Urogenit Tract Infect.
2015 Oct;10(2):112-119. 10.14777/uti.2015.10.2.112.
Change of Antibiotic Resistance to the Causative Organisms of Pelvic Wound Infection for Recent 5 Years
- Affiliations
-
- 1Department of Urology, National Police Hospital, Seoul, Korea. drmsk@korea.com
- 2Department of Plastic Surgery, National Police Hospital, Seoul, Korea.
- 3Department of Laboratoy Medicine, National Police Hospital, Seoul, Korea.
- KMID: 2319436
- DOI: http://doi.org/10.14777/uti.2015.10.2.112
Abstract
- PURPOSE
We researched microbial profiles and the antimicrobial resistance profile of wound infection of the pelvic area in Korea for the recent 5 years in order to provide useful information on the choice of adequate drugs in the treatment of pelvic wound infection.
MATERIALS AND METHODS
We retrospectively analyzed 211 pelvic wound culture samples and their antimicrobial resistance in 198 in- or out-patients of the Urology and Plastic surgery department from January 2010 to December 2014.
RESULTS
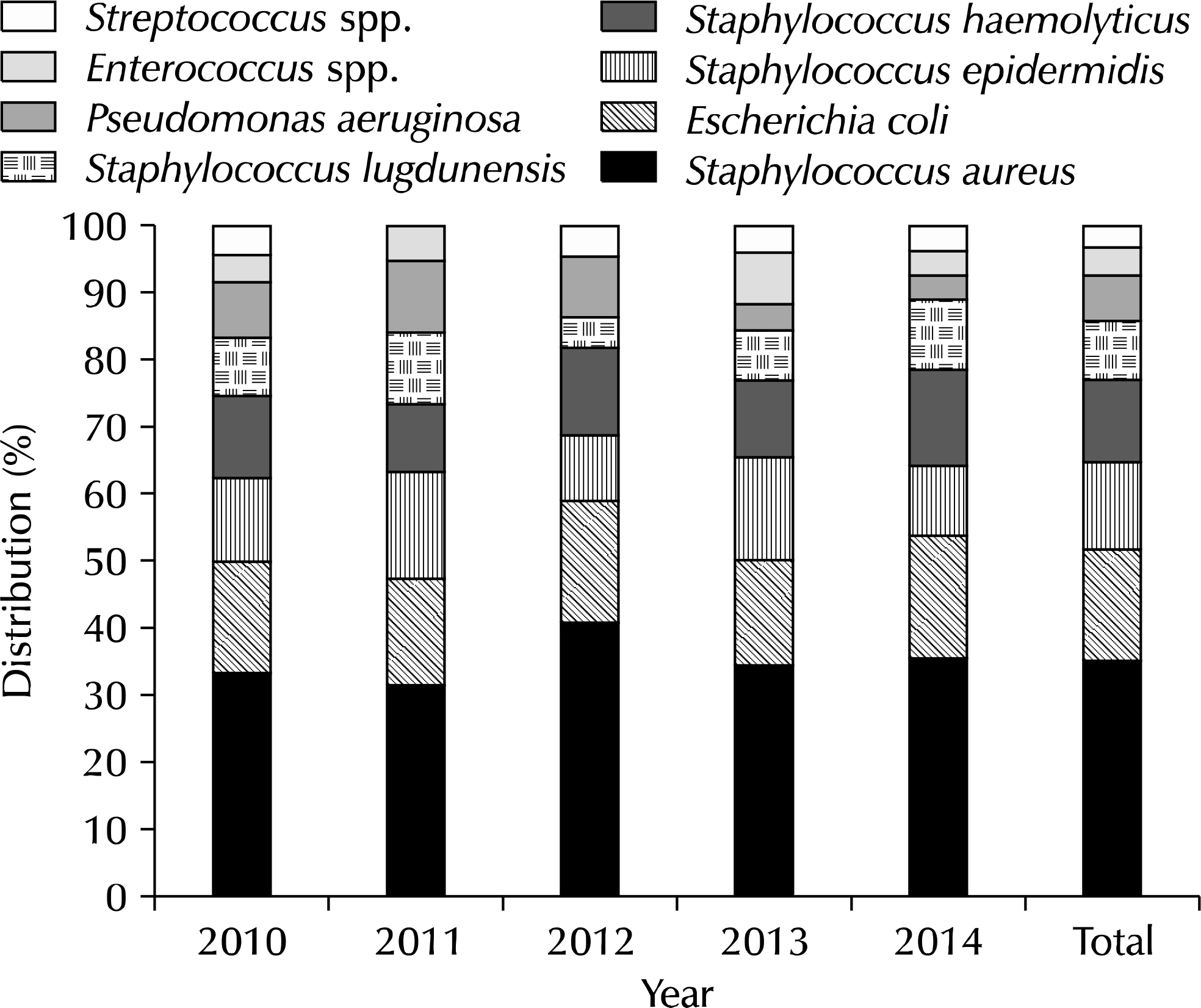
Of the total samples, Staphylococcus aureus was isolated most frequently (35.3%), followed by Escherichia coli (15.1%), Staphylococcus epidermidis (12.6%), Staphylococcus haemolyticus (12.6%), Staphylococcus lugdunensis (8.4%), Pseudomonas aeruginosa (6.7%), Enterococcus spp. (4.2%), and Streptococcus spp. (3.3%). There were no notable changes of bacterial distribution for 5 years. For Gram-positive isolates, the oxacillin resistance rate for Gram-positive bacteria was 42.6% and showed an increasing tendency for the recent 5 years. Piperacillin, rifampicin, and vancomycin had low resistance for Gram-positive bacteria. Carbapenems, piperacillin/tazobactam had low resistance for Gram-negative bacteria. The Gram-positive organisms were more sensitive to many antibiotics in contrast to the Gram-negative organisms.
