Diabetes Metab J.
2011 Aug;35(4):384-389. 10.4093/dmj.2011.35.4.384.
Long Menstrual Cycle Is Associated with Type 2 Diabetes Mellitus in Korean Women
- Affiliations
-
- 1Division of Endocrinology, Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea. jyoh@ewha.ac.kr
- KMID: 2281645
- DOI: http://doi.org/10.4093/dmj.2011.35.4.384
Abstract
- BACKGROUND
Long menstrual cycle is a risk factor for developing type 2 diabetes and cardiovascular disease in women. We aimed to evaluate the association between existing type 2 diabetes and oligomenorrhea before diagnosis of diabetes, and to observe the differences in this association among obese and non-obese Korean women.
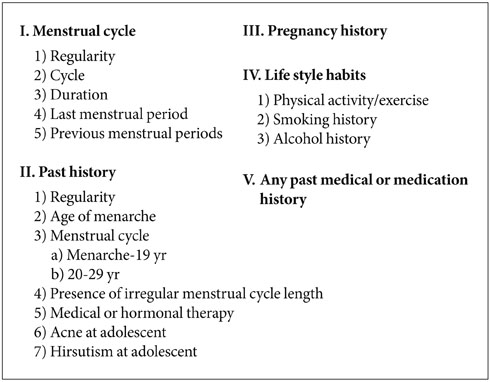
METHODS
Patients with type 2 diabetes (n=118) and without any clinical evidence of abnormal glucose regulation (n=258) who attended the outpatient clinic of a university hospital and were over age 30. Patients self-reporting a menstrual cycle over 40 days during their 20s were defined as oligomenorrhea before diagnosis of diabetes. Obesity was defined as having a body mass index (BMI) over 25 kg/m2.
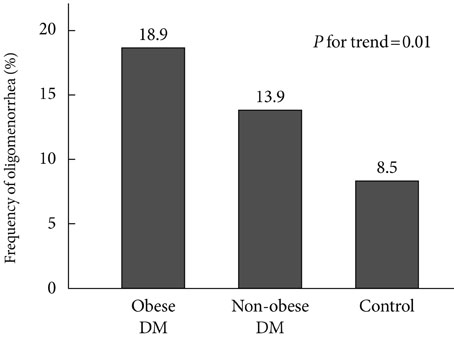
RESULTS
The frequency of oligomenorrhea before diagnosis of diabetes was almost two-fold higher in women with type 2 diabetes than in the control group (16.1% vs. 8.5%, P=0.03). Oligomenorrhea was associated with type 2 diabetes after adjusting for age, BMI, systolic blood pressure, triglycerides, and high density lipoprotein cholesterol (odds ratio, 3.89; 95% confidence interval, 1.37 to 11.04). Among women with oligomenorrhea before diagnosis of diabetes, the frequency of type 2 diabetes was significantly higher in obese subjects than in their non-obese counterparts (90.9% vs. 30.0%, P=0.03).
CONCLUSION
Having a long menstrual cycle could be a risk factor for the development of type 2 diabetes, especially in obese women.
Keyword
MeSH Terms
Figure
Reference
-
1. Edelman SV. Type II diabetes mellitus. Adv Intern Med. 1998. 43:449–500.2. Knowler WC, Saad MF, Pettitt DJ, Nelson RG, Bennett PH. Determinants of diabetes mellitus in the Pima Indians. Diabetes Care. 1993. 16:216–227.3. Solomon CG, Hu FB, Dunaif A, Rich-Edwards JE, Stampfer MJ, Willett WC, Speizer FE, Manson JE. Menstrual cycle irregularity and risk for future cardiovascular disease. J Clin Endocrinol Metab. 2002. 87:2013–2017.4. Griffin ML, South SA, Yankov VI, Booth RA Jr, Asplin CM, Veldhuis JD, Evans WS. Insulin-dependent diabetes mellitus and menstrual dysfunction. Ann Med. 1994. 26:331–340.5. Solomon CG, Rich-Edwards JW, Dunaif A, Willett WC, Hunter DJ, Stampfer MJ, Colditz GA, Spiegelman D, Manson JE. Abnormal menstrual cycle length predicts subsequent non-insulin-dependent diabetes mellitus. Am J Epidemiol. 1998. 147:11 Suppl. S60.6. Solomon CG, Hu FB, Dunaif A, Rich-Edwards J, Willett WC, Hunter DJ, Colditz GA, Speizer FE, Manson JE. Long or highly irregular menstrual cycles as a marker for risk of type 2 diabetes mellitus. JAMA. 2001. 286:2421–2426.7. Roumain J, Charles MA, de Courten MP, Hanson RL, Brodie TD, Pettitt DJ, Knowler WC. The relationship of menstrual irregularity to type 2 diabetes in Pima Indian women. Diabetes Care. 1998. 21:346–349.8. Salley KE, Wickham EP, Cheang KI, Essah PA, Karjane NW, Nestler JE. Glucose intolerance in polycystic ovary syndrome: a position statement of the Androgen Excess Society. J Clin Endocrinol Metab. 2007. 92:4546–4556.9. Legro RS, Kunselman AR, Dodson WC, Dunaif A. Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: a prospective, controlled study in 254 affected women. J Clin Endocrinol Metab. 1999. 84:165–169.10. Hartz AJ, Barboriak PN, Wong A, Katayama KP, Rimm AA. The association of obesity with infertility and related menstural abnormalities in women. Int J Obes. 1979. 3:57–73.11. Dunaif A. Hyperandrogenic anovulation (PCOS): a unique disorder of insulin action associated with an increased risk of non-insulin-dependent diabetes mellitus. Am J Med. 1995. 