Tuberc Respir Dis.
2008 Oct;65(4):313-317.
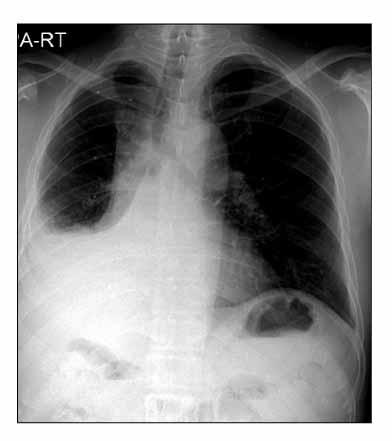
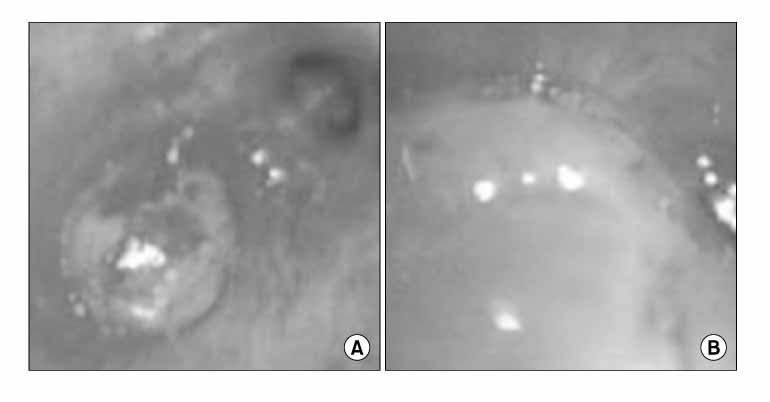
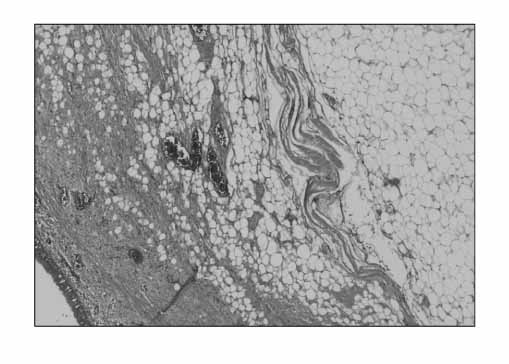
A Case of Endobronchial Lipoma Causing Right Middle and Lower Lobes Collapse and Bronchiolitis Obliterans-organizing Pneumonia
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. sekyukim@yuhs.ac
- 2The Institute of Chest Diseases, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Cardiovascular and Thoracic Surgery, Yonsei University College of Medicine, Seoul, Korea.
Abstract
- Lipoma is a common neoplasm in soft tissues. However, an intrapulmonary lipoma is a rare benign tumor. Patients with a bronchial lipoma might have a malignant potential related to their smoking history due to the case reports of lung cancer accompanied with lipoma. Endobronchial lipoma can cause irreversible parenchymal lung damage if not diagnosed and treated early. Therefore, it should initially be treated by fiberoptic bronchoscopy or surgery depending on the status of distal parenchymal lung damage. Bronchiolitis obliterans with organizing pneumonia (BOOP) is a pathological syndrome that is defined by the presence of buds of granulation tissue consisting of fibroblasts and collagen within the lumen of the distal air spaces. BOOP is caused by drug intoxication, connective tissue disease, infection, obstructive pneumonia, tumors, or an unknown etiology. We encountered a 58 year-old male patient with endobronchial lipoma, causing the collapse of the right middle and lower lobes, and BOOP due to obstructive pneumonia.
