C, Rose P, Kakkar AK. Thrombosis and cancer. Nat Rev Clin Oncol. 2012; 9:437–449.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Early Gastric Cancer Associated with Small Cell Lung Cancer
- Multiple primary lung cancer: Synchronous small cell lung carcinoma and squamous cell carcinoma
- Clinical Characteristics and Abnormal p53 Expression of Lung Cancer Associated with Multiple Primary Cancer
- Druggable Targets of Squamous Cell Lung Cancer
- Adjuvant Chemotherapy for Completely Resected Non-Small Cell Lung Cancer