Diabetes Metab J.
2016 Jun;40(3):175-181. 10.4093/dmj.2016.40.3.175.
Are We in the Same Risk of Diabetes Mellitus? Gender- and Age-Specific Epidemiology of Diabetes in 2001 to 2014 in the Korean Population
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. mkmoon@snu.ac.kr
- 2Department of Internal Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2308624
- DOI: http://doi.org/10.4093/dmj.2016.40.3.175
Abstract
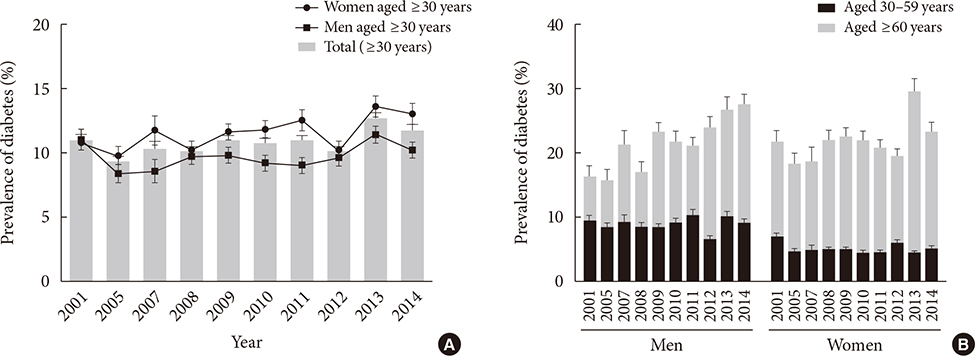
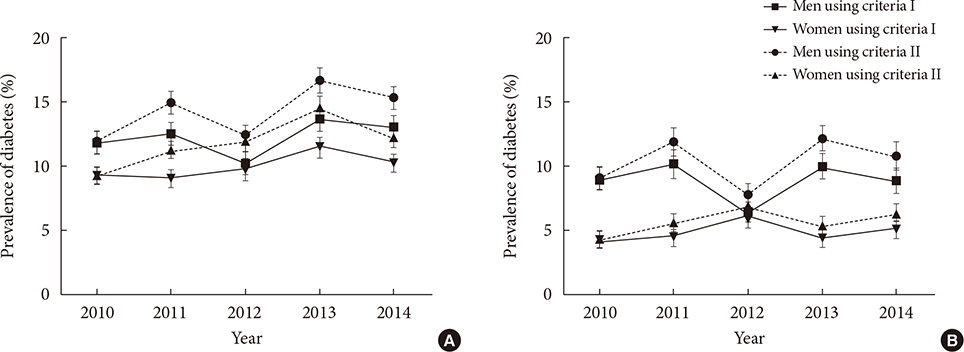
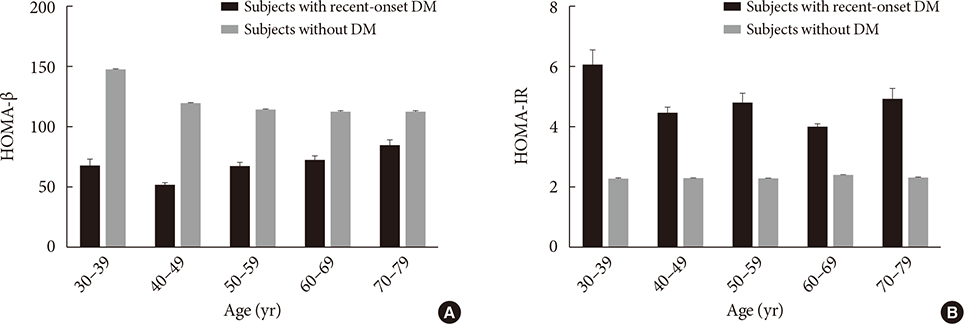
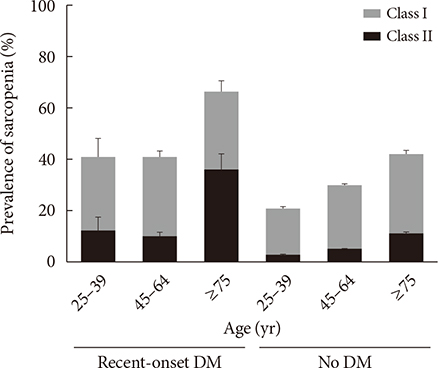
- In the early 2000s, the prevalence of diabetes in adults aged ≥30 years in Korea was about 9% to 10%, and it remained stable. However, a nationwide survey showed that this prevalence increased over the past few years. After age-standardization using the Korean population of the year 2010, the prevalence of diabetes in adults aged ≥30 years was 10.0% to 10.8% between 2001 and 2012, which increased to 12.5% in 2013 and 11.6% in 2014. During that period, there have been changes in the gender- and age-specific prevalence of diabetes in Korean adults. The prevalence of diabetes in the elderly population increased significantly, while this prevalence in young adults, especially in young women, did not change significantly. The contribution of each diabetic risk factor, such as obesity, β-cell dysfunction, sarcopenia, and socioeconomic status, in developing diabetes has also changed during that period in each gender and age group. For young women, obesity was the most important risk factor; by contrast, for elderly diabetic patients, sarcopenia was more important than obesity as a risk factor. Considering the economic burden of diabetes and its associated comorbidities, a public health policy targeting the major risk factors in each population might be more effective in preventing diabetes.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Serum Betatrophin Concentrations and the Risk of Incident Diabetes: A Nested Case-Control Study from Chungju Metabolic Disease Cohort
Seung-Hwan Lee, Marie Rhee, Hyuk-Sang Kwon, Yong-Moon Park, Kun-Ho Yoon
Diabetes Metab J. 2018;42(1):53-62. doi: 10.4093/dmj.2018.42.1.53.
Reference
-
1. International Diabetes Federation. Diabetes atlas. Brussels: International Diabetes Federation;2000.2. International Diabetes Federation. IDF diabetes atlas. 4th ed. Brussels: International Diabetes Federation;2009.3. Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011; 94:311–321.4. Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011; 35:303–308.5. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009; 32:2016–2020.6. Korean Centers for Disease Control and Prevention. Korea health statistics 2014: Korea National Health and Nutrition Examination Survey (KNHANES VI-2). Cheongju: Korean Centers for Disease Control and Prevention;2015.7. Statistics Korea. Population projections for Korea: 2010-2040. Daejeon: Statistics Korea;2011.8. Koo BK, Lee CH, Yang BR, Hwang SS, Choi NK. The incidence and prevalence of diabetes mellitus and related atherosclerotic complications in Korea: a National Health Insurance Database Study. PLoS One. 2014; 9:e110650.9. Koo BK, Kim EK, Choi H, Park KS, Moon MK. Decreasing trends of the prevalence of diabetes and obesity in Korean women aged 30-59 years over the past decade: results from the Korean National Health and Nutrition Examination Survey, 2001-2010. Diabetes Care. 2013; 36:e95–e96.10. Rhee SY, Park SW, Kim DJ, Woo J. Gender disparity in the secular trends for obesity prevalence in Korea: analyses based on the KNHANES 1998-2009. Korean J Intern Med. 2013; 28:29–34.11. Korean Diabetes Association. Treatment guideline for diabetes. Seoul: Korean Diabetes Association;2011.12. Jeon JY, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, Song KH, Won JC, Lim S, Choi SH, Jang MJ, Kim Y, Oh K, Kim DJ, Cha BY. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Prevalence of diabetes and prediabetes according to fasting plasma glucose and HbA1c. Diabetes Metab J. 2013; 37:349–357.13. Charvat H, Goto A, Goto M, Inoue M, Heianza Y, Arase Y, Sone H, Nakagami T, Song X, Qiao Q, Tuomilehto J, Tsugane S, Noda M, Inoue M. Impact of population aging on trends in diabetes prevalence: a meta-regression analysis of 160,000 Japanese adults. J Diabetes Investig. 2015; 6:533–542.14. Xi B, Liang Y, He T, Reilly KH, Hu Y, Wang Q, Yan Y, Mi J. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993-2009. Obes Rev. 2012; 13:287–296.15. Lee YH, Armstrong EJ, Kim G, Oh J, Kang SM, Lee BW, Ahn CW, Cha BS, Lee HC, Mantzoros CS, Kang ES. Undiagnosed diabetes is prevalent in younger adults and associated with a higher risk cardiometabolic profile compared to diagnosed diabetes. Am Heart J. 2015; 170:760–769.e2.16. Korean Diabetes Association. Korea Centers for Disease Control and Prevention: Diabetes fact sheet in Korea 2012. updated 2012 Nov 13. Available from: http://www.diabetes.or.kr/temp/Diabetes_Fact_sheet2012.pdf.17. Kim CS, Ko SH, Kwon HS, Kim NH, Kim JH, Lim S, Choi SH, Song KH, Won JC, Kim DJ, Cha BY. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Prevalence, awareness, and management of obesity in Korea: data from the Korea national health and nutrition examination survey (1998-2011). Diabetes Metab J. 2014; 38:35–43.18. Koo BK, Kim SW, Yi KH, Park KS, Moon MK. Changing relative contribution of abdominal obesity and a family history of diabetes on prevalence of diabetes mellitus in Korean men and women aged 30-49 years from 2001 to 2010. J Diabetes. 