Korean J Crit Care Med.
2014 Nov;29(4):281-287. 10.4266/kjccm.2014.29.4.281.
Comparison of Morphine and Remifentanil on the Duration of Weaning from Mechanical Ventilation
- Affiliations
-
- 1Department of Surgery, Ajou University School of Medicine, Suwon, Korea.
- 2Department of Anesthesiology and Pain Medicine, Chonnam National University, Medical School, Gwangju, Korea.
- 3Division of Pulmonology, Critical Care and Sleep Medicine, Department of Internal Medicine, St. Paul's Hospital, The Catholic University of Korea, Seoul, Korea.
- 4Department of Pulmonology, Kangreung Asan Medical Center, Kangreung, Korea.
- 5Department of Anesthesiology and Pain Medicine, Hanyang University school of Medicine, Seoul, Korea.
- 6Department of Anesthesiology and Pain Medicine, Ajou University School of Medicine, Suwon, Korea.
- 7University of Ulsan, College of Medicine, Asan Medical Center, Seoul, Korea. cmlim@amc.seoul.kr
- KMID: 2227735
- DOI: http://doi.org/10.4266/kjccm.2014.29.4.281
Abstract
- BACKGROUND
A randomized, multicenter, open-label, parallel group study was performed to compare the effects of remifentanil and morphine as analgesic drugs on the duration of weaning time from mechanical ventilation (MV).
METHODS
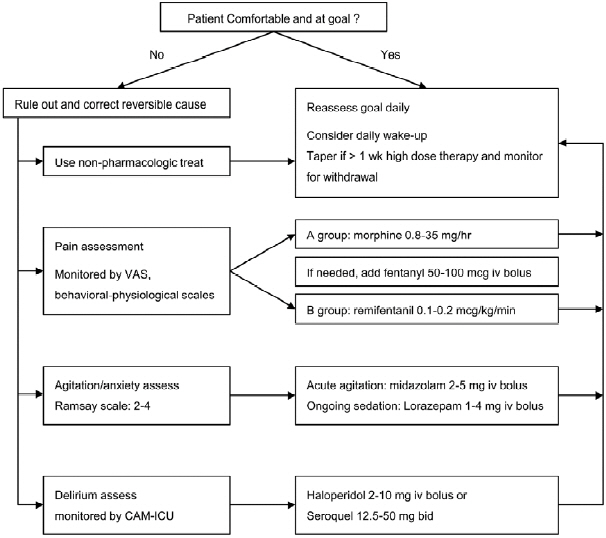
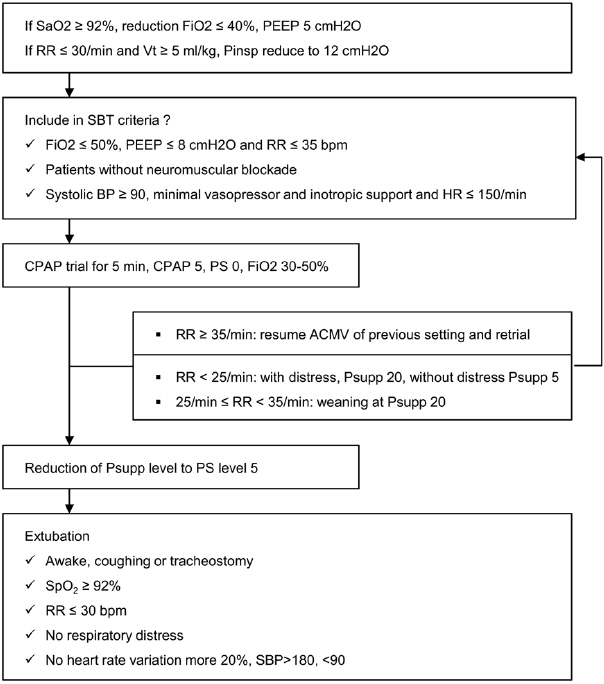
A total of 96 patients with MV in 6 medical and surgical intensive care units were randomly assigned to either, remifentanil (0.1-0.2 mcg/kg/min, n = 49) or morphine (0.8-35 mg/hr, n = 47) from the weaning start. The weaning time was defined as the total ventilation time minus the sum of controlled mode duration.
