J Clin Neurol.
2011 Sep;7(3):168-172. 10.3988/jcn.2011.7.3.168.
Concurrence of Multifocal Motor Neuropathy and Hashimoto's Thyroiditis
- Affiliations
-
- 1Department of Neurology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Neurology, Research Institute and Hospital of National Cancer Center, Goyang, Korea.
- 3Department of Neurology, Clinical Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. kwoo@plaza.snu.ac.kr
- KMID: 2287634
- DOI: http://doi.org/10.3988/jcn.2011.7.3.168
Abstract
- BACKGROUND
Multifocal motor neuropathy (MMN) is an immune-mediated disorder that is characterized by slowly progressive and asymmetrical weakness, but its pathophysiological mechanism is uncertain. The hypothesis that MMN is an immunological disease has been supported by the proven therapeutic effects of intravenous immunoglobulin and the detection of antiganglioside antibodies in MMN patients. The coexistence of MMN with other immune diseases has been rarely reported.
CASE REPORT
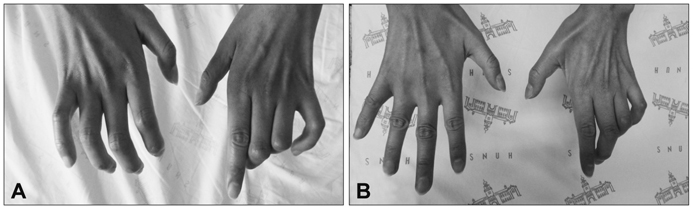
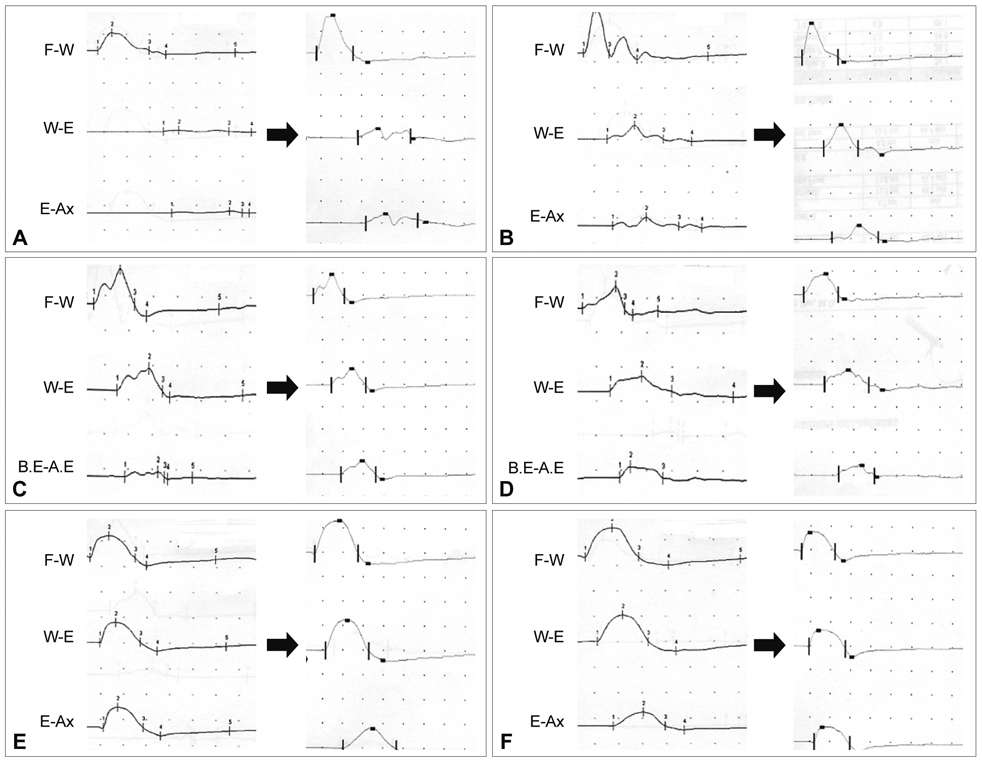
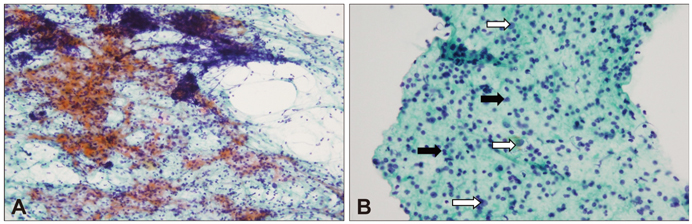
A 37-year-old woman visited our hospital complaining of weakness in both hands. The clinical manifestations coincided well with MMN: predominantly distal upper-limb weakness, asymmetric involvement, a progressive course, absence of sensory symptoms, absence of pyramidal signs, and sparing of the cranial muscles. The electrophysiological findings also supported a diagnosis of MMN, with motor nerve conduction block in the median, ulnar, and radial nerves, without sensory nerve involvement. The patient was simultaneously diagnosed as having Hashimoto's thyroiditis, which is a well-known immune-mediated disease.
