Lab Med Online.
2012 Oct;2(4):226-231.
Mycoplasma pneumoniae Pneumonia Unresponsive to Macrolide Treatment
- Affiliations
-
- 1Department of Laboratory Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea. mnkim@amc.seoul.kr
- 2Department of Pulmonary and Critical Care Medicine, University of Ulsan College of Medicine and Asan Medical Center, Seoul, Korea.
- 3Department of Laboratory Medicine, The Catholic University of Korea School of Medicine, Seoul St. Mary's Hospital, Seoul, Korea.
Abstract
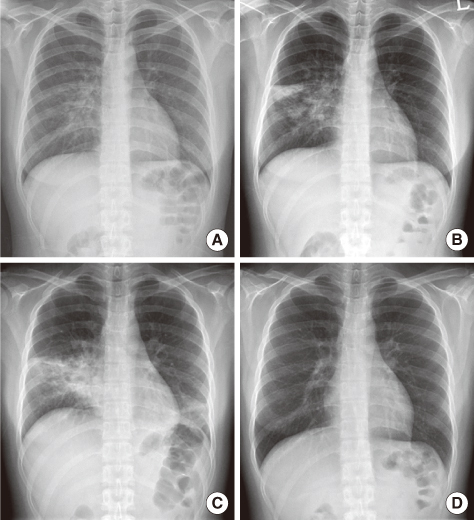
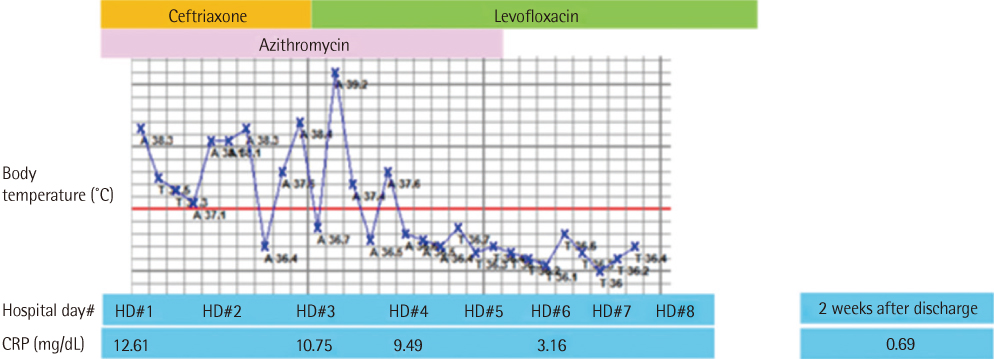
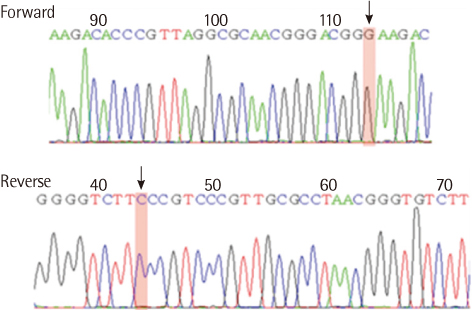
- We present a case of community-acquired pneumonia (CAP) that developed in a previously healthy young woman. She was diagnosed with Mycoplasma pneumoniae pneumonia, but did not respond to macrolide treatment. The pathogens of CAP was examined using chest radiographs, computed tomography, and various laboratory tests including Mycoplasma IgG and IgM antibodies, blood and sputum cultures, and PCR for M. pneumoniae, Legionella pneumophila, and Chlamydophila pneumoniae. In this study, differential diagnosis of the pathogens and analysis of the mechanisms underlying their resistance to macrolide treatment were performed, and the results were discussed. After changing the antimicrobial to quinolone, the patients' clinical symptoms and radiographic findings improved, and she was discharged after 8 days.
MeSH Terms
Figure
Reference
-
1. Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009. 64:Suppl 3. iii1–iii55.
Article2. Wolff BJ, Thacker WL, Schwartz SB, Winchell JM. Detection of macrolide resistance in Mycoplasma pneumoniae by real-time PCR and high-resolution melt analysis. Antimicrob Agents Chemother. 2008. 52:3542–3549.
Article3. Morozumi M, Takahashi T, Ubukata K. Macrolide-resistant Mycoplasma pneumoniae: characteristics of isolates and clinical aspects of community-acquired pneumonia. J Infect Chemother. 2010. 16:78–86.
Article4. Bebear C, Pereyre S, Peuchant O. Mycoplasma pneumoniae: susceptibility and resistance to antibiotics. Future Microbiol. 2011. 6:423–431.5. Atkinson TP, Balish MF, Waites KB. Epidemiology, clinical manifestations, pathogenesis and laboratory detection of Mycoplasma pneumoniae infections. FEMS Microbiol Rev. 2008. 32:956–973.
