Korean Circ J.
2011 Oct;41(10):578-582. 10.4070/kcj.2011.41.10.578.
Optimal Antithrombotic Strategy in Patients With Atrial Fibrillation After Coronary Stent Implantation
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, The Catholic University of Korea School of Medicine, Seoul, Korea. tairho@catholic.ac.kr
- KMID: 2297916
- DOI: http://doi.org/10.4070/kcj.2011.41.10.578
Abstract
- BACKGROUND AND OBJECTIVES
Little evidence is available on the optimal antithrombotic therapy following percutaneous coronary intervention (PCI) in patients with atrial fibrillation (AF). We investigated the outcomes of antithrombotic treatment strategies in AF patients who underwent PCI.
SUBJECTS AND METHODS
Three hundred sixty-two patients (68.0% men, mean age: 68.3+/-7.8 years) with AF and who had undergone PCI with stent implantation between 2005 and 2007 were enrolled. The clinical, demographic and procedural characteristics were reviewed and the stroke risk factors as well as antithrombotic regimens were analyzed.
RESULTS
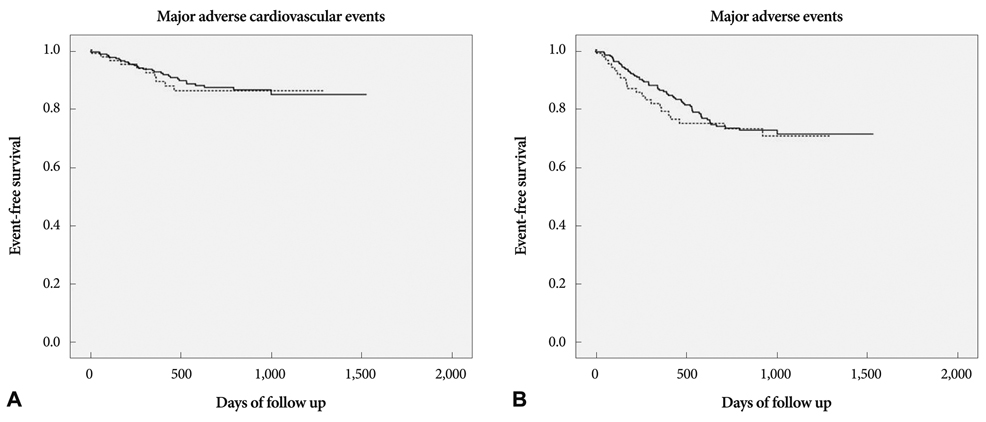
The accompanying comorbidities were as follows: hypertension (59.4%), diabetes (37.3%) and congestive heart failure (16.6%). The average number of stroke risk factors was 1.6. At the time of discharge after PCI, warfarin was prescribed for 84 patients (23.2%). Cilostazol was used in addition to dual antiplatelet therapy in 35% of the patients who did not receive warfarin. The mean follow-up period was 615+/-385 days. The incidences of major adverse cardiac events (MACE), stroke and major bleeding were 11.3%, 3.6% and 4.1%, respectively. By Kaplan-Meier survival analysis, warfarin treatment was not associated with a lower risk of MACE (p=0.886), but it was associated with an increased risk of major bleeding (p=0.002).
CONCLUSION
Oral anticoagulation therapy after PCI may increase hemorrhagic events in Korean AF patients.
MeSH Terms
Figure
Cited by 1 articles
-
Diagnosis and management of acute coronary syndrome
Doo Soo Jeon
J Korean Med Assoc. 2017;60(7):568-576. doi: 10.5124/jkma.2017.60.7.568.
Reference
-
1. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation-executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation). J Am Coll Cardiol. 2006. 48:854–906.2. van Walraven C, Hart RG, Singer DE, et al. Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis. JAMA. 2002. 288:2441–2448.3. Aguilar MI, Hart R, Pearce LA. Oral anticoagulants versus antiplatelet therapy for preventing stroke in patients with non-valvular atrial fibrillation and no history of stroke or transient ischemic attacks. Cochrane Database Syst Rev. 2007. CD006186.4. Lip GY, Karpha M. Anticoagulant and antiplatelet therapy use in patients with atrial fibrillation undergoing percutaneous coronary intervention: the need for consensus and a management guideline. Chest. 2006. 130:1823–1827.5. Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001. 285:2864–2870.6. Ruiz-Nodar JM, Marin F, Hurtado JA, et al. Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation implications for bleeding risk and prognosis. J Am Coll Cardiol. 2008. 51:818–825.7. Lee SW, Park SW, Kim YH, et al. Comparison of triple versus dual antiplatelet therapy after drug-eluting stent implantation (from the DECLARE-Long trial). Am J Cardiol. 2007. 100:1103–1108.8. Han Y, Li Y, Wang S, et al. Cilostazol in addition to aspirin and clopidogrel improves long-term outcomes after percutaneous coronary intervention in patients with acute coronary syndromes: a randomized, controlled study. Am Heart J. 2009. 157:733–739.9. Yang TH, Kim DI, Kim JY, et al. Comparison of triple anti-platelet therapy (aspirin, clopidogrel, and cilostazol) and double anti-platelet therapy (aspirin and clopidogrel) on platelet aggregation in type 2 diabetic patients undergoing drug-eluting stent implantation. Korean Circ J. 2009. 39:462–466.10. Connolly S, Pogue J, Hart R, et al. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial. Lancet. 2006. 367:1903–1912.11. Connolly SJ, Pogue J, Eikelboom J, et al. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation. 2008. 118:2029–2037.12. Sorensen R, Hansen ML, Abildstrom SZ, et al. Risk of bleeding in patients with acute myocardial infarction treated with different combinations of aspirin, clopidogrel, and vitamin K antagonists in Denmark: a retrospective analysis of nationwide registry data. Lancet. 2009. 374:1967–1974.13. Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol. 2007. 50:309–315.14. Suzuki S, Yamashita T, Kato T, et al. Incidence of major bleeding complication of warfarin therapy in Japanese patients with atrial fibrillation. Circ J. 2007. 71:761–765.15. Higashi MK, Veenstra DL, Kondo LM, et al. Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA. 2002. 287:1690–1698.16. Li T, Lange LA, Li X, et al. Polymorphisms in the VKORC1 gene are strongly associated with warfarin dosage requirements in patients receiving anticoagulation. J Med Genet. 2006. 43:740–744.17. Rieder MJ, Reiner AP, Gage BF, et al. Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose. N Engl J Med. 2005. 352:2285–2293.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antithrombotic Strategy in Atrial Fibrillation Patients Undergoing Percutaneous Coronary Intervention
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- Pathophysiology and Diagnosis in Atrial Fibrillation
- A Case of Paroxysmal Atrial Fibrillation and Sinus Bradycardia due to Coronary Artery Spasm
- Antithrombotic Therapy for Patients with Nonvalvular Atrial Fibrillation