Allergy Asthma Immunol Res.
2010 Apr;2(2):114-122. 10.4168/aair.2010.2.2.114.
Beta-Lactam Antibiotic Sensitization and Its Relationship to Allergic Diseases in Tertiary Hospital Nurses
- Affiliations
-
- 1Allergy Division of Internal Medicine, Chonnam National University Hospital, Gwangju, Korea. ischoi@chonnam.ac.kr
- 2Department of Nurse, Chonnam National University Hospital, Gwangju, Korea.
- 3Department of Dermatology, Chonnam National University Hospital, Gwangju, Korea.
- KMID: 2260597
- DOI: http://doi.org/10.4168/aair.2010.2.2.114
Abstract
- PURPOSE
Skin allergies through type 1 and 4 hypersensitivity reactions are the most frequent manifestations of drug allergies. We had previously experienced a case of a nurse with cefotiam-induced contact urticaria syndrome. To aid in preventing the progression of drug-induced allergic disease in nurses, we conducted a survey of tertiary hospital nurses who were likely to have been exposed professionally to antibiotics.
METHODS
All 539 staff nurses at a tertiary hospital were asked to respond to a questionnaire regarding antibiotic exposure. Of the 457 nurses (84.8%) who responded, 427 (79.2%) received a physical examination of the hands and 318 (59.0%) received skin prick tests with the beta-lactam antibiotics cefotiam, cefoperazone, ceftizoxime, flomoxef, piperacillin and penicillin G.
RESULTS
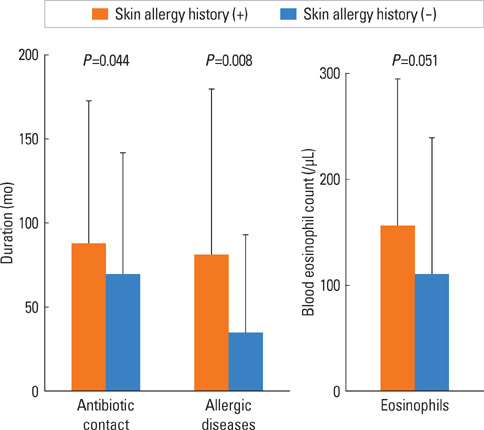
A positive response to at least one of the antibiotics occurred in 8 (2.6%) of the 311 subjects included in the analysis and stages 1 and 2 contact urticaria syndrome were observed in 38 (8.9%) and 3 (0.7%) of 427 nurses, respectively. The frequencies of a positive antibiotic skin test (6.9 versus 1.3%, chi-square=7.15, P=0.018), stage 1 contact urticaria syndrome (14.4 versus 7.4%, chi-square=4.33, P=0.038) and drug allergy (15.3 versus 3.6%, chi-square=18.28, P=0.000) were higher in subjects with a positive skin allergy history than in those without. Allergic rhinitis (P=0.02, OR=3.86, CI=1.23-12.06), night cough (P=0.04, OR=3.12, CI=1.03-9.41) and food allergy (P=0.00, OR=9.90, CI=3.38-29.98) were significant risk factors for drug allergy.
CONCLUSIONS
Antibiotic sensitization and drug allergy occurred more frequently in nurses with a positive skin allergy history. Atopy may be an important risk factor for drug allergy.
MeSH Terms
-
Anti-Bacterial Agents
Cefoperazone
Cefotiam
Ceftizoxime
Cephalosporins
Cough
Drug Hypersensitivity
Food Hypersensitivity
Hand
Hypersensitivity
Penicillin G
Physical Examination
Piperacillin
Rhinitis
Rhinitis, Allergic, Perennial
Risk Factors
Skin
Skin Tests
Tertiary Care Centers
Urticaria
Surveys and Questionnaires
Anti-Bacterial Agents
Cefoperazone
Cefotiam
Ceftizoxime
Cephalosporins
Penicillin G
Piperacillin
Figure
Cited by 1 articles
-
Usefulness of
In Vivo andIn Vitro Diagnostic Tests in the Diagnosis of Hypersensitivity Reactions to Quinolones and in the Evaluation of Cross-Reactivity: A Comprehensive Study Including the Latest Quinolone Gemifloxacin
Semra Demir, Asli Gelincik, Nilgun Akdeniz, Esin Aktas-Cetin, Muge Olgac, Derya Unal, Belkis Ertek, Raif Coskun, Bahattin Colakoğlu, Gunnur Deniz, Suna Buyukozturk
Allergy Asthma Immunol Res. 2017;9(4):347-359. doi: 10.4168/aair.2017.9.4.347.
