Korean Circ J.
1974 Jun;4(1):43-55. 10.4070/kcj.1974.4.1.43.
A Study on the Use of the Electrocardiogram for Diagnostic Evaluation of Patients with Mitral Valvular Disease
- KMID: 2229710
- DOI: http://doi.org/10.4070/kcj.1974.4.1.43
Abstract
- Electrocardiography has been long an important tool in cardiac diagnosis and, with advances in electrocardiography, the accuracy of the electrocardiographic diagnosis has been greatly increased. Though the most accurate methods for quantitative diagnosis of mitral valvular disease are cardiac catheterization and ventriculography, these procedures are time consuming, expensive, and not without risk, thus, it would be helpful if routine catheterization of the heart could be avoided in patients who are potential condidates for mitral valvulotomy. This could be done if reliable electrocardiographic criteria could be found for estimating the amount of obstrcution and leak at the mitral valve. As mitral valvular dysfunction progress, changes (hypertrophy and/or dilation) in the left atrium and both ventricles are inevitable. Many authors attempted to characterize the electrocardiographic findings of such changes according to the specific lesion of the mitral valve. In addition to atrial fibrillation, characteristic P wave changes and their diagnostic significance have been reported (Macruz et al., 1958; Arevalo et al., 1963: Morris et al., 1964). The diagnostic importance of QRS voltage difference in precordial leads has been stressed in the differential diagnosis of specific lesions of mitral valvular disease (Janton et al., 1954: Bateman and January, 1955: Wierum and Glenn, 1957: Bentivoglio et al., 1958: Imperial et al., 1960). Semle and Pruitt(1960) reported that a mean QRS electrical axis of +91degrees or more degrees was the most frequent positive single index of increased total pulmonary resistance in mitral stenosis, and Fowler et al. (1955) stated that precordial lead V1 was very helpful in evaluating the degree of pulmonary hypertension. In Korea there are only a few reports on the electrocardiographic changes in mitral valvular disease and the correlation of electrocardiographic findings and hemodynamics (Oh et al., 1961: Kim, 1970: Kim, 1971). It would be evident that the various electrocardiographic