Ann Rehabil Med.
2012 Aug;36(4):480-487. 10.5535/arm.2012.36.4.480.
Injectate Volumes Needed to Reach Specific Landmarks and Contrast Pattern in Kambin's Triangle Approach with Spinal Stenosis
- Affiliations
-
- 1Department of Rehabilitation Medicine, Gachon University of Medicine and Science, Gil Medical Center, Incheon 405-760, Korea.
- 2Department of Radiology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul 139-707, Korea.
- 3Department of Rehabilitation Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul 139-707, Korea. swc328@naver.com
- KMID: 2266718
- DOI: http://doi.org/10.5535/arm.2012.36.4.480
Abstract
OBJECTIVE
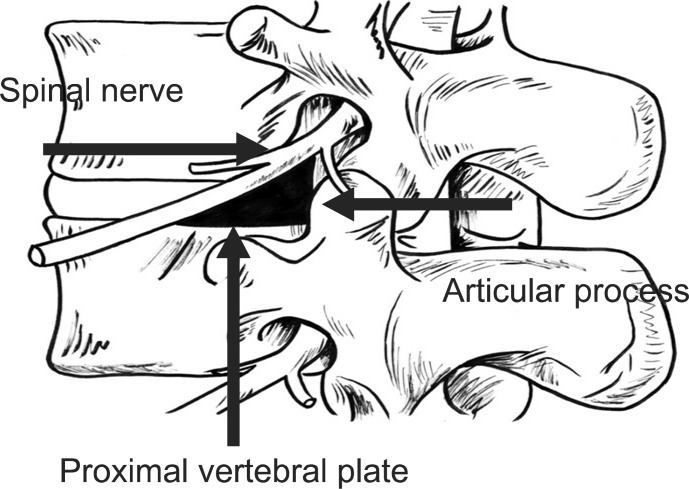
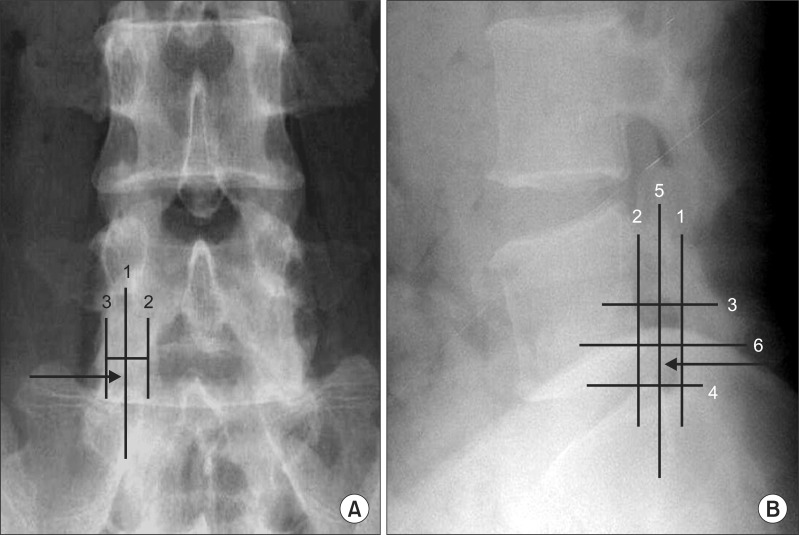
To identify the volumes of contrast material needed to reach the specific landmarks and contrast pattern during Kambin's triangle approach (KB-A) in lumbar spinal stenosis. METHOD: Sixty patients undergoing KB-A were investigated. Fifty-six patients were included in this study. KB-A were performed with the use of contrast-enhanced fluoroscopic visualization. After confirming the appropriate spinal needle position, a slow injection of up to 5.0 ml of nonionic contrast material was carried out. Under intermittent fluoroscopic guidance, contrast volumes were recorded as flow reached specific anatomic landmarks: ipsilateral inferior or superior neural foramen.
