Korean J Schizophr Res.
2012 Oct;15(2):106-113. 10.16946/kjsr.2012.15.2.106.
Attitude Toward Antipsychotic Treatment According to Patients' Awareness of the Name of Their Illness in Patients with Schizophrenia
- Affiliations
-
- 1Department of Psychiatry, Chonnam National University Medical School, Gwangju, Korea. swkim@chonnam.ac.kr
- 2Gwang-ju Bukgu Community Mental Health Center, Gwangju, Korea.
- 3Department of Psychiatry, St. John Hospital, Gwangju, Korea.
- KMID: 2288287
- DOI: http://doi.org/10.16946/kjsr.2012.15.2.106
Abstract
OBJECTIVES
This study compared attitudes toward antipsychotic treatment according to awareness of the name of their illness in patients with schizophrenia.
METHODS
Information on sociodemographic and clinical characteristics, including awareness of the importance of antipsychotic treatment, was obtained through a self-report questionnaire. The Drug Attitude Inventory (DAI) was administered. The data were compared according to awareness of the name of their illness.
RESULTS
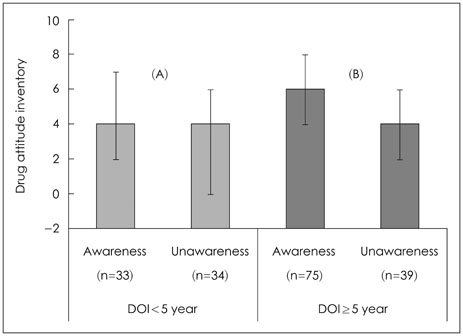
The study analyzed data for 199 patients with schizophrenia. Of these, 115 patients (57.8%) were aware that their illness was called schizophrenia, while 84 patients (42.2%) knew it by their psychotic symptoms or as another mental illness, such as depression. The patients aware of the name of their illness had significantly longer durations of illness and higher scores on the DAI. They were significantly more likely to have stopped taking medication on their own accord and to agree with the importance of antipsychotic treatment. Statistical significance was sustained in a logistic regression analysis after adjusting for the duration of illness and study site, except for the DAI score, which had borderline significance (p=0.055). In subjects with duration of illness > or =5 years, patients aware of the name of their illness had significantly higher scores on the DAI.
CONCLUSION
Awareness of the name of their illness was associated with awareness of the importance of, and a positive attitude toward, antipsychotic treatments in patients. Psycho-education, including telling the patient the correct name of his or her illness, might be needed for maintaining antipsychotic treatment in patients with chronic schizophrenia.
MeSH Terms
Figure
Reference
-
1. Kane JM. Schizophrenia. N Engl J Med. 1996. 334:34–41.
Article2. Davis JM. Overview: maintenance therapy in psychiatry: I. Schizophrenia. Am J Psychiatry. 1975. 132:1237–1245.
Article3. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005. 353:1209–1223.
Article4. Kissling W. Compliance, quality assurance and standards for relapse prevention in schizophrenia. Acta Psychiatr Scand Suppl. 1994. 382:16–24.
Article5. Coldham EL, Addington J, Addington D. Medication adherence of individuals with a first episode of psychosis. Acta Psychiatr Scand. 2002. 106:286–290.
Article6. Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002. 63:892–909.
Article7. Valenstein M, Ganoczy D, McCarthy JF, Myra Kim H, Lee TA, Blow FC. Antipsychotic adherence over time among patients receiving treatment for schizophrenia: a retrospective review. J Clin Psychiatry. 2006. 67:1542–1550.
Article8. Zygmunt A, Olfson M, Boyer CA, Mechanic D. Interventions to improve medication adherence in schizophrenia. Am J Psychiatry. 2002. 159:1653–1664.
Article9. You JH, Woo YS, Hahn C, Choi JW, Ko HJ. Predicting Factors Associated with Drug Compliance in Psychiatric Outpatients of a University Hospital. Korean J Psychopharmacol. 2010. 21:29–34.10. Kwon JS, Shin SW, Cheong YM, Park KH. Medication Compliance in Psychiatric Outpatients of a University Hospital. J Korean Neuropsychiatr Assoc. 1997. 36:523–529.11. Kim SW, Yoon JS, Choi SK. Survey of medication adherence in patients with schizophrenia-Korean ADHES data. Hum Psychopharmacol. 2006. 21:533–537.
Article12. Ascher-Svanum H, Faries DE, Zhu B, Ernst FR, Swartz MS, Swanson JW. Medication adherence and long-term functional outcomes in the treatment of schizophrenia in usual care. J Clin Psychiatry. 2006. 67:453–460.
Article13. Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res. 2010. 176:109–113.
Article14. Dutta R, Murray RM, Allardyce J, Jones PB, Boydell J. Early risk factors for suicide in an epidemiological first episode psychosis cohort. Schizophr Res. 2011. 126:11–19.
Article15. Linden M, Godemann F. The differentiation between 'lack of insight' and 'dysfunctional health beliefs' in schizophrenia. Psychopathology. 2007. 40:236–241.
Article16. Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM. Assessment of insight in psychosis. Am J Psychiatry. 1993. 150:873–879.