findings noted in western races can't be applied to Koreans. The main objectives of this study are: 1. To determine the electrocardiographic characteristics of pure mitral valvular disease and the differentiation between the specific lesions of pure mitral stenosis, pure mitral insufficiency and combined lesions of mitral stenosis and insufficiency. 2. To know whether the characteristic electrocardiographic changes of mitral stenosis are directly related to the narrowed valve area or to the hemodynamic abnormalities secondary to obstruction.
SUBJECTS AND METHODS
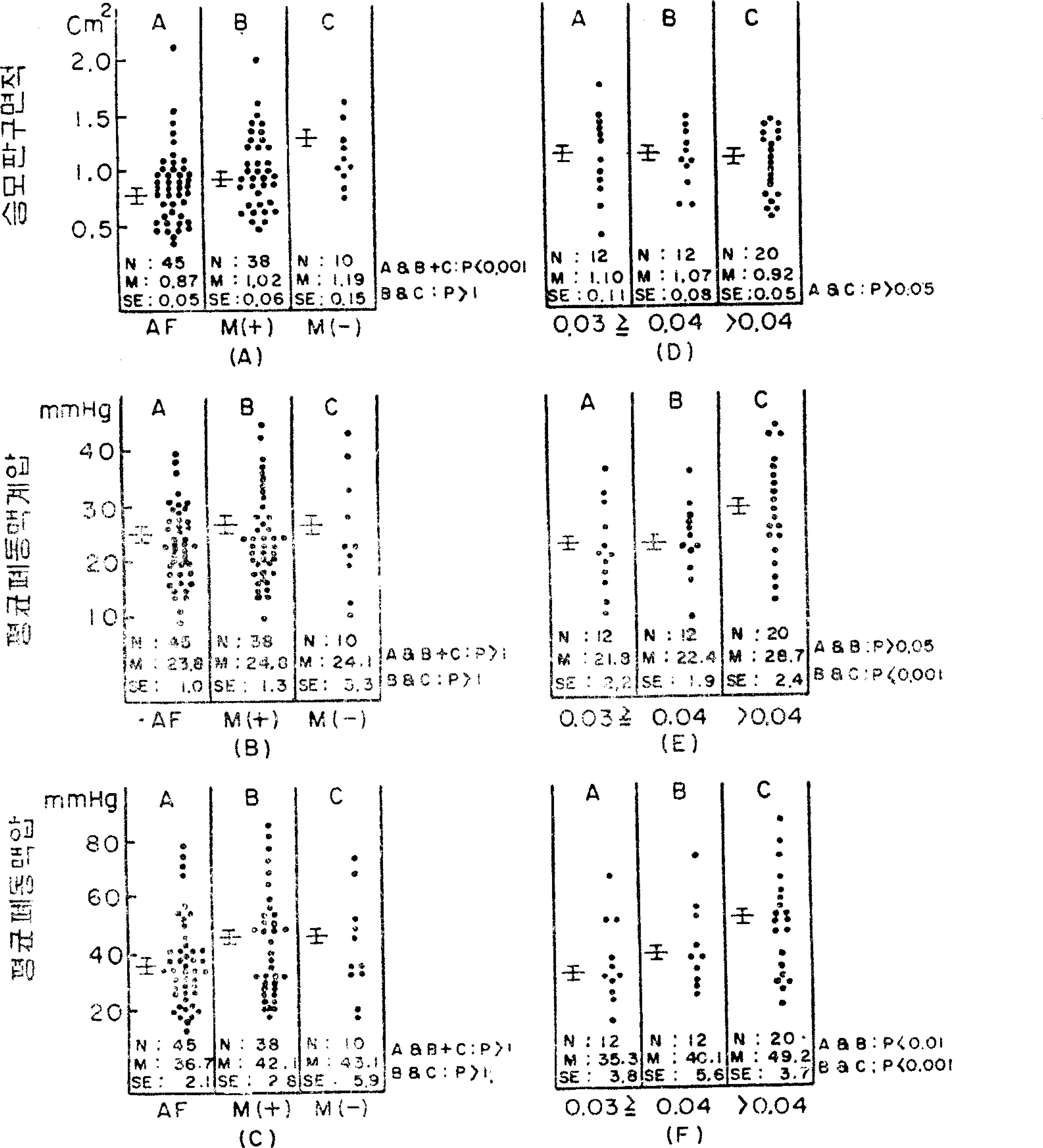
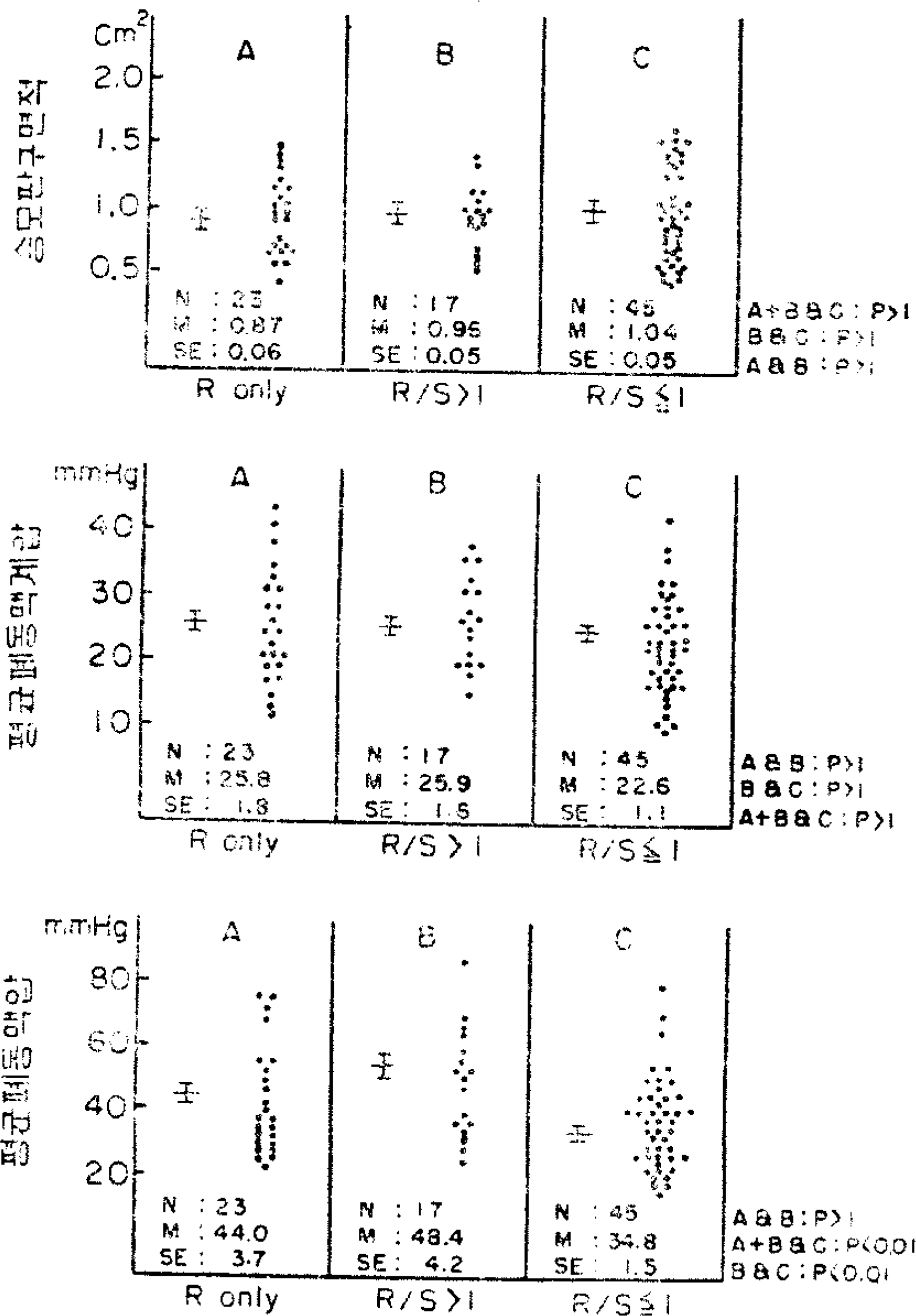
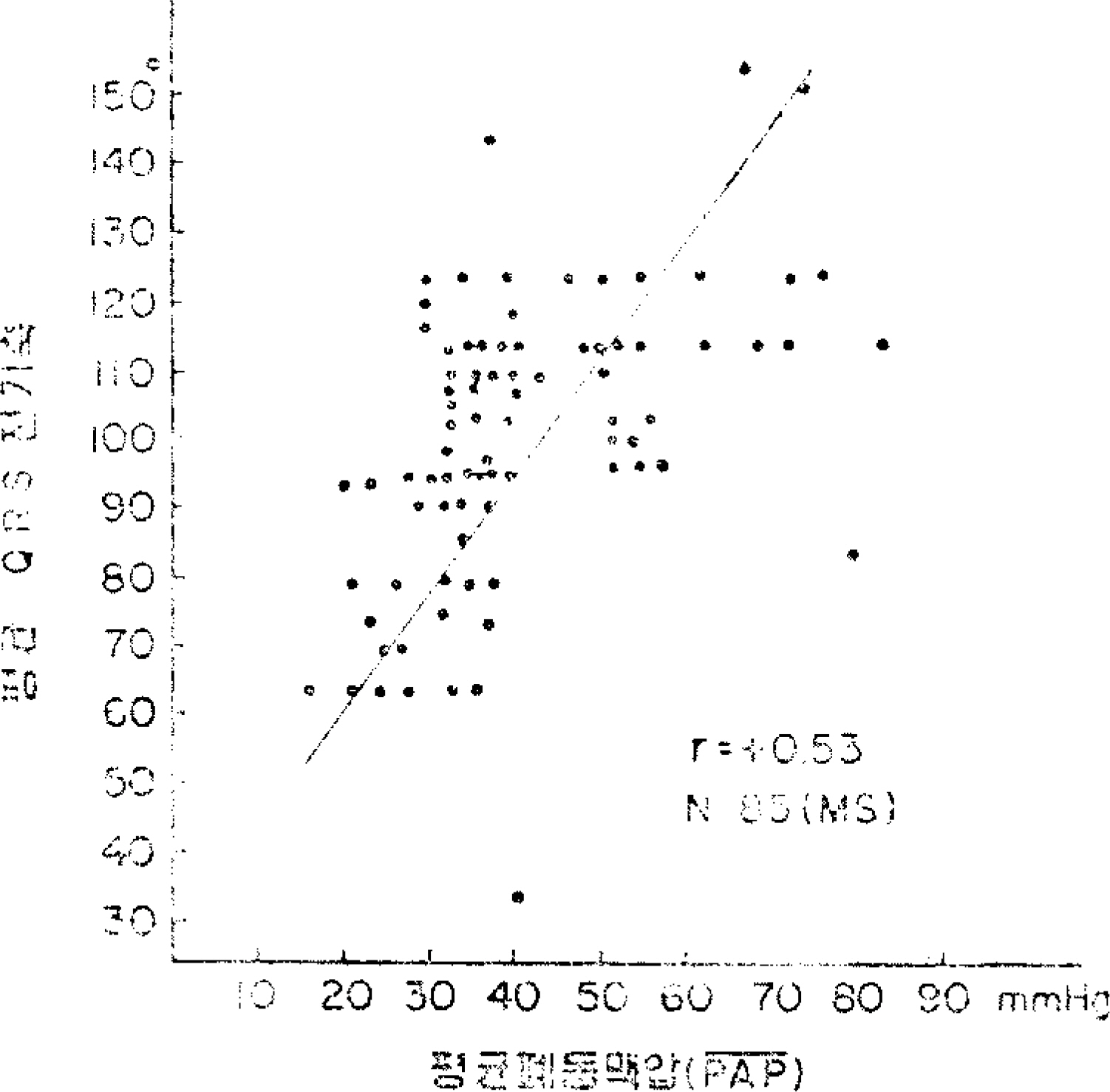
139 cases of isolated mitral valvular disease were reviewed: of these 93 were cases of pure mitral stenosis, 18 were pure mitral insufficiency, and 28 were combined mitral stenosis and insufficiency. Of the total patients, 68 were male and 71 were female. The ages ranged from 10 to 54 years with an average of 35.6 years. Diagnosis was based on cardiac catheterization and supplemented by cienangiocardiography. The conventional 12 lead electrocardiogram was taken at normal sensitivity and at a paper speed of 25mm/sec. The mitral valve area was estimated according to the Gorlin's formula and cardiac output was determined by the direct Fick's principle. The electrocardiograms were analyzed with respect to: 1. Rhythm (atrial fibrillation and sinus rhythm) 2. Presence or absence of P-mitrale 3. Terminal P force in lead V1 (by the method of Morris et. al., 1964) 4. Mean QRS electrical axis in frontal plane 5. QRS voltage in percordial leads(V1S, V5R, V6R & V1S+V(5-6)R) 6. R/S ratio in lead V1 7. Conduction disturbance of right bundle branch block In patients with pure mitral stenosis the electrocardiographic findings of atrial fibrillation P-mitrale, terminal P force in lead V1 were correlated with the hemodynamic data of mean pulmonary artery pressure, mean pulmonary arterial wedge pressure and mitral valve area. An attempt was made to ascertain whether or not a quantitative correlation could be found. A patient showing electrocardiographic pattern of right bundle branch block was excluded in the evaluation of QRS voltage in lead V1 and mean QRS electrical axis in frontal plane.