2015; 7:465–472.19. Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001; 345:790–797.20. Tatsumi Y, Ohno Y, Morimoto A, Nishigaki Y, Mizuno S, Watanabe S. Age differences in the risk of diabetes incidence according to body mass index level in Japanese women. Obes Res Clin Pract. 2013; 7:e455–e463.21. Meigs JB, Wilson PW, Fox CS, Vasan RS, Nathan DM, Sullivan LM, D'Agostino RB. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab. 2006; 91:2906–2912.22. Ohn JH, Kwak SH, Cho YM, Lim S, Jang HC, Park KS, Cho NH. 10-Year trajectory of beta-cell function and insulin sensitivity in the development of type 2 diabetes: a community-based prospective cohort study. Lancet Diabetes Endocrinol. 2016; 4:27–34.23. Morimoto A, Tatsumi Y, Deura K, Mizuno S, Ohno Y, Miyamatsu N, Watanabe S. Impact of impaired insulin secretion and insulin resistance on the incidence of type 2 diabetes mellitus in a Japanese population: the Saku study. Diabetologia. 2013; 56:1671–1679.24. Festa A, Williams K, D'Agostino R Jr, Wagenknecht LE, Haffner SM. The natural course of beta-cell function in nondiabetic and diabetic individuals: the Insulin Resistance Atherosclerosis Study. Diabetes. 2006; 55:1114–1120.25. Park KS. The search for genetic risk factors of type 2 diabetes mellitus. Diabetes Metab J. 2011; 35:12–22.26. Mohan V, Amutha A, Ranjani H, Unnikrishnan R, Datta M, Anjana RM, Staimez L, Ali MK, Narayan KM. Associations of beta-cell function and insulin resistance with youth-onset type 2 diabetes and prediabetes among Asian Indians. Diabetes Technol Ther. 2013; 15:315–322.27. Koo BK, Roh E, Yang YS, Moon MK. Difference between old and young adults in contribution of beta-cell function and sarcopenia in developing diabetes mellitus. J Diabetes Investig. 2016; 7:233–240.28. de Miguel-Yanes JM, Shrader P, Pencina MJ, Fox CS, Manning AK, Grant RW, Dupuis J, Florez JC, D'Agostino RB Sr, Cupples LA, Meigs JB. MAGIC Investigators. DIAGRAM+ Investigators. Genetic risk reclassification for type 2 diabetes by age below or above 50 years using 40 type 2 diabetes risk single nucleotide polymorphisms. Diabetes Care. 2011; 34:121–125.29. Wong J, Molyneaux L, Zhao D, Constantino M, Gray RS, Twigg SM, Xu ZR, Yue DK. Different accelerators to early-onset type 2 diabetes: a comparison of Anglo-Celtic and Chinese patients. J Diabetes Complications. 2008; 22:389–394.30. Robbins JM, Vaccarino V, Zhang H, Kasl SV. Socioeconomic status and type 2 diabetes in African American and non-Hispanic white women and men: evidence from the Third National Health and Nutrition Examination Survey. Am J Public Health. 