Ann Rehabil Med.
2011 Dec;35(6):833-843. 10.5535/arm.2011.35.6.833.
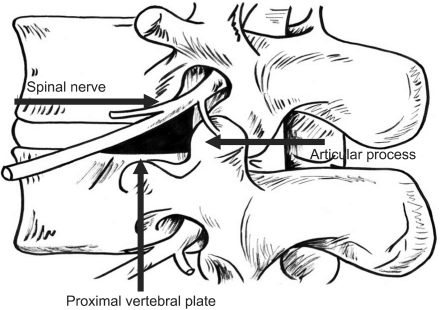
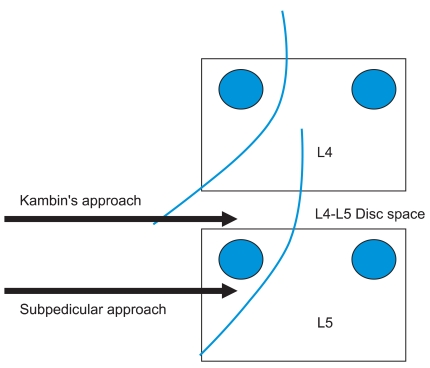
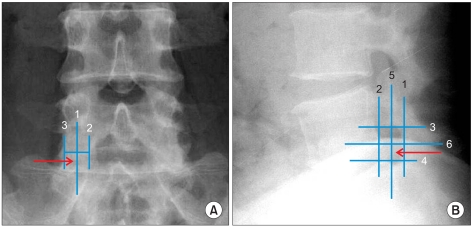
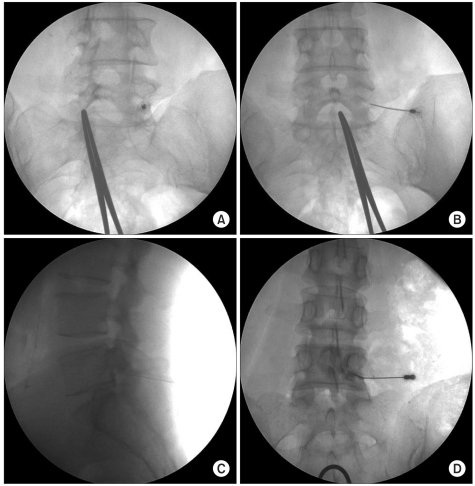
Kambin's Triangle Approach of Lumbar Transforaminal Epidural Injection with Spinal Stenosis
- Affiliations
-
- 1Department of Rehabilitation Medicine, Soonchunhyang University College of Medicine, Seoul 140-887, Korea.
- 2Department of Rehabilitation Medicine, Hallym University College of Medicine, Seoul 134-814, Korea.
- 3Department of Rehabilitation Medicine, Samyook Hospital, Gwangju 464-864, Korea.
- 4Department of Rehabilitation Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul 139-707, Korea. swc328@naver.com
- KMID: 2266809
- DOI: http://doi.org/10.5535/arm.2011.35.6.833
Abstract
OBJECTIVE
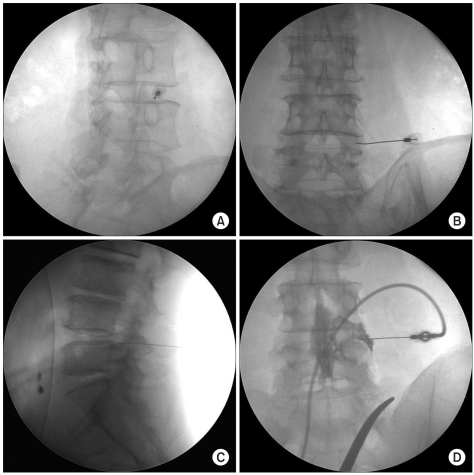
To compare the short-term effect and advantage of transforaminal epidural steroid injection (TFESI) performed using the Kambin's triangle and subpedicular approaches. METHOD: Forty-two patients with radicular pain from lumbar spinal stenosis were enrolled. Subjects were randomly assigned to one of two groups. All procedures were performed using C-arm KMC 950. The frequency of complications during the procedure and the effect of TFESI at 2 and 4 weeks after the procedure between the two groups were compared. Short-term outcomes were measured using a visual numeric scale (VNS) and a five-grade scale. Multiple logistic regression analyses were performed to evaluate the relationship between possible outcome predictors (Kambin's triangle or subpedicular approach, age, duration of symptoms and sex) and the therapeutic effect.
