Correlation between Location of Brain Lesion and Cognitive Function and Findings of Videofluoroscopic Swallowing Study
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Korea University College of Medicine, Seoul 136-705, Korea. hkkwon@korea.ac.kr
- KMID: 2266740
- DOI: http://doi.org/10.5535/arm.2012.36.3.347
Abstract
OBJECTIVE
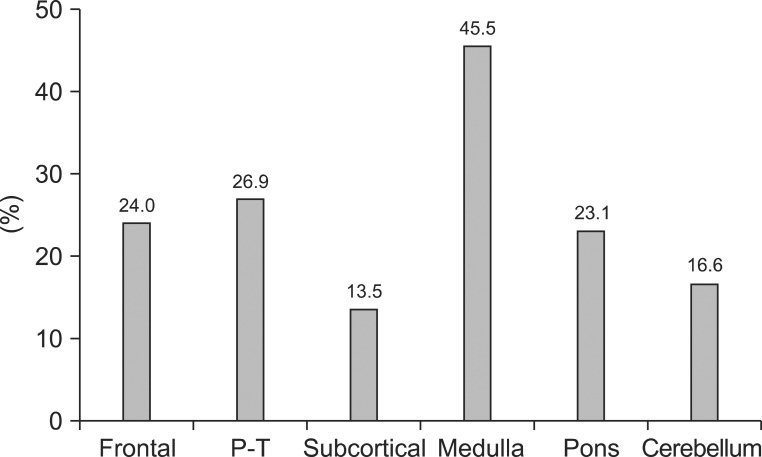
To investigate whether patterns of swallowing difficulties were associated with the location of the brain lesion, cognitive function, and severity of stroke in stroke patients. METHOD: Seventy-six patients with first-time acute stroke were included in the present investigation. Swallowing-related parameters, which were assessed videofluoroscopically, included impairment of lip closure, decreased tongue movement, amount of oral remnant, premature loss of food material, delay in oral transit time, laryngeal elevation, delay in pharyngeal triggering time, presence of penetration or aspiration, and the amount of vallecular and pyriform sinus remnants. The locations of brain lesions were classified into the frontal, parietotemporal, subcortical, medulla, pons, and cerebellum. The degree of cognitive impairment and the severity of stroke were assessed by the Mini Mental Status Examination (MMSE) and the National Institute of Health Stroke Scale (NIHSS), respectively.
RESULTS
An insufficient laryngeal elevation, the amount of pyriform sinus, and vallecular space remnant in addition to the incidence of aspiration were correlated with medullary infarction. Other swallowing parameters were not related to lesion topology. Lip closure dysfunction, decreased tongue movement, increased oral remnant and premature loss were associated with low MMSE scores. A delayed oral transit time were associated with NIHSS scores.
CONCLUSION
In-coordination of the lip, the tongue, and the oropharynx were associated with the degree of cognitive impairment and the stroke severity rather than with the location of the lesion, whereas incomplete laryngeal elevation and aspiration were predominant in medullary lesions.
MeSH Terms
Figure
Cited by 4 articles
-
Characteristics of Patients With Aneurysmal Subarachnoid Hemorrhage and Risk Factors Related to Dysphagia
Seung Hwa Rhie, Ji Won Choi, Se Jeong Jeon, Sung Don Kang, Min Cheol Joo, Min Su Kim
Ann Rehabil Med. 2016;40(6):1024-1032. doi: 10.5535/arm.2016.40.6.1024.The Relationship Between Tongue Pressure and Oral Dysphagia in Stroke Patients
Jong Ha Lee, Hee-Sang Kim, Dong Hwan Yun, Jinmann Chon, Yoo Jin Han, Seung Don Yoo, Dong Hwan Kim, Seung Ah Lee, Hye In Joo, Ji-su Park, Jin Chul Kim, Yunsoo Soh
Ann Rehabil Med. 2016;40(4):620-628. doi: 10.5535/arm.2016.40.4.620.Relationship Between Cognitive Function and Dysphagia After Stroke
Soo Yung Jo, Jeong-Won Hwang, Sung-Bom Pyun
Ann Rehabil Med. 2017;41(4):564-572. doi: 10.5535/arm.2017.41.4.564.Association of Brain Lesions and Videofluoroscopic Dysphagia Scale Parameters on Patients With Acute Cerebral Infarctions
Sang Jun Mo, Ho Joong Jeong, Yong Hyun Han, Kihun Hwang, Jong Kyoung Choi
Ann Rehabil Med. 2018;42(4):560-568. doi: 10.5535/arm.2018.42.4.560.
Reference
-
1. Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL. Aspiration in patients with acute stroke. Arch Phys Med Rehabil. 1998; 79:14–19. PMID: 9440410.
Article2. Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. Br Med J (Clin Res Ed). 1987; 295:411–441.
Article3. Smithard DG, O'Neill PA, England RE, Park CL, Wyatt R, Martin DF, Morris J. The natural history of dysphagia following a stroke. Dysphagia. 1997; 12:188–193. PMID: 9294937.