Article6. Daxboeck F, Krause R, Wenisch C. Laboratory diagnosis of Mycoplasma pneumoniae infection. Clin Microbiol Infect. 2003. 9:263–273.7. Nilsson AC, Björkman P, Persson K. Polymerase chain reaction is superior to serology for the diagnosis of acute Mycoplasma pneumoniae infection and reveals a high rate of persistent infection. BMC Microbiol. 2008. 8:93.
Article8. Bae SM, Jang MJ, Song HJ, Jeon DY, Kweon SS, Kang YH. Prevalence of Mycoplasma pneumoniae antibodies in healthy residents of Jeonnam Province. Korean J Clin Microbiol. 2007. 10:109–113.9. Youn YS, Lee KY. Mycoplasma pneumoniae pneumonia in children. Korean J Pediatr. 2012. 55:42–47.10. Harris M, Clark J, Coote N, Fletcher P, Harnden A, McKean M, et al. British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011. 66:Suppl 2. ii1–ii23.
Article11. Waites KB, Crabb DM, Duffy LB. In vitro activities of ABT-773 and other antimicrobials against human mycoplasmas. Antimicrob Agents Chemother. 2003. 47:39–42.
Article12. Hansen LH, Mauvais P, Douthwaite S. The macrolide-ketolide antibiotic binding site is formed by structures in domains II and V of 23S ribosomal RNA. Mol Microbiol. 1999. 31:623–631.
Article13. Poehlsgaard J, Douthwaite S. Macrolide antibiotic interaction and resistance on the bacterial ribosome. Curr Opin Investig Drugs. 2003. 4:140–148.14. Vester B, Douthwaite S. Macrolide resistance conferred by base substitutions in 23S rRNA. Antimicrob Agents Chemother. 2001. 45:1–12.
Article15. Morozumi M, Iwata S, Hasegawa K, Chiba N, Takayanagi R, Matsubara K, et al. Increased macrolide resistance of Mycoplasma pneumoniae in pediatric patients with community-acquired pneumonia. Antimicrob Agents Chemother. 2008. 52:348–350.
Article16. Bébéar CM, Pereyre S. Mechanisms of drug resistance in Mycoplasma pneumoniae. Curr Drug Targets Infect Disord. 2005. 5:263–271.17. Pereyre S, Charron A, Renaudin H, Bébéar C, Bébéar CM. First report of macrolide-resistant strains and description of a novel nucleotide sequence variation in the P1 adhesin gene in Mycoplasma pneumoniae clinical strains isolated in France over 12 years. J Clin Microbiol. 2007. 45:3534–3539.
Article18. Liu Y, Ye X, Zhang H, Xu X, Li W, Zhu D, et al. Characterization of macrolide resistance in Mycoplasma pneumoniae isolated from children in Shanghai, China. Diagn Microbiol Infect Dis. 2010. 67:355–358.
Article19. Xin D, Mi Z, Han X, Qin L, Li J, Wei T, et al. Molecular mechanisms of macrolide resistance in clinical isolates of Mycoplasma pneumoniae from China. Antimicrob Agents Chemother. 2009. 53:2158–2159.
Article20. Oh CE, Choi EH, Lee HJ. Detection of genetic mutations associated with macrolide resistance of Mycoplasma pneumoniae. Korean J Pediatr. 2010. 53:178–183.
Article21. Chang MW, Kim KH, Park ID, Song GY, Kim SW, Lee EY. Isolation of Mycoplasma pneumoniae and antimicrobial susceptibilities of the Isolates (III). J Life Sci. 2005. 15:479–485.
Article22. Kim SW. Antibiotic resistance and treatment update of community-acquired pneumonia. Korean J Med. 2011. 81:690–698.23. Tamura A, Matsubara K, Tanaka T, Nigami H, Yura K, Fukaya T. Methylprednisolone pulse therapy for refractory Mycoplasma pneumoniae pneumonia in children. J Infect. 2008. 57:223–228.
Article24. Miyashita N, Obase Y, Ouchi K, Kawasaki K, Kawai Y, Kobashi Y, et al. Clinical features of severe Mycoplasma pneumoniae pneumonia in adults admitted to an intensive care unit. J Med Microbiol. 2007. 56:1625–1629.
Article25. Kim DH, Lee KY, Kim MS, Youn YS, Hwang JY, Rhim JW, et al. Corticosteroid treatment in siblings affected with severe Mycoplasma pneumoniae pneumonia. Infect Chemother. 2009. 41:190–195.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Macrolide-refractory Mycoplasma pneumoniae pneumonia and hemophagocytic lymphohistiocytosis: case report and literature review
- Therapeutic Efficacy and Safety of Prolonged Macrolide, Corticosteroid, Doxycycline, and Levofloxacin against Macrolide-Unresponsive Mycoplasma pneumoniae Pneumonia in Children
- Comparison of the characteristics of macrolide-sensitive and macrolide-resistant Mycoplasma pneumoniae pneumonia requiring hospitalization in children
- Clinical issues regarding increased macrolide-resistant Mycoplasma pneumoniae in children
- Mycoplasma Pneumoniae-Associated Necrotizing Pneumonia in Children: a case-report