Korean J Urol.
2006 Jan;47(1):42-46. 10.4111/kju.2006.47.1.42.
The Recurrence of Chronic Pelvic Pain Syndrome and the Role of Uro-Vaxom(R)
- Affiliations
-
- 1Department of Urology, College of Medicine, Ewha Womans University, Seoul, Korea. bonstone@ewha.ac.kr
- KMID: 2294214
- DOI: http://doi.org/10.4111/kju.2006.47.1.42
Abstract
-
PURPOSE: Chronic pelvic pain syndrome (CPPS) is the most common urogenital disease in middle aged men, and it shows various symptoms and a high recurrent rate. Uro-Vaxom(R) is effective for the treatment of urinary tract infection via the activation of the urothelial immune system. The main objectives of this study were to investigate the recurrence of CPPS and to find out if Uro-Vaxom(R) is helpful to suppress the recurrence of this condition.
MATERIALS AND METHODS
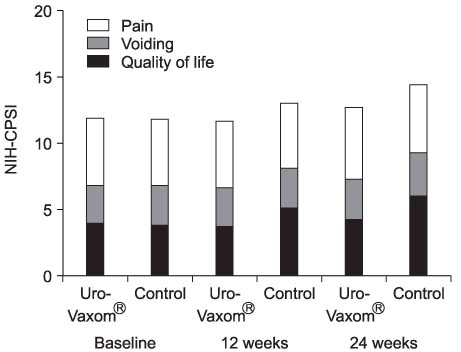
After completing treatment for CPPS (NIH-IIIa 45, NIH-IIIb 85), 130 patients were given a 12 week course of Uro-Vaxom(R) 60mg once a day before breakfast. Sixty patients were also included in the study as a control group after they completed the treatment for CPPS (NIH-IIIa 22, NIH-IIIb 38). All of patients were reevaluated 12 weeks and 24 weeks later with the NIH-CPSI criteria and the EPS findings.
RESULTS
The overall recurrent rate for NIH-IIIa disease was 22.7%, and it was 26.3% for the patients with NIH-IIIb disease in the control group, and it was 6.7% for the patients with NIH-IIIa disease and 7.1% for the patients with NIH-IIIb disease in the Uro-Vaxom(R) group (p<0.05). The classification of the recurrent CPPS was 46.7% NIH-IIIa and 53.3% NIH- IIIb in the control group, and 11.1% NIH-IIIa and 88.9% NIH-IIIb in the Uro-Vaxom(R) group. The possible predisposing factors related to the recurrence of CPPS were excessive alcoholic drinking (29.2%), overwork (25.0%) and stress (16.7%). In the non-recurrent patients, there was no change of the NIH-Chronic Prostatitis Symptom Index and the EPS findings for all patients during the follow-up period.
CONCLUSIONS
There was about a 30% recurrence rate of CPPS within 6 months after treatment, and Uro-Vaxom(R) may play a significant role to suppress the recurrence of CPPS.
Keyword
MeSH Terms
Figure
Reference
-
1. Collins MM, Stafford RS, O'Leary MP, Barry MJ. Distinguishing chronic prostatitis and benign prostatic hyperplasia symptoms: results of a national survey of physician visits. Urology. 1999. 53:921–925.2. Nickel JC, Nyberg LM, Hennenfent M. Research guidelines for chronic prostatitis: consensus report from the first National Institutes of Health International Prostatitis Collaborative Network. Urology. 1999. 54:229–233.3. Bosch A, Benedi VJ, Pares R, Jofre J. Enhancement of the humoral immune response and resistance to bacterial infection in mice by the oral administration of a bacterial immunomodulator (OM-89). Immunopharmacol Immunotoxicol. 1988. 10:333–343.4. Tammen H. The German Urinary Tract Infection Study Group. Immunobiotherapy with Uro-Vaxom in recurrent urinary tract infection. Br J Urol. 1990. 65:6–9.5. Chong CH, Ryu DS, Oh TH. The Korean version of NIH-Chronic Prostatitis Symptom Index (NIH-CPSI): validation study and characteristics on chronic prostatitis. Korean J Urol. 2001. 42:511–521.6. von Lackum WH. Clinical and experimental data on prostatic infection. J Urol. 1927. 18:293–306.7. Campbell MF. Campbell MF, editor. The male reproductive tract: the prostate. Principles of urology: an introductory text to the disease of the urological tract. 1957. Philadelphia: WB Saunders;311–313.8. Collins MM, Stafford RS, O'Leary MP, Barry MJ. How common is prostatitis? A national survey of physician visits. J Urol. 1998. 159:1224–1228.9. Roberts RO, Lieber MM, Rhodes T, Girman CJ, Bostwick DG, Jacobsen SJ. Prevalence of a physician-assigned diagnosis of prostatitis: the Olmsted County Study of Urinary Symptoms and Health Status Among Men. Urology. 