Ann Rehabil Med.
2014 Feb;38(1):6-12. 10.5535/arm.2014.38.1.6.
Associating Factors Regarding Nasogastric Tube Removal in Patients With Dysphagia After Stroke
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation and Regional Cardiocerebrovascular Center, Dong-A University Hospital, Busan, Korea. jingee00@naver.com
- KMID: 2266534
- DOI: http://doi.org/10.5535/arm.2014.38.1.6
Abstract
OBJECTIVE
To demonstrate associating factors regarding nasogastric tube (NGT) removal in patients with dysphagia after stroke.
METHODS
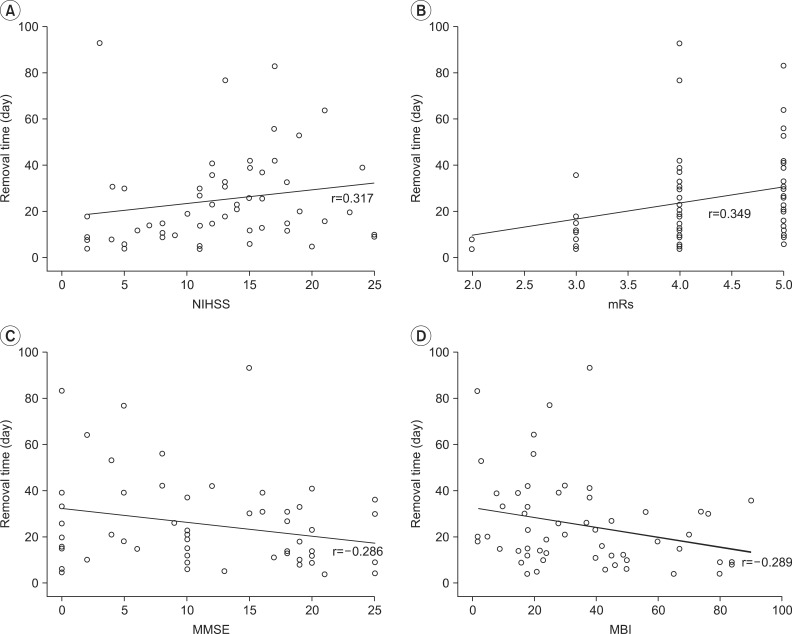
This study is a retrospective medical chart review. Patients were divided into non-brain stem (NBS) and brain stem (BS) groups. A videofluoroscopic swallowing study was conducted until swallowing functions were recovered. Initial disease status was measured using the National Institutes of Health Stroke Scale (NIHSS) and the modified Rankin Scale (mRS). Risk factors related to stroke were evaluated. The penetration-aspiration scale (PAS) was used as the swallowing test. Functional status was measured by Mini-Mental Status Examination (MMSE) and Modified Barthel Index (MBI). Within each group, initial evaluations and their subsequent changes were compared according to the NGT removal status. Correlation between the NGT removal time and other initial factors were evaluated.
RESULTS
Ninety-nine patients were allocated to the NBS group and 39 to the BS group. In NBS, age, PAS, MMSE, and MBI were significantly different according to the NGT removal status. In BS, smoking and PAS were significantly different. In NBS, changes in PAS, MMSE, and MBI were significantly different according to the NGT removal status. In BS, only PAS change was significantly different. In NBS, initial NIHSS, mRS, MMSE, and MBI were correlated with removal time.
CONCLUSION
In stroke patients with NTG, younger age, better initial disease and functional status seems to remove NGT in NBS stroke. Therefore, when deciding to remove NGT, those three factors should be considered discreetly.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Factors Associated With Successful Gastrostomy Tube Weaning in Patients With Prolonged Dysphagia After Stroke
Bo Seong Jang, Jun Young Park, Jae Hyun Lee, Young Joo Sim, Ho Joong Jeong, Ghi Chan Kim
Ann Rehabil Med. 2021;45(1):33-41. doi: 10.5535/arm.20149.
Reference
-
1. Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. Br Med J (Clin Res Ed). 1987; 295:411–414.
Article2. Horner J, Massey EW, Riski JE, Lathrop DL, Chase KN. Aspiration following stroke: clinical correlates and outcome. Neurology. 1988; 38:1359–1362. PMID: 3412582.
Article3. Barer DH. The natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry. 1989; 52:236–241. PMID: 2564884.