98(1A):33S–39S.12. Longcope C, Baker R, Johnston CC Jr. Androgen and estrogen metabolism: relationship to obesity. Metabolism. 1986. 35:235–237.13. Weiss DJ, Charles MA, Dunaif A, Prior DE, Lillioja S, Knowler WC, Herman WH. Hyperinsulinemia is associated with menstrual irregularity and altered serum androgens in Pima Indian women. Metabolism. 1994. 43:803–807.14. Poretsky L, Kalin MF. The gonadotropic function of insulin. Endocr Rev. 1987. 8:132–141.15. Lillioja S, Mott DM, Spraul M, Ferraro R, Foley JE, Ravussin E, Knowler WC, Bennett PH, Bogardus C. Insulin resistance and insulin secretory dysfunction as precursors of non-insulin-dependent diabetes mellitus: prospective studies of Pima Indians. N Engl J Med. 1993. 329:1988–1992.16. Ehrmann DA, Barnes RB, Rosenfield RL, Cavaghan MK, Imperial J. Prevalence of impaired glucose tolerance and diabetes in women with polycystic ovary syndrome. Diabetes Care. 1999. 22:141–146.17. Adams J, Polson DW, Franks S. Prevalence of polycystic ovaries in women with anovulation and idiopathic hirsutism. Br Med J (Clin Res Ed). 1986. 293:355–359.18. Plymate SR, Matej LA, Jones RE, Friedl KE. Inhibition of sex hormone-binding globulin production in the human hepatoma (Hep G2) cell line by insulin and prolactin. J Clin Endocrinol Metab. 1988. 67:460–464.19. Nestler JE, Powers LP, Matt DW, Steingold KA, Plymate SR, Rittmaster RS, Clore JN, Blackard WG. A direct effect of hyperinsulinemia on serum sex hormone-binding globulin levels in obese women with the polycystic ovary syndrome. J Clin Endocrinol Metab. 1991. 72:83–89.20. Haffner SM, Valdez RA, Morales PA, Hazuda HP, Stern MP. Decreased sex hormone-binding globulin predicts noninsulin-dependent diabetes mellitus in women but not in men. J Clin Endocrinol Metab. 1993. 77:56–60.21. Dunaif A, Finegood DT. Beta-cell dysfunction independent of obesity and glucose intolerance in the polycystic ovary syndrome. J Clin Endocrinol Metab. 1996. 81:942–947.22. Coviello AD, Legro RS, Dunaif A. Adolescent girls with polycystic ovary syndrome have an increased risk of the metabolic syndrome associated with increasing androgen levels independent of obesity and insulin resistance. J Clin Endocrinol Metab. 2006. 91:492–497.23. Lewy VD, Danadian K, Witchel SF, Arslanian S. Early metabolic abnormalities in adolescent girls with polycystic ovarian syndrome. J Pediatr. 2001. 138:38–44.24. Palmert MR, Gordon CM, Kartashov AI, Legro RS, Emans SJ, Dunaif A. Screening for abnormal glucose tolerance in adolescents with polycystic ovary syndrome. J Clin Endocrinol Metab. 2002. 87:1017–1023.25. Tfayli H, Arslanian S. Menstrual health and the metabolic syndrome in adolescents. Ann N Y Acad Sci. 2008. 1135:85–94.26. Hull MG. Epidemiology of infertility and polycystic ovarian disease: endocrinological and demographic studies. Gynecol Endocrinol. 1987. 1:235–245.27. Dunaif A, Graf M, Mandeli J, Laumas V, Dobrjansky A. Characterization of groups of hyperandrogenic women with acanthosis nigricans, impaired glucose tolerance, and/or hyperinsulinemia. J Clin Endocrinol Metab. 1987. 65:499–507.28. Ireland K, Child T. Polycystic ovary syndrome and the postmenopausal woman. J Br Menopause Soc. 2006. 12:143–148.29. Chang RJ, Nakamura RM, Judd HL, Kaplan SA. Insulin resistance in nonobese patients with polycystic ovarian disease. J Clin Endocrinol Metab. 1983. 57:356–359.30. Must A, Phillips SM, Naumova EN, Blum M, Harris S, Dawson-Hughes B, Rand WM. Recall of early menstrual history and menarcheal body size: after 30 years, how well do women remember? Am J Epidemiol. 2002. 155:672–679.31. Jukic AM, Weinberg CR, Wilcox AJ, McConnaughey DR, Hornsby P, Baird DD. Accuracy of reporting of menstrual cycle length. Am J Epidemiol. 2008. 167:25–33.32. Bachand AM, Cragin LA, Reif JS. Reliability of retrospectively assessed categorical menstrual cycle length data. Ann Epidemiol. 2009. 19:501–503.33. Small CM, Manatunga AK, Marcus M. Validity of self-reported menstrual cycle length. Ann Epidemiol. 2007. 17:163–170.