RESULTS
AND SUMMARY: 1. P wave abnormality, which was noted in most (131/139) cases, is apparently a characteristic and most frequent electrocardiographic finding in mitral valvular disease. Of the P weve abnormalities the development of atrial fibrillation and P-mitrale were thought to be related to the duration of the illness rather than to the types of lesion or hemodynamic abnormalities secondary to valvular dysfunction. However, the terminal P force in lead V1 was thought to be related to the mean pulmonary arterial wedge pressure rather than to narrowing of the valve. 2. 15 patients showed the electrocardiographic pattern of right bundle branch block. In patients with mitral stenosis this electrocardiographic pattern was noted at almost all levels of mean pulmonary artery pressure, mean pulmonary arterial wedge pressure, mitral gradient and mitral valve area. 3. Mean QRS electrical axis and QRS voltage in precordial leads; There was no case which deviated leftward more than +30degrees even among cases with a predominant or pure mitral insufficiency. Although the difference of mean value in mean QRS electrical axis and QRS voltage in precordial leads according to the types of the lesion was significant, this difference was generally not helpful in the differential diagnosis in individual patients because of much overlapping among cases. 4. There was no definite electrocardiographic criteria to differentiate clearly the types of mitral valvular disease. However, the following aspects of electrocardiogram may be useful in differential diagnosis. a. Difference of QRS voltage in precordial leads: The volage of V1S and V1S+V(5-6)R in all patients with pure mitral insufficiency was over 1mm and 11mm respectively. That of V1S+V(5-6)R in all patients with pure mitral stenosis was below 39mm. b. R/S ratio in lead V1: There was no case showing "R wave only" in lead V1 among patients with pure or predominant mitral insufficiency. c. Mean QRS electrical axis in frontal plane: The mean QRS electrical axis of all patients with pure mitral stenosis deviated rightward more than +60degrees in all except one case. None of the patients with pure mitral insufficiency deviated rightward more than +110degrees. 5. Relationship between hemodynamics and electrocardiography in paitents with mitral stenosis: Among the hemodynamic abnormalities, mean pulmonary artery pressure showed a close relationship with the following aspects of the electrocardiogram. a. R/S ratio in lead V1:The mean value of mean pulmonary artery pressure (45.9+/-3.8mmHg) in groups showing R/S>1 was significantly elevated as compared with that (34.8+/-1.5mmHg) of groups showing R/Sdegrees1. b. Mean QRS electrical axis in frontal plane: There was a weak positive correlation (r=+0.53) between mean pulmonary artery prersure and QRS electrical axis in the frontal plane. The QRS axis of all patients with a mean pulmonary artery pressure of 41mmHg or more was +91degrees or more except for one case. c. Terminal P force in lead V1: The difference of mean value in mean pulmonary artery pressure according to the size of terminal P force in lead V1 was significant in all cases.
MeSH Terms
-
Atrial Fibrillation
Axis, Cervical Vertebra
Bundle-Branch Block
Cardiac Catheterization
Cardiac Catheters
Cardiac Output
Catheterization
Catheters
Continental Population Groups
Diagnosis
Diagnosis, Differential
Electrocardiography*
Female
Heart
Heart Atria
Hemodynamics
Humans
Hypertension, Pulmonary
Korea
Male
Mitral Valve
Mitral Valve Insufficiency
Mitral Valve Stenosis
Pulmonary Artery
Pulmonary Wedge Pressure
Figure
Reference
-