1998. 51:578–584.10. Mehik A, Hellstrom P, Lukkarinen O, Sarpola A, Jarvelin M. Epidemiology of prostatitis in Finnish men: a population-based cross-sectional study. BJU Int. 2000. 86:443–448.11. Ku JH, Lee NK, Park YH. The analysis of chronic prostatitis symptom score surveyed in 19 year old Korean men in the area of Teajeon and Chungnam. Korean J Urol. 2001. 42:85–92.12. Nickel JC. Walsh PC, Retik AB, Vaughan ED, Wein AJ, editors. Prostatitis and related conditions. Campbell's urology. 2002. 8th ed. Philadelphia: Saunders;604–606.13. Batstone GR, Doble A, Batstone D. Chronic prostatitis. Curr Opin Urol. 2003. 13:23–29.14. Nickel JC, Costerton JW, McLean RJ, Olson M. Bacterial biofilms: influence on the pathogenesis, diagnosis and treatment of urinary tract infections. J Antimicrob Chemother. 1994. 33:Suppl A. 31–41.15. Fair WR, Couch J, Wehner N. Prostatic antibacterial factor: identity and significance. Urology. 1976. 7:169–177.16. Kirby R, Lowe D, Bultitude MI, Shuttleworth KE. Intraprostatic urinary reflux: an aetiological factor in abacterial prostatitis. Br J Urol. 1982. 54:729–731.17. Kim YS, Choi YD, Kang KH, Ryu RH, Choi HK, Park HS, et al. Study of prostatic disease and symptom between special occupation groups (taxi driver, barber). Korean J Urol. 1998. 39:1093–1097.18. Alexander RB, Trissel D. Chronic prostatitis: results of an internet survey. Urology. 1996. 48:568–574.19. Koroku M, Kumamoto Y, Hirose T. A study on the role of Chlamydia trachomatis in chronic prostatitis--analysis of anti-Chlamydia trachomatis specific IgA in expressed prostate secretion by western-blotting method. Kansenshogaku Zasshi. 1995. 69:426–437.20. Bottex C, Boyer G, Fontangews R. Efficacy of an immunomodulator in compensating antibiotic-induced immunosuppression. Int J Immunopathol Pharmacol. 1989. 2:41–44.21. Fliedner M, Mehls O, Rauterberg EW, Ritz E. Urinary sIgA in children with urinary tract infection. J Pediatr. 1986. 109:416–421.22. Hachen HJ. Oral immunotherapy in paraplegic patients with chronic urinary tract infections: a double-blind, placebo-controlled trial. J Urol. 1990. 143:759–762.23. Leskinen M, Lukkarinen O, Marttila T. Effects of finasteride in patients with inflammatory chronic pelvic pain syndrome: a double-blind, placebo-controlled, pilot study. Urology. 1999. 53:502–505.24. Lee KC, Choi H, Park HS, Kim JJ, Moon DG. Therapeutic efficacy of extracorporeal magnetic therapy in chronic pelvic pain syndrome. Korean J Urol. 2003. 44:693–696.25. Litwin MS, McNaughton-Collins M, Fowler FJ Jr, Nickel JC, Calhoun EA, Pontari MA, et al. The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure. J Urol. 1999. 162:369–375.26. Benoit G, Merlud L, Meduri G, Moukarzel M, Quilard J, Ledroux M, et al. Anatomy of the prostatic nerves. Surg Radiol Anat. 1994. 16:23–29.27. Krieger JN, Egan KJ, Ross SO, Jacobs R, Berger RE. Chronic pelvic pains represent the most prominent urogenital symptoms of "chronic prostatitis". Urology. 1996. 48:715–722.28. Kim SW, Ha JS, Lee SJ, Cho YH, Yoon MS. Clinical effect of tamsulosin in noninflammatory chronic pelvic pain syndrome. Korean J Urol. 2003. 44:120–123.29. Blacklock NJ. Anatomical factors in prostatitis. Br J Urol. 1974. 46:47–54.30. Schaeffer AJ. Classification (traditional and National Institutes of Health) and demographics of prostatitis. Urology. 2002. 60:5–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Application of Uro-vaxom(R), Urinary Tract Immunostimulator in the Treatment of Chronic Pelvic Pain Syndrome
- The Clinical Efficacy of Uro-Vaxom(R)in the Treatment of Recurrent Urinary Tract Infections
- Efficacy and Safety of Uro-Vaxom Treatment for Patients with Recurrent Cystitis: An Open Multicenter Study
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome: What Are the Starting and Worsening Factors?
- Neuropathic Pain in Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)