RESULTS
VNS was improved 2 weeks after the injection and continued to improve until 4 weeks in both groups. There were no statistical differences in changes of VNS, effectiveness and contrast spread pattern between these two groups. No correlation was found between the other variables tested and therapeutic effect. Spinal nerve pricking occurred in five cases of the subpedicular and in none of the cases of the Kambin's triangle approach (p<0.05).
CONCLUSION
The Kambin's triangle approach is as efficacious as the subpedicular approach for short-term effect and offers considerable advantages (i.e., less spinal nerve pricking during procedure). The Kambin's triangle approach maybe an alternative method for transforaminal epidural steroid injection in cases where needle tip positioning in the anterior epidural space is difficult.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Cadaveric anatomy of the lumbar triangular safe zone of Kambin’s in North West Indian population
Chiman Kumari, Tulika Gupta, Richa Gupta, Vishal Kumar, Daisy Sahni, Anjali Aggarwal, Neelkamal
Anat Cell Biol. 2021;54(1):35-41. doi: 10.5115/acb.20.243.
Reference
-
1. Grubb SA, Lipscomb HJ, Coonrad RW. Degenerative adult onset scoliosis. Spine. 1988; 13:241–245. PMID: 2968664.
Article2. Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine (Phila Pa 1976). 1994; 15:1619–1627. PMID: 7939999.
Article3. Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age,sex, and size. A prospective controlled clinical study. Spine. 1994; 19:1611–1161. PMID: 7939998.4. Rydevik B, Brown MD, Lundborg G. Pathoanatomy and pathophysiology of nerve root compression. Spine. 1984; 9:7–15. PMID: 6372124.
Article5. Olmarker K, Redevik B, Holm S. Edema formation in spinal nerve roots induced by experimental, graded compression. An experimental study on the pig cauda equina with special reference to differences in effects between rapid and slow onset of compression. Spine. 1989; 14:569–573. PMID: 2546258.6. Kantrowitz F, Robinson DR, McGuire MB, Levine L. Corticosteroids inhibit prostaglandin production by rheumatoid synovia. Nature. 1975; 258:737–739. PMID: 1207758.
Article7. Fukusaki M, Kobayashi I, Hara T, Sumikawa K. Symptoms of spinal stenosis do not improve after epidural steroid injection. Clin J Pain. 1998; 14:148–151. PMID: 9647457.
Article8. Johansson A, Hao J, Sjolund B. Local corticosteroid application blocks transmission in normal nociceptive C-fibres. Acta Anaesthesiol Scand. 1990; 34:335–338. PMID: 2167604.
Article9. Slipman CW, Chow DW. Therapeutic spinal corticosteroid injections for the management of radiculopathies. Phys Med Rehabil Clin N Am. 2002; 13:697–711. PMID: 12380554.
Article10. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002; 27:11–16. PMID: 11805628.11. Manchikanti L, Cash KA, Pampati V, Damron KS, McManus CD. Evaluation of lumbar transforaminal epidural injections with needle placement and contrast flow patterns: a prospective, descriptive report. Pain Physician. 2004; 7:217–223. PMID: 16868595.12. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED, Slaten WK, Rao S. Fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil. 2002; 81:898–905. PMID: 12447088.13. Murthy NS, Maus TP, Behrns CL. Intraforaminal location of the great anterior radiculomedullary artery (artery of Adamkiewicz): a retrospective review. Pain Med. 2010; 11:1756–1764. PMID: 21134118.