CONCLUSIONS
Of varied causative organisms and susceptibility of the pelvic wound site, the most frequently infected organisms of the pelvic area were S. aureus, followed by E. coli. The methicillin resistive S. aureus (MRSA) incidence showed a tendency to increase yearly, thus selection or early change of antibiotics considering MRSA is recommended if the antibiotic response is poor. Gram-negative bacteria has a higher resistance rate compared with Gram-positive bacteria and had carbapenems and piperacillin/tazobactam.
MeSH Terms
-
Anti-Bacterial Agents
Carbapenems
Drug Resistance
Drug Resistance, Microbial*
Enterococcus
Escherichia coli
Gram-Negative Bacteria
Gram-Positive Bacteria
Humans
Incidence
Korea
Methicillin
Methicillin-Resistant Staphylococcus aureus
Outpatients
Oxacillin
Pelvic Infection
Piperacillin
Pseudomonas aeruginosa
Retrospective Studies
Rifampin
Staphylococcus aureus
Staphylococcus epidermidis
Staphylococcus haemolyticus
Staphylococcus lugdunensis
Streptococcus
Surgery, Plastic
Urology
Vancomycin
Wound Infection*
Wounds and Injuries*
Anti-Bacterial Agents
Carbapenems
Methicillin
Oxacillin
Piperacillin
Rifampin
Vancomycin
Figure
Reference
-
1.Leaper DJ., Harding KG. Wounds: biology and management. Oxford: Oxford University Press;1998.2.Bowler PG., Duerden BI., Armstrong DG. Wound microbiology and associated approaches to wound management. Clin Microbiol Rev. 2001. 14:244–69.
Article3.Forbes BA., Sahm DF., Weissfeld AS. Skin soft tissue and wound infections. Forbes BA, Sahm DF, Weissfeld AS, Baron EJ, editors. editors.Bailey & Scott's diagnostic microbiology. 10th ed.St. Louis: Mosby;1998. p. 972–84.4.Dykhuizen RS., Trent RJ., Pacitti DP., Reid TM., Douglas JG., Smith CC. An analysis of 900 consecutive admissions to a regional infection unit. J Infect. 1994. 29:189–93.
Article5.Bannister BA., Begg NT., Gillespie SH. Skin, mucosal and soft tissue infections. Bannister BA, Begg NT, Gillespie SH, editors. editors.Infectious disease. Oxford: Blackwell Science;1996. p. 76–102.6.Finch R. Skin and soft-tissue infections. Lancet. 1988. 1:164–8.
Article7.Sands K., Vineyard G., Platt R. Surgical site infections occurring after hospital discharge. J Infect Dis. 1996. 173:963–70.
Article8.Garner JS. CDC guideline for prevention of surgical wound infections, 1985. Supersedes guideline for prevention of surgical wound infections published in 1982. (Originally published in November 1985). Revised. Infect Control. 1986. 7:193–200.9.Gaynes RP., Culver DH., Horan TC., Edwards JR., Richards C., Tolson JS. Surgical site infection (SSI) rates in the United States, 1992-1998: the National Nosocomial Infections Surveillance System basic SSI risk index. Clin Infect Dis. 2001. 33(Suppl 2):S69–77.
Article10.Lee MS., Chong YS. Characteriscs of methicillin-resistant Staphylococcus aureus isolated from wounds in Korean patients. J Infect Chemother. 1996. 2:130–5.11.Kim JM., Lee SD., Jo WY. Correlation between wound dehescence after major urologic surgery and MRSA Infection. Korean J Urol. 2006. 47:298–302.