RESULTS
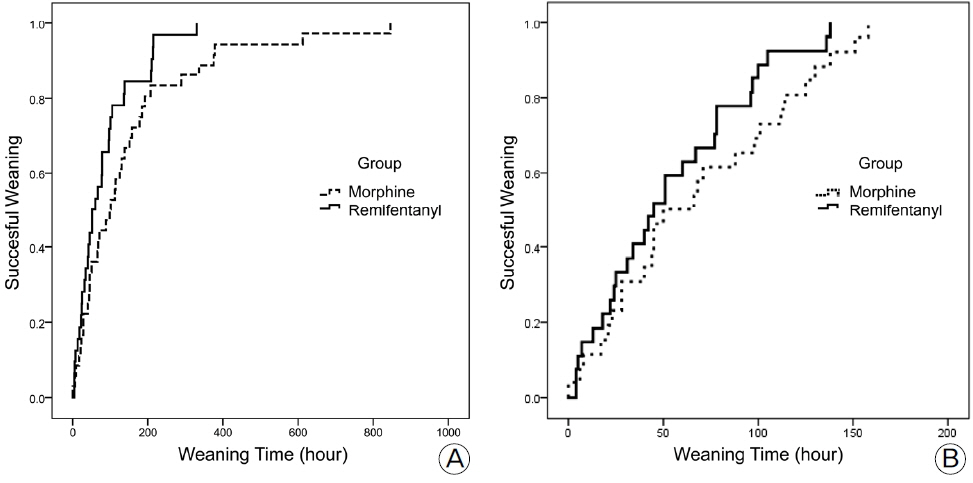
Compared with the morphine group, the remifentanil-based analgesic group showed a tendency of shorter weaning time (mean 143.9 hr, 89.7 hr, respectively: p = 0.069). Secondary outcomes such as total ventilation time, successful weaning rate at the 7th of MV day was similar in both groups. There was also no difference in the mortality rate at the 7th and 28th hospital day. Kaplan-Meyer curve for weaning was not different between the two groups.
CONCLUSIONS
Remifentanil usage during the weaning phase tended to decrease weaning time compared with morphine usage.
MeSH Terms
Figure
Reference
-
References
1). Breen D, Karabinis A, Malbrain M, Morais R, Albrecht S, Jarnvig IL, et al. Decreased duration of mechanical ventilation when comparing analgesia-based sedation using remifentanil with standard hypnotic-based sedation for up to 10 days in intensive care unit patients: a randomised trial [ISRCTN47583497]. Crit Care. 2005; 9:R200–10.2). Rozendaal FW, Spronk PE, Snellen FF, Schoen A, van Zanten AR, Foudraine NA, et al. Remifentanil-propofol analgo-sedation shortens duration of ventilation and length of ICU stay compared to a conventional regimen: a centre randomised, cross-over, open-label study in the Netherlands. Intensive Care Med. 2009; 35:291–8.
Article3). Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013; 41:263–306.
Article4). Payen JF, Chanques G, Mantz J, Hercule C, Auriant I, Leguillou JL, et al. Current practices in sedation and analgesia for mechanically ventilated critically ill patients: a prospective multicenter patient-based study. Anesthesiology. 2007; 106:687–95. quiz 891–2.5). Egan TD, Lemmens HJ, Fiset P, Hermann DJ, Muir KT, Stanski DR, et al. The pharmacokinetics of the new short-acting opioid remifentanil (GI87084B) in healthy adult male volunteers. Anesthesiology. 1993; 79:881–92.