Reference
-
1. Gomes ER, Demoly P. 111 Epidemiology of hypersensitivity drug reactions. Curr Opin Allergy Clin Immunol. 2005. 5:309–316.2. Çelik G, Pichler WJ, Adkinson NF Jr. Adkinson NF, Bochner BS, Busse WW, Holgate ST, Lemanske RF, Simons FER, editors. Drug allergy. Middleton's allergy. Principles and practice. 2009. 7th ed. Philadelphia: Mosby Elsevier;1205–1226. .3. Schnyder B. Approach to the patient with drug allergy. Immunol Allergy Clin N Am. 2009. 29:405–418.4. Romano A, Demoly P. Recent advances in the diagnosis of drug allergy. Curr Opin Allergy Clin Immunol. 2007. 7:299–303.5. DeSwarte RD, Patterson R. Patterson R, Grammer LC, Greenberger PA. Drug allergy. Allergic diseases. 1997. 5th ed. Philadelphia: Lippincott-Raven;317–412.6. Lee KH, Choi IS, Lee WJ, Kang SJ, Jeong HK. A case of cefotiam-contact anaphylaxis. Korean J Med. 2009. 76:Suppl 1. S238–S242. Korean.7. Tadokoro K, Niimi N, Ohtoshi T, Nakajima K, Takafuji S, Onodera K, Suzuki S, Muranaka M. Cefotiam-induced IgE-mediated occupational contact anaphylaxis of nurses; case reports, RAST analysis, and a review of the literature. Clin Exp Allergy. 1994. 24:127–133.8. Shimizu S, Chen KR, Miyakawa S. Cefotiam-induced contact urticaria syndrome: an occupational condition in Japanese nurses. Dermatology. 1996. 192:174–176.9. Shin KY, Lee JY, Park CW, Lee CH. A case of cefotiam-induced contact urticaria syndrome. Korean J Dermatol. 1998. 36:1092–1095. Korean.10. Shin HJ, Kim WS, Lee SY, Lee JS, Whang KU. A case of cefotiam-induced contact urticaria syndrome. Korean J Dermatol. 2005. 43:131–133. Korean.11. Jang PM, Kim HJ, Kim YS, Cho YS, Lee JW, Yu KW, Lim H. Two cases of contact urticaria syndrome from cefotiam in nurses. J Korean Soc Clin Toxicol. 2006. 4:65–68.12. Lee JY, Kim GI, Park CW, Lee CH. Two cases of cefotiam-induced contact urticaria syndrome. Ann Dermatol. 2000. 12:119–121.13. Choi HJ, Song JY, Park YM, Kim CW, Kim HO. Occupational contact urticaria syndrome induced by cefotiam dihydrochloride in a nurse. Ann Dermatol. 2003. 15:113–115.14. Jeong J, You K, Nahm S, Kim E. Anaphylaxis after epidermal contact with cefotiam hydrochloride. J Allergy Clin Immunol. 2006. 117:S227.15. NIH Publication No. 97-4051. Expert panel report 3: guidelines for the diagnosis and management of asthma. Full Report 2007. 2007. Bethesda, MD: U.S. Department of Health and Human Services; National Institutes of Health; National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program.16. Demoly P, Kropf R, Bircher A, Pichler WJ. Drug hypersensitivity: questionnaire. EAACI interest group on drug hypersensitivity. Allergy. 1999. 54:999–1003.17. Von Krogh G, Maibach HI. The contact urticaria syndrome-an updated review. J Am Acad Dermatol. 1981. 5:328–342.18. Gober MD, DeCapite TJ, Gaspari AA. Adkinson NF, Bochner BS, Busse WW, Holgate ST, Lemanske RF, Simons FER, editors. Contact dermatitis. Middleton's allergy. Principles and practice. 2009. 7th ed. Philadelphia: Mosby Elsevier;1105–1116.19. Barbaud A, Goncalo M, Bruynzeel D, Bircher A. Guidelines for performing skin tests with drugs in the investigation of cutaneous adverse drug reactions. Contact Dermatitis. 