Korean J Crit Care Med.
2015 May;30(2):103-108. 10.4266/kjccm.2015.30.2.103.
Lung Transplantation in a Patient with Pre-transplant Colonization of Extensively Drug-resistant Acinetobacter baumannii
- Affiliations
-
- 1Division of Respiratory, Allergy and Critical Care, Department of Internal Medicine, The Catholic University of Korea, Seoul, Korea. cmcksc@catholic.ac.kr
- 2Department of Thoracic and Cardiovascular Surgery, St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 3Division of Hematology and Oncology, Catholic Blood and Marrow Transplantation Center, Department of Internal Medicine, St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- KMID: 2227673
- DOI: http://doi.org/10.4266/kjccm.2015.30.2.103
Abstract
- Colonization of the pre-transplant lung by multidrug-resistant bacteria affects short- and long-term outcomes of lung transplantation. However, there are no case reports on the colonization of a pre-transplant lung by drug-resistant Acinetobacter baumannii. We report a case of extensively drug resistant (XDR) A. baumannii colonization in the tracheobronchial tree that caused severe infectious complications after bilateral lung transplantation. A 23-year-old man diagnosed with bronchiolitis obliterans syndrome (BOS) 4 years earlier with a history of allogenic bone marrow transplantation for acute lymphoblastic leukemia was admitted to the hospital with dyspnea. Due to progressive hypercapnic respiratory failure, long-term mechanical ventilation was started after a tracheostomy was performed, and the patient underwent a bilateral lung transplantation to treat end-stage BOS. After the transplantation, the colonization of XDR A. baumannii caused severe bacterial pneumonia in the early postoperative period. Combined treatment with colistin and meropenem led to recovery from the pneumonia but caused drug-induced renal failure. Because many centers are willing to transplant candidates who are on mechanical ventilation or extracorporeal life support, the incidence of XDR A. baumannii colonization of pretransplant lungs is expected to increase. Further studies are needed to examine pre-transplant management strategies in patients colonized with XDR A. baumannii.
MeSH Terms
-
Acinetobacter baumannii*
Bacteria
Bone Marrow Transplantation
Bronchiolitis Obliterans
Colistin
Colon*