Article6). Shapiro BA, Warren J, Egol AB, Greenbaum DM, Jacobi J, Nasraway SA, et al. Practice parameters for intravenous analgesia and sedation for adult patients in the intensive care unit: an executive summary. Society of Critical Care Medicine. Crit Care Med. 1995; 23:1596–600.7). Trescot AM, Datta S, Lee M, Hansen H. Opioid pharmacology. Pain Physician. 2008; 11(2 Suppl):S133–53.
Article8). Michelsen LG, Hug CC Jr. The pharmacokinetics of remifentanil. J Clin Anesth. 1996; 8:679–82.
Article9). Kapila A, Glass PS, Jacobs JR, Muir KT, Hermann DJ, Shiraishi M, et al. Measured context-sensitive half-times of remifentanil and alfentanil. Anesthesiology. 1995; 83:968–75.
Article10). Pitsiu M, Wilmer A, Bodenham A, Breen D, Bach V, Bonde J, et al. Pharmacokinetics of remifentanil and its major metabolite, remifentanil acid, in ICU patients with renal impairment. Br J Anaesth. 2004; 92:493–503.11). Steinlechner B, Dworschak M, Birkenberg B, Lang T, Schiferer A, Moritz A, et al. Low-dose remifentanil to suppress haemodynamic responses to noxious stimuli in cardiac surgery: a dose-finding study. Br J Anaesth. 2007; 98:598–603.
Article12). Glass PS, Hardman D, Kamiyama Y, Quill TJ, Marton G, Donn KH, et al. Preliminary pharmacokinetics and pharmacodynamics of an ultra-short-acting opioid: remifentanil (GI87084B). Anesth Analg. 1993; 77:1031–40.13). Muellejans B1, López A, Cross MH, Bonome C, Morrison L, Kirkham AJ. Remifentanil versus fentanyl for analgesia based sedation to provide patient comfort in the intensive care unit: a randomized, double-blind controlled trial [ISRCTN43755713]. Crit Care. 2004; 8:R1–R11.14). Dahaba AA, Grabner T, Rehak PH, List WF, Metzler H. Remifentanil versus morphine analgesia and sedation for mechanically ventilated critically ill patients: a randomized double blind study. Anesthesiology. 2004; 101:640–6.15). Wang JY, Winship SM, Thomas SD, Gin T, Russell GN. Induction of anaesthesia in patients with coronary artery disease: a comparison between sevoflurane-remifentanil and fentanyl-etomidate. Anaesth Intensive Care. 1999; 27:363–8.
Article16). Reid JE, Mirakhur RK. Bradycardia after administration of remifentanil. Br J Anaesth. 2000; 84:422–3.
Article17). Kurdi O, Deleuze A, Marret E, Bonnet F. Asystole during anaesthetic induction with remifentanil and sevoflurane. Br J Anaesth. 2001; 87:943.18). Nooh N, Abdelhalim AA, Abdullah WA, Sheta SA. Effect of remifentanil on the hemodynamic responses and recovery profile of patients undergoing single jaw orthognathic surgery. Int J Oral Maxillofac Surg. 2013; 42:988–93.
Article19). Gesztesi Z, Mootz BL, White PF. The use of a remifentanil infusion for hemodynamic control during intracranial surgery. Anesth Analg. 1999; 89:1282–7.
Article20). Carrer S1, Bocchi A, Candini M, Donegà L, Tartari S. Short term analgesia based sedation in the Intensive Care Unit: morphine vs remifentanil + morphine. Minerva Anestesiol. 2007; 73:327–32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Morphine and Remifentanil on the Duration of Weaning from Mechanical Ventilation
- Weaning Approach with Weaning Index for Postoperative Patients with Mechanical Ventilator Support in the ICU
- Comparison of Initial Weaning Success Rates and Weaning Periods between Synchronized Intermittent Mandatory Ventilation and Pressure Support Ventilation
- Outcomes of patients with COPD requring mechanical ventilation
- The Usefulness of Noninvasive Positive Pressure Ventilation as a New Weaning Method