Korean Circ J.
2011 May;41(5):280-282. 10.4070/kcj.2011.41.5.280.
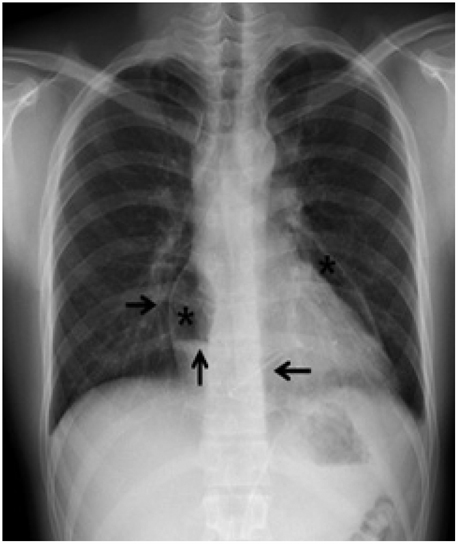
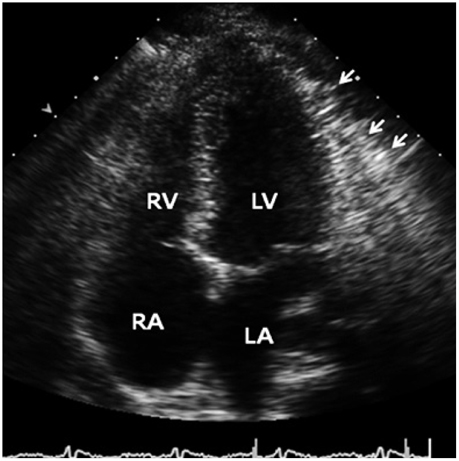
Pneumopericardium as a Complication of Pericardiocentesis
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. medsws@catholic.ac.kr
- KMID: 2297937
- DOI: http://doi.org/10.4070/kcj.2011.41.5.280
Abstract
- Pneumopericardium is a rare complication of pericardiocentesis, occurring either as a result of direct pleuro-pericardial communication or a leaky drainage system. Air-fluid level surrounding the heart shadow within the pericardium on a chest X-ray is an early observation at diagnosis. This clinical measurement and process is variable, depending on the hemodynamic status of the patient. The development of a cardiac tamponade is a serious complication, necessitating prompt recognition and treatment. We recently observed a case of pneumopericardium after a therapeutic pericardiocentesis in a 20-year-old man with tuberculous pericardial effusion.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Spontaneous Pneumomediastinum, Pneumopericardium, and Pneumothorax with Respiratory Failure in a Patient with AIDS and Pneumocystis jirovecii Pneumonia
Yun Kyung Park, Hee Chan Jung, Shin Young Kim, Min Young Kim, Kwanhoon Jo, Se Young Kim, Borami Kang, Gihyeon Woo, Hyun Joo Choi, Seong-Heon Wie
Infect Chemother. 2014;46(3):204-208. doi: 10.3947/ic.2014.46.3.204.
Reference
-
1. Lee YJ, Jin SW, Jang SH, et al. A case of spontaneous pneumomediastinum and pneumopericardium in a young adult. Korean J Intern Med. 2001. 16:205–209.2. Brander L, Ramsay D, Dreier D, Peter M, Graeni R. Continuous left hemidiaphragm sign revisited: a case of spontaneous pneumopericardium and literature review. Heart. 2002. 88:e5.3. Arroyo M, Soberman JE. Adenosine deaminase in the diagnosis of tuberculous pericardial effusion. Am J Med Sci. 2008. 335:227–229.4. Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation. 2005. 112:3608–3616.5. Park WH, Jun JE, Park MH. Echocardiographic observation in 50 cases of pericardial effusion. Korean Circ J. 1982. 12:135–143.6. Buchanan CL, Sullivan VV, Lampman R, Kulkarni MG. Pericardiocentesis with extended catheter drainage: an effective therapy. Ann Thorac Surg. 2003. 76:817–820.7. Naunheim KS, Kesler KA, Fiore AC, et al. Pericardial drainage: subxiphoid vs. transthoracic approach. Eur J Cardiothorac Surg. 1991. 5:99–103.