MeSH Terms
Figure
Reference
-
1. Yokozaki M, Kodama T, Yokose T, Nishimura M, Yoshida J, Mizokami H, et al. Endobronchial lipoma: a report of three cases. Jpn J Clin Oncol. 1996. 26:53–57.2. Nomori H, Horio H, Suemasu K. Two-stage operation for endobronchial lipoma and lung cancer using bronchoscopy and thoracoscopy in an elderly patient with chronic obstructive pulmonary disease. Jpn J Thorac Cardiovasc Surg. 1999. 47:567–569.3. Rokitansky C. A manual of pathological anatomy. 1854. London: Sydenham Society;196.4. Kim HJ, Wang JH, In HH, Song KH, Song JO, Song KS, et al. A case of endobronchial lipoma causing middle lobe syndrome. Tuberc Respir Dis. 1997. 44:191–196.5. Lee JM, Park JH, Baik HJ, Zo JI. A case report of endobronchial lipoma. Korean J Thorac Cardiovasc Surg. 1997. 30:116–118.6. Chung SS, Kim HJ, Byun KH, Park HS, Song JW, Cho JS, et al. A case of endobronchial lipoma causing left lung collapse. Korean J Med. 1998. 55:415–419.7. Jeong NY, Yang DG, Kim SK. Endobronchial lipoma. Diagn Treat. 2001. 21:1325–1327.8. Park CB, Cho DG, Ahn MI, Song SH, Kim CH, Yoo JY, et al. Endobronchial lipoma diagnosed by chest CT: a case report. Korean J Thorac Cardiovasc Surg. 2003. 36:39–42.9. Kim JW, Huh JG, Lee HK, Joo M, Kim SW, Ku BI, et al. Endobronchial lipomatous hamartoma removed by bronchotomy: one case report. Korean J Thorac Cardiovasc Surg. 2003. 36:870–873.10. Schlesinger C, Koss MN. The organizing pneumonias: an update and review. Curr Opin Pulm Med. 2005. 11:422–430.11. Cockcroft DW, Copland GM, Donevan RE, Gourlay RH. Endobronchial lipoma: two cases and review of the literature. Can Med Assoc J. 1976. 115:326–328.12. Box K, Kerr KM, Jeffrey RR, Douglas JG. Endobronchial lipoma associated with lobar bronchiectasis. Respir Med. 1991. 85:71–72.13. Schraufnagel DE, Morin JE, Wang NS. Endobronchial lipoma. Chest. 1979. 75:97–99.14. Politis J, Funahashi A, Gehlsen JA, DeCock D, Stengel BF, Choi H. Intrathoracic lipomas: report of three cases and review of the literature with emphasis on endobronchial lipoma. J Thorac Cardiovasc Surg. 1979. 77:550–556.15. Suzuki N, Takizawa H, Yamaguchi M, Matsuzaki G, Kiyosawa H, Dohi M, et al. A case of asymptomatic endobronchial lipoma followed for 4 years. Nihon Kyobu Shikkan Gakkai Zasshi. 1992. 30:1879–1883.16. Tomashefski JF Jr. Benign endobronchial mesenchymal tumors: their relationship to parenchymal pulmonary hamartomas. Am J Surg Pathol. 1982. 6:531–540.17. Stey CA, Vogt P, Russi EW. Endobronchial lipomatous hamartoma: a rare cause of bronchial occlusion. Chest. 1998. 113:254–255.18. Muraoka M, Oka T, Akamine S, Nagayasu T, Iseki M, Suyama N, et al. Endobronchial lipoma: review of 64 cases reported in Japan. Chest. 2003. 123:293–296.19. Mata JM, Caceres J, Ferrer J, Gomez E, Castaner F, Velayos A. Endobronchial lipoma: CT diagnosis. J Comput Assist Tomogr. 1991. 15:750–751.20. Simmers TA, Jie C, Sie B. Endobronchial lipoma posing as carcinoma. Neth J Med. 1997. 51:143–145.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of idiopathic bronchiolitis obliterans organizing pneumonia
- A case of bronchiolitis obliterans organizing pneumonia associated with wheezing
- Dermatomyositis without elevation of creatine kinase presented as bronchiolitis obliterans organizing pneumonia
- A case of bronchiolitis obliterans organizing pneumonia associated with adenovirus
- Diffuse Micronodular Pattern of Bronchiolitis Obliterans Organizing Pneumonia: A Case Report