Article17. Kampman O, Laippala P, Väänänen J, Koivisto E, Kiviniemi P, Kilkku N, et al. Indicators of medication compliance in first-episode psychosis. Psychiatry Res. 2002. 110:39–48.
Article18. David AS. Insight and psychosis. Br J Psychiatry. 1990. 156:798–808.
Article19. Yen CF, Chen CS, Ko CH, Yeh ML, Yang SJ, Yen JY, et al. Relationships between insight and medication adherence in outpatients with schizophrenia and bipolar disorder: prospective study. Psychiatry Clin Neurosci. 2005. 59:403–409.
Article20. Day JC, Bentall RP, Roberts C, Randall F, Rogers A, Cattell D, et al. Attitudes toward antipsychotic medication: the impact of clinical variables and relationships with health professionals. Arch Gen Psychiatry. 2005. 62:717–724.21. Kim SW, Shin IS, Kim JM, Yang SJ, Shin HY, Yoon JS. Association between attitude toward medication and neurocognitive function in schizophrenia. Clin Neuropharmacol. 2006. 29:197–205.
Article22. Kim SW, Yoon JS, Lee MS, Lee HY. The analysis of newspaper-articles on psychosis. J Korean Neuropsychiatr Assoc. 2000. 39:838–848.23. Kim SW, Kim SY, Yoo JA, Bae KY, Kim JM, Shin IS, et al. The stigmatization of psychosis in Korean Newspaper articles. Korean J Schizophr Res. 2011. 14:42–49.24. Ono Y, Satsumi Y, Kim Y, Iwadate T, Moriyama K, Nakane Y, et al. Schizophrenia: is it time to replace the term? Psychiatry Clin Neurosci. 1999. 53:335–341.
Article25. Chung KF, Chan JH. Can a less pejorative Chinese translation for schizophrenia reduce stigma? A study of adolescents' attitudes toward people with schizophrenia. Psychiatry Clin Neurosci. 2004. 58:507–515.
Article26. Kim SW, Jang JE, Kim JM, Shin IS, Ban DH, Choi B, et al. Comparison of Stigma according to the Term Used for Schizophrenia: Split-Mind Disorder vs. Attunement Disorder. J Korean Neuropsychiatr Assoc. 2012. 51:210–217.
Article27. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 1994. 4th ed. Washington DC: American Psychiatric Press Inc.28. Hogan TP, Awad AG, Eastwood R. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med. 1983. 13:177–183.
Article29. Yoon BH, Bahk WM, Lee KU, Hong CH, Ahn JK, Kim MK. Psychometric properties of Korean version of Drug Attitude Inventory (KDAI-10). Korean J Psychopharmacol. 2005. 16:480–487.30. Amador XF, Flaum M, Andreasen NC, Strauss DH, Yale SA, Clark SC, et al. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch Gen Psychiatry. 1994. 51:826–836.
Article31. Thompson KN, McGorry PD, Harrigan SM. Reduced awareness of illness in first-episode psychosis. Compr Psychiatry. 2001. 42:498–503.
Article32. Gaebel W, Riesbeck M, von Wilmsdorff M, Burns T, Derks EM, Kahn RS, et al. Drug attitude as predictor for effectiveness in first-episode schizophrenia: Results of an open randomized trial (EUFEST). Eur Neuropsychopharmacol. 2010. 20:310–316.
Article33. Kamali M, Kelly BD, Clarke M, Browne S, Gervin M, Kinsella A, et al. A prospective evaluation of adherence to medication in first episode schizophrenia. Eur Psychiatry. 2006. 21:29–33.
Article34. Wong MM, Chen EY, Lui SS, Tso S. Medication adherence and subjective weight perception in patients with first-episode psychotic disorder. Clin Schizophr Relat Psychoses. 2011. 5:135–141.
Article35. Aleman A, Agrawal N, Morgan KD, David AS. Insight in psychosis and neuropsychological function: meta-analysis. Br J Psychiatry. 2006. 189:204–212.36. Amador XF, Gorman JM. Psychopathologic domains and insight in schizophrenia. Psychiatr Clin North Am. 1998. 21:27–42.
Article37. Marková IS, Berrios GE. The meaning of insight in clinical psychiatry. Br J Psychiatry. 1992. 160:850–860.
Article38. Cuffel BJ, Alford J, Fischer EP, Owen RR. Awareness of illness in schizophrenia and outpatient treatment adherence. J Nerv Ment Dis. 1996. 184:653–659.
Article39. Donohoe G, Owens N, O'Donnell C, Burke T, Moore L, Tobin A, et al. Predictors of compliance with neuroleptic medication among inpatients with schizophrenia: a discriminant function analysis. Eur Psychiatry. 2001. 16:293–298.
Article40. Kozuki Y, Froelicher ES. Lack of awareness and nonadherence in schizophrenia. West J Nurs Res. 2003. 25:57–74.
Article41. Mutsatsa SH, Joyce EM, Hutton SB, Webb E, Gibbins H, Paul S, et al. Clinical correlates of early medication adherence: West London first episode schizophrenia study. Acta Psychiatr Scand. 2003. 108:439–446.