2001. 45:321–328.20. Adinoff AD, Rosloniec DM, McCall LL, Nelson HS. Immediate skin test reactivity to Food and Drug Administration-approved standardized extracts. J Allergy Clin Immunol. 1990. 86:766–774.21. Gomes E, Cardoso MF, Praca F, Gomes L, Marino E, Demoly P. Self-reported drug allergy in a general adult Portuguese population. Clin Exp Allergy. 2004. 34:1597–1601.22. Solley GO, Gleich GJ, Van Dellen RG. Penicillin allergy: clinical experience with a battery of skin-test reagents. J Allergy Clin Immunol. 1982. 69:238–244.23. Raja AS, Lindsell CJ, Bernstein JA, Codispoti CD, Moellman JJ. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Ann Emerg Med. 2009. 54:72–77.24. Sullivan TJ, Wedner HJ, Shatz GS, Yecies LD, Parker CW. Skin testing to detect penicillin allergy. J Allergy Clin Immunol. 1981. 68:171–180.25. You HS, So HS. A study on the prevalence of dermatitis and allergic reactions to medicine & disinfectant used by nurses. Chonnam J Nurs Sci. 2002. 7:19–34.26. Polk RE, Healy DP, Schwartz LB, Rock DT, Garson ML, Roller K. Vancomycin and the red-man syndrome: pharmacodynamics of histamine release. J Infect Dis. 1988. 157:502–507.27. Barbaud A, Reichert-Penetrat S, Trechot P, Jacquin-Petit MA, Ehlinger A, Noirez V, Faure GC, Schmutz JL, Bene MC. The use of skin testing in the investigation of cutaneous adverse drug reactions. Br J Dermatol. 1998. 139:49–58.28. Madaan A, Li JT. Cephalosporin allergy. Immunol Allergy Clin North Am. 2004. 24:463–476. vi–vii.29. Kim SH, Choi IS, Lee S, Jung SH, Seo SR, Mun JS, Han ER. A case of cold urticaria with exercise- and cold-induced anaphylaxis. Chonnam Med J. 2006. 42:140–143. Korean.30. Seo E, Yoon TY, Jung JS, Jang EJ, Choi W, Kim MK. A case of contact urticaria syndrome induced by cefotiam and imipenem in atopic dermatitis patient. Korean J Asthma Allergy Clin Immunol. 2009. 29:217–220. Korean.31. Adkinson NF Jr. Risk factors for drug allergy. J Allergy Clin Immunol. 1984. 74:567–572.32. Apter AJ, Schelleman H, Walker A, Addya K, Rebbeck T. Clinical and genetic risk factors of self-reported penicillin allergy. J Allergy Clin Immunol. 2008. 122:152–158.33. Schnuch A, Brasch J, Uter W. Polysensitization and increased susceptibility in contact allergy: a review. Allergy. 2008. 63:156–167.34. Empedrad R, Darter AL, Earl HS, Gruchalla RS. Nonirritating intradermal skin test concentrations for commonly prescribed antibiotics. J Allergy Clin Immunol. 2003. 112:629–630.35. Park MA, Matesic D, Markus PJ, Li JT. Female sex as a risk factor for penicillin allergy. Ann Allergy Asthma Immunol. 2007. 99:54–58.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between beta-Lactam Antimicrobial Use and Antimicrobial resistance in Klebsiella pneumoniae Clinical Isolates at 5 Tertiary Hospitals in Korea
- Community Acquired Pneumonia
- Allergen sensitization trajectories in children with respiratory and allergic diseases
- Beta-Lactam Allergy and Cross-Reactivity
- Trends in Allergic Sensitization and Diseases in the Korean General Population Over a 9-Year Period