2001; 91:76–83.31. Rabi DM, Edwards AL, Southern DA, Svenson LW, Sargious PM, Norton P, Larsen ET, Ghali WA. Association of socio-economic status with diabetes prevalence and utilization of diabetes care services. BMC Health Serv Res. 2006; 6:124.32. Kim SH. International statistics yearbook. Daejeon: Statistics Korea;2011.33. Koo BK, Kim SW, Yi KH, Moon MK. Low economic status is identified as an emerging risk factor for diabetes mellitus in Korean men aged 30 to 59 years in Korean National Health and Nutrition Examination Survey 2008 to 2010. Diabetes Metab J. 2015; 39:137–146.34. Hwang J, Shon C. Relationship between socioeconomic status and type 2 diabetes: results from Korea National Health and Nutrition Examination Survey (KNHANES) 2010-2012. BMJ Open. 2014; 4:e005710.35. Kim SR, Han K, Choi JY, Ersek J, Liu J, Jo SJ, Lee KS, Yim HW, Lee WC, Park YG, Lee SH, Park YM. Age- and sex-specific relationships between household income, education, and diabetes mellitus in Korean adults: the Korea National Health and Nutrition Examination Survey, 2008-2010. PLoS One. 2015; 10:e0117034.36. Ning F, Pang ZC, Dong YH, Gao WG, Nan HR, Wang SJ, Zhang L, Ren J, Tuomilehto J, Hammar N, Malmberg K, Andersson SW, Qiao Q. Qingdao Diabetes Survey Group. Risk factors associated with the dramatic increase in the prevalence of diabetes in the adult Chinese population in Qingdao, China. Diabet Med. 2009; 26:855–863.37. Deepa M, Anjana RM, Manjula D, Narayan KM, Mohan V. Convergence of prevalence rates of diabetes and cardiometabolic risk factors in middle and low income groups in urban India: 10-year follow-up of the Chennai Urban Population Study. J Diabetes Sci Technol. 2011; 5:918–927.38. Caiazzo A, Cardano M, Cois E, Costa G, Marinacci C, Spadea T, Vannoni F, Venturini L. Inequalities in health in Italy. Epidemiol Prev. 2004; 28:3 Suppl. i–ix. 1–161.39. van Lenthe FJ, Schrijvers CT, Droomers M, Joung IM, Louwman MJ, Mackenbach JP. Investigating explanations of socio-economic inequalities in health: the Dutch GLOBE study. Eur J Public Health. 2004; 14:63–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter: Genome-Wide Association Study Identifies Two Novel Loci with Sex-Specific Effects for Type 2 Diabetes Mellitus and Glycemic Traits in a Korean Population (Diabetes Metab J 2014;38:375-87)
- Epidemiology of Peripheral Arterial Diseases in Individuals with Diabetes Mellitus
- Response: Genome-Wide Association Study Identifies Two Novel Loci with Sex-Specific Effects for Type 2 Diabetes Mellitus and Glycemic Traits in a Korean Population (Diabetes Metab J 2014;38:375-87)
- The Epidemiology of Diabetes in Korea
- Prevention of Diabetes Mellitus: Including Review of Finnish Diabetes Prevention Study and Diabetes Prevention Program