Article12.Lee JH., Han HS., Min SK., Lee HK., Lee JH., Kim YW, et al. Surveillance of surgical wound infections among patients from the department of surgery: prospective trial. J Korean Surg Soc. 2004. 66:133–7.13.Kim DW., Bong JG., Jeong JH., Lee YS., Park JH., Lee BC. Risk factors and prognostic influences of burn wound infection. J Korean Surg Soc. 2001. 61:195–202.14.Pondei K., Fente BG., Oladapo O. Current microbial isolates from wound swabs, their culture and sensitivity pattern at the niger delta university teaching hospital, okolobiri, Nigeria. Trop Med Health. 2013. 41:49–53.
Article15.Basu S., Ramchuran Panray T., Bali Singh T., Gulati AK., Shukla VK. A prospective, descriptive study to identify the microbiological profile of chronic wounds in outpatients. Ostomy Wound Manage. 2009. 55:14–20.16.Gupta AK., Batra P., Mathur P., Karoung A., Thanbuana BT., Thomas S, et al. Microbial epidemiology and antimicrobial susceptibility profile of wound infections in outpatients at a level 1 trauma centre. J Patient Saf Infect Control. 2015 Jul 15. [Epub].DOI: doi: 10.1016/j.jpsic.2015.06.001.
Article17.Wariso BA., Nwachukwu CO. A survey of common pathogens in wound in patients at the University of Port Harcourt Teaching Hospital (U.P.T.H), Port Harcourt. West Afr J Med. 2003. 22:50–4.
Article18.Phillips J., O'Grady H., Baker E. Prevention of surgical site infections. Surgery. 2014. 32:468–71.
Article19.Kim JM., Lee SD., Jang CH. A single center study of the change of antibiotic resistance to the causative organisms of urinary tract infection for recent 10 years. Korean J Urogenit Tract Infect Inflamm. 2008. 3:63–74.20.Hooton TM., Stamm WE. Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin North Am. 1997. 11:551–81.
Article21.Jones ME., Karlowsky JA., Draghi DC., Thornsberry C., Sahm DF., Nathwani D. Epidemiology and antibiotic susceptibility of bacteria causing skin and soft tissue infections in the USA and Europe: a guide to appropriate antimicrobial therapy. Int J Antimicrob Agents. 2003. 22:406–19.
Article22.Kaul R., McGeer A., Low DE., Green K., Schwartz B. Population-based surveillance for group A streptococcal necrotizing fasciitis: clinical features, prognostic indicators, and microbiologic analysis of seventy-seven cases. Ontario Group A Streptococcal Study. Am J Med. 1997. 103:18–24.23.Moet GJ., Jones RN., Biedenbach DJ., Stilwell MG., Fritsche TR. Contemporary causes of skin and soft tissue infections in North America, Latin America, and Europe: report from the SENTRY Antimicrobial Surveillance Program (1998-2004). Diagn Microbiol Infect Dis. 2007. 57:7–13.
Article24.The Korean Society of Infectious Diseases, The Korean Society for Chemotherapy, The Korean Society of Clinical Microbiology, Korean Dermatological Association. Clinical practice guidelines for soft tissue infections. Infect Chemother. 2012. 44:213–32.25.Goswami NN., Trivedi HR., Goswami AP., Patel TK., Tripathi CB. Antibiotic sensitivity profile of bacterial pathogens in postoperative wound infections at a tertiary care hospital in Gujarat, India. J Pharmacol Pharmacother. 2011. 2:158–64.
Article26.Giacometti A., Cirioni O., Schimizzi AM., Del Prete MS., Barchiesi F., D'Errico MM, et al. Epidemiology and microbiology of surgical wound infections. J Clin Microbiol. 2000. 38:918–22.
Article27.Gustafson TL., Band JD., Hutcheson RH Jr., Schaffner W. Pseudomonas folliculitis: an outbreak and review. Rev Infect Dis. 1983. 5:1–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Investigation of Causative Organisms and Resistance to Antibiotics in Urinary Tract Infection
- Changes of Bacterial Resistant Pattern in Adult Acute Epididymitis at a Tertiary Hospital in Recent Ten Years
- The Cultured Organisms and In Vitro Antibiotic Sensitivity of Ocular Bacterial Infection
- Antibiotic Sensitivity to the Causative Organism of Acute Simple Urinary Tract Infection for Recent 3 Years
- The Resistance to Ciprofloxacin in Bacterial Ocular Disease