Article4. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999; 30:744–748. PMID: 10187872.5. Splaingard ML, Hutchins B, Sulton LD, Chaudhuri G. Aspiration in rehabilitation patients: videofluoroscopy vs bedside clinical assessment. Arch Phys Med Rehabil. 1988; 69:637–640. PMID: 3408337.6. Robbins J, Levin RL. Swallowing after unilateral stroke of the cerebral cortex: preliminary experience. Dysphagia. 1988; 3:11–17. PMID: 3248391.
Article7. Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993; 74:1295–1300. PMID: 8259895.
Article8. Alberts MJ, Horner J, Gray L, Brazer SR. Aspiration after stroke: lesion analysis by brain MRI. Dysphagia. 1992; 7:170–173. PMID: 1499361.
Article9. Lee CK, Kim JA. Pattern of post-stroke swallowing disorder according to the brain lesion. J Korean Acad Rehabil Med. 2001; 25:193–201.10. Steinhagen V, Grossmann A, Benecke R, Walter U. Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke. 2009; 40:1903–1906. PMID: 19286597.
Article11. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, Pedace C, Lenzi L. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–335. PMID: 19717014.
Article12. Langdon PC, Lee AH, Binns CW. Dysphagia in acute ischaemic stroke: severity, recovery and relationship to stroke subtype. J Clin Neurosci. 2007; 14:630–634. PMID: 17434310.
Article13. Broadley S, Croser D, Cottrell J, Creevy M, Teo E, Yiu D, Pathi R, Taylor J, Thompson PD. Predictors of prolonged dysphagia following acute stroke. J Clin Neurosci. 2003; 10:300–305. PMID: 12763332.
Article14. Schroeder MF, Daniels SK, McClain M, Corey DM, Foundas AL. Clinical and cognitive predictors of swallowing recovery in stroke. J Rehabil Res Dev. 2006; 43:301–310. PMID: 17041816.
Article15. Lyden PD, Lu M, Levine SR, Brott TG, Broderick J. A modified National Institutes of Health Stroke Scale for use in stroke clinical trials: preliminary reliability and validity. Stroke. 2001; 32:1310–1317. PMID: 11387492.16. Lee KM, Jang YH, Kim YH, Moon SK, Park JH, Park SW, Yu HJ, Lee SG, Chun MH, Han TR. Reliability and validity of Korean Version of National Institutes of Health Stroke Scale. J Korean Acad Rehabil Med. 2004; 28:422–435.17. Mungas D, Marshall SC, Weldon M, Haan M, Reed BR. Age and education correction of Mini-Mental State Examination for English and Spanish-speaking elderly. Neurology. 1996; 46:700–706. PMID: 8618670.
Article18. Kohn R, Vicente B, Rioseco P, Saldivia S, Torres S. The mini-mental state examination: age and education distribution for a Latin American population. Aging Ment Health. 2008; 12:66–71. PMID: 18297480.
Article19. Kim SJ, Park YH. Comparison of sensitivity of neurobehavioral cognitive status examination and minimental state examination. J Korean Acad Rehabil Med. 1997; 21:1105–1109.20. Granger CV, Dewis LS, Peters NC, Sherwood CC, Barrett JE. Stroke rehabilitation: analysis of repeated Barthel index measures. Arch Phys Med Rehabil. 1979; 60:14–17. PMID: 420565.21. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, Kim SH, Kim TH, Han TR. Development of the Korean Version of Modified Barthel Index (K-MBI): multicenter study for subjects with stroke. J Korean Acad Rehabil Med. 2007; 31:283–297.22. Logemann JA. Swallowing physiology and pathophysiology. Otolaryngol Clin North Am. 1988; 21:613–623. PMID: 3054716.
Article23. Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010; 41:482–486. PMID: 20093638.
Article24. Paciaroni M, Mazzotta G, Corea F, Caso V, Venti M, Milia P, Silvestrelli G, Palmerini F, Parnetti L, Gallai V. Dysphagia following Stroke. Eur Neurol. 2004; 51:162–167. PMID: 15073441.
Article25. Achem SR, Devault KR. Dysphagia in aging. J Clin Gastroenterol. 2005; 39:357–371. PMID: 15815202.
Article26. Daggett A, Logemann J, Rademaker A, Pauloski B. Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia. 2006; 21:270–274. PMID: 17216388.
Article27. Leslie P, Drinnan MJ, Ford GA, Wilson JA. Swallow respiratory patterns and aging: presbyphagia or dysphagia? J Gerontol A Biol Sci Med Sci. 2005; 60:391–395. PMID: 15860480.
Article28. Sato S, Toyoda K, Uehara T, Toratani N, Yokota C, Moriwaki H, Naritomi H, Minematsu K. Baseline NIH Stroke Scale Score predicting outcome in anterior and posterior circulation strokes. Neurology. 2008; 70:2371–2377. PMID: 18434640.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Location of Brain Lesion and Clinical Factors and Findings of Videofluoroscopic Swallowing Study in Subacute Stroke Patients
- The Effect of Stroke on Pharyngeal Laterality During Swallowing
- Comparison of Swallowing Functions Between Brain Tumor and Stroke Patients
- Dysphagia Pattern according to Stroke Location
- Pattern of Post-Stroke Swallowing Disorder according to the Brain Lesion