Article14. Kambin P, Sampson S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin Orthop Relat Res. 1986; 207:37–43. PMID: 3720102.15. Kambin P. Arthroscopic microdiskectomy. Mt Sinai J Med. 1991; 58:159–164. PMID: 1857361.16. Kambin P, Savitz MH. Arthroscopic microdiscectomy: an alternative to open disc surgery. Mt Sinai J Med. 2000; 67:283–287. PMID: 11021778.17. Jasper JF. Lumbar retrodiscal transforaminal injection. Pain Physician. 2007; 10:501–510. PMID: 17525785.
Article18. Lew HL, Coelho P, Chou LH. Preganglionic approach to transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2004; 83:378. PMID: 15100628.
Article19. Lee CK, Rauschning W, Glenn W. Lateral lumbar spinal canal stenosis: classification, pathologic anatomy and surgical decompression. Spine. 1988; 13:313–320. PMID: 3388117.
Article20. Delport EG, Cucuzzella AR, Marley JK, Pruitt CM, Fisher JR. Treatment of lumbar spinal stenosis with epidural steroid injections: a retrospective outcome study. Arch Phys Med Rehabil. 2004; 85:479–484. PMID: 15031837.
Article21. Riew KD, Yin Y, Gilula L, Bridwell KH, Lenke LG, Lauryssen C, Goette K. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blind study. J Bone Joint Surg Am. 2000; 82:1589–1593. PMID: 11097449.22. Boswell MV, Hansen HC, Trescot AM, Hirsch JA. Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Physician. 2003; 6:319–334. PMID: 16880879.23. Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Physician. 2000; 3:374–398. PMID: 16906179.
Article24. Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002; 2:70–75. PMID: 14588291.25. Glaser SE, Falco F. Paraplegia following a thoracolumbar transforaminal epidural steroid injection. Pain Physician. 2005; 8:309–314. PMID: 16850088.26. Glaser SE, Shah RV. Root cause analysis of paraplegia following transforaminal epidural steroid injections: the 'unsafe' triangle. Pain Physician. 2010; 13:237–244. PMID: 20495587.27. Alleyne CH Jr, Cawley CM, Shengelaia GG, Barrow DL. Microsurgical anatomy of the artery of Adamkiewicz and its segmental artery. J Neurosurg. 1998; 89:791–795. PMID: 9817417.
Article28. Groen RJ, Groenewegen HJ, van Alphen HA, Hoogland PV. Morphology of the human internal vertebral venous plexus: a cadaver study after intravenous Araldite CY 221 injection. Anat Rec. 1997; 249:285–294. PMID: 9335475.
Article29. Crall TS, Gilula LA, Kim YJ, Cho Y, Pilgram T, Riew KD. The diagnostic effect of various needle tip positions in selective lumbar nerve blocks: an analysis of 1202 injections. Spine. 2006; 31:920–922. PMID: 16622382.
Article30. Lee JW, Kim SH, Choi JY, Yeom JS, Kim KJ, Chung SK, Kim HJ, Kim C, Kwack KS, Kwon JW, et al. Transforaminal epidural steroid injection for lumbosacral radiculopathy: preganglionic versus conventional approach. Korean J Radiol. 2006; 7:139–144. PMID: 16799275.
Article31. Jeong HS, Lee JW, Kim SH, Myung JS, Kim JH, Kang HS. Effectiveness of transforaminal epidural steroid injection by using a preganglionic approach: a prospective randomized controlled study. Radiology. 2007; 245:584–590. PMID: 17940309.
Article32. Lee IS, Kim SH, Lee JW, Hong SH, Choi JY, Kang HS, Song JW, Kwon AK. Comparison of the temporary diagnostic relief of transforaminal epidural steroid injection approaches: conventional versus posterolateral technique. AJNR. 2007; 28:204–208. PMID: 17296980.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Full-endoscopic Trans-Kambin’s Triangle Lumbar Interbody Fusion: Technique and Review of Literature
- Injectate Volumes Needed to Reach Specific Landmarks and Contrast Pattern in Kambin's Triangle Approach with Spinal Stenosis
- Lumbar Ventral Epidural Approach
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy
- Cadaveric anatomy of the lumbar triangular safe zone of Kambin’s in North West Indian population