CONCLUSIONS
The concurrence of MMN and Hashimoto's thyroiditis in our patient is significant for understanding the immunological characteristics of the two diseases.
MeSH Terms
Figure
Reference
-
1. Nobile-Orazio E, Cappellari A, Priori A. Multifocal motor neuropathy: current concepts and controversies. Muscle Nerve. 2005. 31:663–680.
Article2. Slee M, Selvan A, Donaghy M. Multifocal motor neuropathy: the diagnostic spectrum and response to treatment. Neurology. 2007. 69:1680–1687.
Article3. Pestronk A, Cornblath DR, Ilyas AA, Baba H, Quarles RH, Griffin JW, et al. A treatable multifocal motor neuropathy with antibodies to GM1 ganglioside. Ann Neurol. 1988. 24:73–78.
Article4. Léger JM, Chassande B, Musset L, Meininger V, Bouche P, Baumann N. Intravenous immunoglobulin therapy in multifocal motor neuropathy: a double-blind, placebo-controlled study. Brain. 2001. 124:145–153.
Article5. Nobile-Orazio E. Multifocal motor neuropathy. J Neuroimmunol. 2001. 115:4–18.
Article6. Kosugi S, Mori T, Iwamori M, Nagai Y, Imura H. Islet cell-activating protein reverses anti-fucosyl GM1 ganglioside antibody-induced inhibition of adenosine 3',5'-monophosphate production in FRTL-5 rat thyroid cells. Endocrinology. 1989. 124:1230–1234.
Article7. Wang C, Crapo LM. The epidemiology of thyroid disease and implications for screening. Endocrinol Metab Clin North Am. 1997. 26:189–218.
Article8. Amino N, Tada H, Hidaka Y, Hashimoto K. Hashimoto's disease and Dr. Hakaru Hashimoto. Endocr J. 2002. 49:393–397.9. Jenkins RC, Weetman AP. Disease associations with autoimmune thyroid disease. Thyroid. 2002. 12:977–988.
Article10. Chaudhry V, Corse AM, Cornblath DR, Kuncl RW, Freimer ML, Griffin JW. Multifocal motor neuropathy: electrodiagnostic features. Muscle Nerve. 1994. 17:198–205.
Article11. Arasaki K, Kusunoki S, Kudo N, Kanazawa I. Acute conduction block in vitro following exposure to antiganglioside sera. Muscle Nerve. 1993. 16:587–593.
Article12. Kanda T, Iwasaki T, Yamawaki M, Tai T, Mizusawa H. Anti-GM1 antibody facilitates leakage in an in vitro blood-nerve barrier model. Neurology. 2000. 55:585–587.
Article13. Fishman PS, Shy ME, Hart DE, Thompson PE, Cashman NR. Antibodies to the ganglioside GD1b in a patient with motor neuron disease and thyroid adenoma. Arch Neurol. 1991. 48:1188–1190.
Article14. Toscano A, Rodolico C, Benvenga S, Girlanda P, Laurà M, Mazzeo A, et al. Multifocal motor neuropathy and asymptomatic Hashimotos thyroiditis: first report of an association. Neuromuscul Disord. 2002. 12:566–568.
Article15. Kwon JY, Kim JY, Jeong JH, Park KD. Multiple sclerosis and peripheral multifocal demyelinating neuropathies occurring in a same patient. J Clin Neurol. 2008. 4:51–57.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Demyelinating Peripheral Neuropathy Associated with Hashimoto's Thyroiditis
- Ultrasonographic Findings of Papillary Thyroid Cancer with or without Hashimoto's Thyroiditis
- Progression of Hashimoto’s Thyroiditis to Graves’ Disease: a Report of Two Pediatric Cases
- Hashimoto Thyroiditis Presenting with a Transient Myotonia
- Association Kikuchi disease with Hashimoto thyroiditis: a case report and literature review