Article4. Horner J, Buoyer FG, Alberts MJ, Helms MJ. Dysphagia following brain-stem stroke: clinical correlates and outcome. Arch Neurol. 1991; 48:1170–1173. PMID: 1953404.5. Mann G, Hankey GJ, Cameron D. Swallowing disorders following acute stroke: prevalence and diagnostic accuracy. Cerebrovasc Dis. 2000; 10:380–386. PMID: 10971024.
Article6. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke: does dysphagia matter? Stroke. 1996; 27:1200–1204. PMID: 8685928.7. Paciaroni M, Mazzotta G, Corea F, Caso V, Venti M, Milia P, et al. Dysphagia following stroke. Eur Neurol. 2004; 51:162–167. PMID: 15073441.
Article8. Kalra L, Smith DH, Crome P. Stroke in patients aged over 75 years: outcome and predictors. Postgrad Med J. 1993; 69:33–36. PMID: 8446547.
Article9. Schmidt J, Holas M, Halvorson K, Reding M. Videofluoroscopic evidence of aspiration predicts pneumonia and death but not dehydration following stroke. Dysphagia. 1994; 9:7–11. PMID: 8131429.
Article10. Smithard DG, Smeeton NC, Wolfe CD. Long-term outcome after stroke: does dysphagia matter? Age Ageing. 2007; 36:90–94. PMID: 17172601.
Article11. Gomes CA Jr, Lustosa SA, Matos D, Andriolo RB, Waisberg DR, Waisberg J. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst Rev. 2012; 3:CD008096. PMID: 22419328.12. Dennis MS, Lewis SC, Warlow C. FOOD Trial Collaboration. Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): a multicentre randomised controlled trial. Lancet. 2005; 365:764–772. PMID: 15733717.13. Wang TG, Wu MC, Chang YC, Hsiao TY, Lien IN. The effect of nasogastric tubes on swallowing function in persons with dysphagia following stroke. Arch Phys Med Rehabil. 2006; 87:1270–1273. PMID: 16935066.
Article14. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999; 30:744–748. PMID: 10187872.15. Ros L, Garcia M, Prat J, Gonzalez C, Gimeno C, Albert A, et al. Predictors of nosocomial infection in acute stroke: relation with morbimortality and outcome. Med Clin (Barc). 2007; 128:441–447. PMID: 17408536.16. Oto T, Kandori Y, Ohta T, Domen K, Koyama T. Predicting the chance of weaning dysphagic stroke patients from enteral nutrition: a multivariate logistic modelling study. Eur J Phys Rehabil Med. 2009; 45:355–362. PMID: 19238132.17. Ickenstein GW, Stein J, Ambrosi D, Goldstein R, Horn M, Bogdahn U. Predictors of survival after severe dysphagic stroke. J Neurol. 2005; 252:1510–1516. PMID: 16136260.
Article18. Mann G, Hankey GJ. Initial clinical and demographic predictors of swallowing impairment following acute stroke. Dysphagia. 2001; 16:208–215. PMID: 11453569.
Article19. Remesso GC, Fukujima MM, Chiappetta AL, Oda AL, Aguiar AS, Oliveira Ade S, et al. Swallowing disorders after ischemic stroke. Arq Neuropsiquiatr. 2011; 69:785–789. PMID: 22042182.
Article20. Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010; 8:917–932. PMID: 20602553.
Article21. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.22. Teismann IK, Suntrup S, Warnecke T, Steinstrater O, Fischer M, Floel A, et al. Cortical swallowing processing in early subacute stroke. BMC Neurol. 2011; 11:34. PMID: 21392404.
Article23. Okubo PC, Fabio SR, Domenis DR, Takayanagui OM. Using the National Institute of Health Stroke Scale to predict dysphagia in acute ischemic stroke. Cerebrovasc Dis. 2012; 33:501–507. PMID: 22538772.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Self-Knotting of Nasogastric Tube in a Stroke Patient with Dysphagia: A Case Report
- The Effect of Nasogastric Tube on Swallowing Function in Stroke Patients with Dysphagia
- Gastroesophageal Reflux during Nasogastric Tube Feeding versus Oroesophageal Tube Feeding in Stroke Patients: A 24 Hour Esophageal pH-monitoring
- Comparison of Percutaneous Endoscopic Gastrostomy and Nasogastric Tube Feeding in Dysphagic Stroke
- The Phenomenological Study on the Experiences of Nasogastric Tube Feeding among Cerebral Stoke Patients with Dysphagia