1). 서추영. 김인수. 이기환. 김학중. 한국인의심장질환. 대한내과학회잡지. 11:509. 1968.2). 송희승. 이정하•노영무. 박신권■박희문. 이만호서순규. 한국성인심장병의역학직연구. 대한내괴-학회잡지. 15:727. 1972.3). 송정상. 한국인순환기질환의통계적관찰. 대한내과학희잡지. 14:19. 1971.4.송희승•이영.오세용■이범세. 김도전. 장재현이성호. 심방세동의임상직관찰. 대한내과학회잡지. 11:415. 1968.5.Janton O.H.., Heidorn G.., Soloff L.A.., Neili T.J.E.., Glover R.P.The clinical determincticn of mitral insuff iciency ichen associated xvith mitral stenosir. Circulaticn. 10:207. 1554.6). Friedberg C.K.Diseases of the heart. Philadelphia and Lcndcn W.B. Saunders Company;3rd ed.1966.7). Bentivᄋglio L.G.., Uricchio J.F.., Waldow Α.., Likoff W.and Coldberg, H. An electrocardiographic analysis of sixty-five cases cf mitral regurgitation. 18:572. 1958.8). Bateman R.D. Jr.., January L.E.The precordial electrccardiogram in mitral regurgitation. Am. J. Med. 18:415. 1955.9). Berliner K.., Mas'er A.M.Mitral stenosis: A correlaticn of electrocardiographic and pathologic observations. Arch. Int. Med. 61:39. 1938.10). Pruitt R.D.., Robinson J.G.The electrccardiographic findings in patients undergcing surgical explcration of the mitral valve,. Am. Heart. 52:880. 1956.11). Imperial E.S.., Bendezu J.., Zimmermann, H. A. Electrccardicgraphic analysis of pure mitral valvular disease A study based on fifty seven cases zvith ο ρ en-he art operation. Am. Heart: J. 00:705. 1960. ,.12). J. J. Jr.., Estes E.H. Jr.., Whalen R.E.., Thcmpson H.K. Jr.., Mclntcsh H.D.P-wave analysis in valvular heart disease. Circulaticn. 29:242. 1964.13). Fowler N.O.., Noble W.J.., Giarratons S.J.., and Mannix E. P.The clinical estimation of pulmonary hepertension accompanying mitral stenosis. Am. Heart J. 49:237. 1955.14). Semler H.J.., and Pruitt R.D.An electrocardiographic estimaticn of puhncnary vascular obstructicn in 80 patients with mitral stenosis. Am. Heart/. 59:541. 1960.15). 오상진. 석영관. 박회명•이성행•김대수. 승모판협착증의심전도. 대한내과학회잡지, 과: 483,.1961.16). 김도진. 승모판협착증의우심실비대에관한삼전도와X-선의비교관찰, 대한내과학회잡지:_Λ. 3:493. 1970.17). 김연길. 승모판질환의방실비대에관한심전도斗X-선의비교관찰. 대한내과학회잡지:. 1:563. 1971.18). Gcrlin R.., Gorlin S.G.Hydraulic formula for calculation of the area of the stenotic mitral valve, other cardiac valves, and general circulatory shunts,. I. Am. Heart/. 41:1. 1955.19). Selzer Α.Effects of atrial fibrillation upon the circulation in patients mith mitral stenosis. Am. Heart J. 59:518. 1960.20). Abildkov J.A.., Millar J.., Burgess M.J.Atrial fibrillation. Am. J. Cardiol. 28:263. 1971.21). Lewis B.B.M.., Golin R.., Houssay H.E.J.., Haynes F.W.., Dexter L.Clinical and physiologic correlation in patients with mitral stenosis,. V. Am. Heart/. 43:2. 1952.22). Hugenholtz P.G.., Ryan T.J.., Stein S.W.., Abelmann W.H.The spectrum of pure mitral stenosis: Ή em odyn am ic studies in relation to clinical disability. Asm. 'L Cardiol. 10:773. 1962.23). Wierum C.., Glenn F.Electrocardiographic indications of significant mitral insufficiency in patients with mitral valve disease. Am. Heart. 53:359. 1957.24). Brigden W.Leatham A.Brit. Heart J.f. 15:55. 1953. (sited from Wierum and Glenn, 1957).25). Hurst J.W.., Logue R.B.The heart. McGrazv Hill Bock Co???pany;2nd ed.1970.26). Macruz R.., Perloff J.K.., Case R.B.A method for the electrocardiograpic recognition of atrial enlargement. Circulation. 17:882. 1958.27). Arevalo A.C.., Spagnuolo M.., and Feinstein A.R.A simple electrocardiographic indication of left atrial enlargement: A study of young patients with rheumatic heart disease. JAMA. 185:358. 1963.28). Cosby R.S.., Levinson D.C.., Dimitroff S.P.».., Oblath R.W.., Herman L.M.., Griffith G.C.The electrocardiogram in congenital heart disease and mitral stenosis. Am. Heart/. 46:670. 1953.29). Janton O.H.., Glover R.P.., O'Neill T.J.E.Indications for commissurotomy in mitral stenosis. Am. J. Med. 12:621. 1952.30). Fraser H.RT.., Turner R.Electrocardiography in mitral valvular disease. Brit. Heart J. 17:459. 1955. {cited from Hust and Logue, 197 (f).31). 서순규. 한국인심전도에관한연구. 항공의학. 3:4–5. 1955.32). 이성호. 정상심전도에관한연구. 대한내과학회잡지. 3:555. 1960.33). 박윤진. 건강한국인의심전도에서보는심실비대상에관하여. 대한내과학회잡지'. 5:1. 1962.34). Kossmann C.E.The normal electrocardiogram. Circulation. 8:920. 1953.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relation between Left Atrial Size and Atrial Fibrillation
- Silent Aortic Regurgitation
- Familial mitral valve prolapse in a Maltese dog family
- The Relationship of Mitral Valve Area Measured by 2-Dimensional Echocardiography with the M-Mode Measurements in Mitral Valvular Stenosis
- Echocardiographic Studies on Mitral Valvular Heart Disease