RESULTS
After 2.0 ml of contrast was injected, 93.2% of KB-A cases spread to the medial aspect of the inferior pedicle of the corresponding level of injection and 86.3% of KB-A spread to the medial aspect of the superior pedicle of the corresponding level of injection. After 3 ml of contrast was injected, 95.3% of KB-A spread to cover both the medial aspect of the inferior pedicle and the superior pedicle of the corresponding level of injection. A volume of 2 ml of injectate reaches the anterior epidural space 100% of the time.
CONCLUSION
This study demonstrates injectate volumes needed to reach the specific anatomic landmarks in KB-A. A volume of 3.0 ml of injectate reaches both the medial aspect of theinferior pedicle and the superior pedicle 94.6% of the time. Therefore, Interventionalists may consider a 1-level instead of a 2-level injection for patients with a bleeding risk or for 2 level central pathology.
Keyword
Figure
Reference
-
1. Slipman CW, Chow DW. Therapeutic spinal corticosteroid injections for the management of radiculopathies. Phys Med Rehabil Clin N Am. 2002; 13:697–711. PMID: 12380554.
Article2. Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine. 2002; 27:11–16. PMID: 11805628.3. Manchikanti L, Cash KA, Pampati V, Damron KS, McManus CD. Evaluation of lumbar transforaminal epidural injections with needle placement and contrast flow patterns: a prospective, descriptive report. Pain Physician. 2004; 7:217–223. PMID: 16868595.4. Murthy NS, Maus TP, Behrns CL. Intraforaminal location of the great anterior radiculomedullary artery (artery of Adamkiewicz): a retrospective review. Pain Med. 2010; 11:1756–1764. PMID: 21134118.
Article5. Botwin KP, Gruber RD, Bouchlas CG, Torres-Ramos FM, Sanelli JT, Freeman ED, Slaten WK, Rao S. Fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar stenosis: an outcome study. Am J Phys Med Rehabil. 2002; 81:898–905. PMID: 12447088.6. Kambin P, Brager MD. Percutaneous posterolateral discectomy. Anatomy and mechanism. Clin Orthop Relat Res. 1987; 223:145–154. PMID: 3652568.7. Kambin P. Arthroscopic microdiskectomy. Mt Sinai J Med. 1991; 58:159–164. PMID: 1857361.8. Furman MB, Mehta AR, Kim RE, Simon JI, Patel R, Lee TS, Reeves RS. Injectate volumes needed to reach specific landmarks in lumbar transforaminal epidural injections. PM R. 2010; 2:625–635. PMID: 20659718.
Article9. Hogan QH. Epidural anatomy examined by cryomicrotome section. Influence of age, vertebral level, and disease. Reg Anesth. 1996; 21:395–406. PMID: 8895998.10. Glaser SE, Shah RV. Root cause analysis of paraplegia following transforaminal epidural steroid injections: the 'unsafe' triangle. Pain Physician. 2010; 13:237–244. PMID: 20495587.11. Kambin P, Savitz MH. Arthroscopic microdiscectomy: an alternative to open disc surgery. Mt Sinai J Med. 2000; 67:283–287. PMID: 11021778.12. Jasper JF. Lumbar retrodiscal transforaminal injection. Pain Physician. 2007; 10:501–510. PMID: 17525785.
Article13. Lew HL, Coelho P, Chou LH. Preganglionic approach to transforaminal epidural steroid injections. Am J Phys Med Rehabil. 2004; 83:378. PMID: 15100628.
Article14. Lee IS, Kim SH, Lee JW, Hong SH, Choi JY, Kang HS, Song JW, Kwon AK. Comparison of the temporary diagnostic relief of transforaminal epidural steroid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol. 2007; 28:204–208. PMID: 17296980.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Kambin's Triangle Approach of Lumbar Transforaminal Epidural Injection with Spinal Stenosis
- Full-endoscopic Trans-Kambin’s Triangle Lumbar Interbody Fusion: Technique and Review of Literature
- Get Ready for 100 Years of Active Spine Life Using Percutaneous Endoscopic Spine Surgery (PESS)
- Anatomic Considerations of Intervertebral Disc Perspective in Lumbar Posterolateral Approach via Kambin's Triangle: Cadaveric Study
- Cadaveric anatomy of the lumbar triangular safe zone of Kambin’s in North West Indian population