Article42. Smith TE, Hull JW, Goodman M, Hedayat-Harris A, Willson DF, Israel LM, et al. The relative influences of symptoms, insight, and neurocognition on social adjustment in schizophrenia and schizoaffective disorder. J Nerv Ment Dis. 1999. 187:102–108.
Article43. Watson PW, Garety PA, Weinman J, Dunn G, Bebbington PE, Fowler D, et al. Emotional dysfunction in schizophrenia spectrum psychosis: the role of illness perceptions. Psychol Med. 2006. 36:761–770.
Article44. Tait L, Birchwood M, Trower P. Predicting engagement with services for psychosis: insight, symptoms and recovery style. Br J Psychiatry. 2003. 182:123–128.
Article45. Lincoln TM, Lüllmann E, Rief W. Correlates and long-term consequences of poor insight in patients with schizophrenia. Schizophr Bull. 2007. 33:1324–1342.
Article46. Park JI, Chung YC. Renaming the term 'schizophrenia' in Korea. Korean J Schizophr Res. 2008. 11:107–117.47. Green RS, Ganter AB. Telling patients and families the psychiatric diagnosis: a survey of psychiatrists. Hosp Community Psychiatry. 1987. 38:666–668.
Article48. Mitchell AJ. Reluctance to disclose difficult diagnoses: a narrative review comparing communication by psychiatrists and oncologists. Support Care Cancer. 2007. 15:819–828.
Article49. Clafferty RA, McCabe E, Brown KW. Conspiracy of silence? Telling patients with schizophrenia their diagnosis. Psychiatr Bull R Coll Psychiatr. 2001. 25:339.
Article50. Clafferty RA, McCabe E, Brown KW. Telling patients with schizophrenia their diagnosis. Patients should be informed about their illness. BMJ. 2000. 321:384–385.51. Atkinson JM. To tell or not to tell the diagnosis of schizophrenia. J Med Ethics. 1989. 15:21–24.
Article52. Nishimura Y, Ono H. Ono Y, editor. A study on renaming schizophrenia and informing diagnosis. Studies on the effects of renaming psychiatric disorders. 2005. Tokyo: Ministry of Health, Labor and Welfare;6–13. (in Japanese).53. Sato M, Koiwa M. Ono Y, editor. Prevalence of "Togo Shitcho Sho" (schizophrenia) and the ripple effect. Studies on the effects of renaming psychiatric disorders. 2005. Tokyo: Ministry of Health, Labor and Welfare;14–18. (in Japanese).54. Mitsumoto Sato. Integration disorder: the process and effects of renaming schizophrenia in Japan. Korean J Schizophr Res. 2008. 11:65–65.55. Staring AB, Van der Gaag M, Van den Berge M, Duivenvoorden HJ, Mulder CL. Stigma moderates the associations of insight with depressed mood, low self-esteem, and low quality of life in patients with schizophrenia spectrum disorders. Schizophr Res. 2009. 115:363–369.
Article56. Cooke M, Peters E, Fannon D, Anilkumar AP, Aasen I, Kuipers E, et al. Insight, distress and coping styles in schizophrenia. Schizophr Res. 2007. 94:12–22.
Article57. Lysaker PH, Roe D, Yanos PT. Toward understanding the insight paradox: internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophr Bull. 2007. 33:192–199.
Article58. Schwartz RC, Smith SD. Suicidality and psychosis: the predictive potential of symptomatology and insight into illness. J Psychiatr Res. 2004. 38:185–191.
Article59. Amador XF, Friedman JH, Kasapis C, Yale SA, Flaum M, Gorman JM. Suicidal behaviour in schizophrenia and its relationship to awareness of illness. Am J Psychiatry. 1996. 153:1185–1188.60. Schwartz RC, Petersen S. The relationship between insight and suicidality among patients with schizophrenia. J Nerv Ment Dis. 1999. 187:376–378.
Article61. Schwartz RC. Insight and suicidality in schizophrenia: a replication study. J Nerv Ment Dis. 2000. 188:235–237.
Article62. Kim CH, Jayathilake K, Meltzer HY. Hopelessness, neurocognitive function, and insight in schizophrenia: relationship to suicidal behavior. Schizophr Res. 2003. 60:71–80.
Article63. Beck EM, Cavelti M, Kvrgic S, Kleim B, Vauth R. Are we addressing the 'right stuff' to enhance adherence in schizophrenia? Understanding the role of insight and attitudes towards medication. Schizophr Res. 2011. 132:42–49.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Attitude Toward Illness and Treatment in Adherent Schizophrenia Patients: A Qualitative Study
- Treatment-Resistant Schizophrenia : Pathophysiology and Treatment
- Electroconvulsive Therapy in Schizophrenia: Clinical Applications and Effectiveness
- Antipsychotic Polypharmacy in Treatment of Schizophrenia; Should or Should Not?
- Subjective Quality of Life in Patients with Schizophrenia Receiving Antipsychotics: Relationship among Subjective Quality of Life, Drug Attitude, and Side-effect Profiles of Drugs