Drug Resistance
Dyspnea
Humans
Incidence
Lung
Lung Transplantation*
Pneumonia
Pneumonia, Bacterial
Postoperative Period
Precursor Cell Lymphoblastic Leukemia-Lymphoma
Renal Insufficiency
Respiration, Artificial
Respiratory Insufficiency
Tracheostomy
Young Adult
Colistin
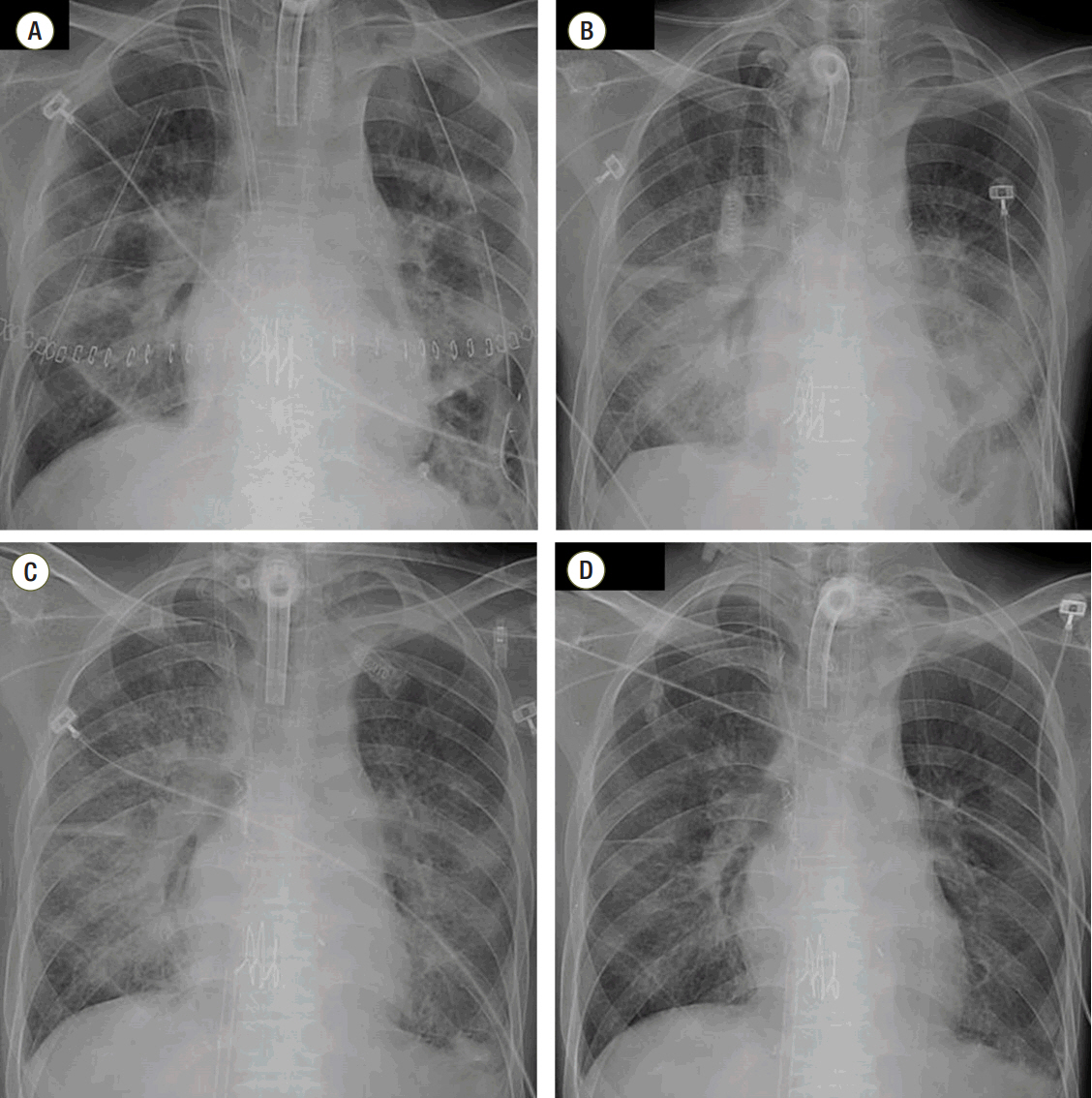
Figure
Reference
-
References
1. Holm AM, Riise GC, Brinch L, Bjørtuft O, Iversen M, Simonsen S, et al. Lung transplantation for bronchiolitis obliterans after allogeneic hematopoietic stem cell transplantation: unresolved questions. Transplantation. 2013; 96:e21–2.2. Kim YR, Haam SJ, Park YG, Lim BJ, Park YM, Paik HC. Lung transplantation for bronchiolitis obliterans after allogeneic hematopoietic stem cell transplantation. Yonsei Med J. 2012; 53:1054–7.
Article3. Soubani AO, Kingah P, Alshabani K, Muma G, Haq A. Lung transplantation following hematopoietic stem cell transplantation: report of two cases and systematic review of literature. Clin Transplant. 2014; 28:776–82.
Article4. Orens JB, Estenne M, Arcasoy S, Conte JV, Corris P, Egan JJ, et al. International guidelines for the selection of lung transplant candidates: 2006 update--a consensus report from the Pulmonary Scientific Council of the International Society for Heart and Lung Transplantation. J Heart Lung transplant. 2006; 25:745–55.
Article5. Fournier PE, Richet H. The epidemiology and control of Acinetobacter baumannii in health care facilities. Clin Infect Dis. 2006; 42:692–9.
Article6. Nunley DR, Bauldoff GS, Mangino JE, Pope-Harman AL. Mortality associated with Acinetobacter baumannii infections experienced by lung transplant recipients. Lung. 2010; 188:381–5.
Article7. Shields RK, Kwak EJ, Potoski BA, Doi Y, Adams-Haduch JM, Silviera FP, et al. High mortality rates among solid organ transplant recipients infected with extensively drug-resistant Acinetobacter baumannii: using in vitro antibiotic combination testing to identify the combination of a carbapenem and colistin as an effective treatment regimen. Diagn Microbiol Infect Dis. 2011; 70:246–52.
Article8. Shoham S, Shah PD. Impact of multidrug-resistant organisms on patients considered for lung transplantation. Infect Dis Clin North Am. 2013; 27:343–58.
Article9. Bonvillain RW, Valentine VG, Lombard G, LaPlace S, Dhillon G, Wang G. Post-operative infections in cystic fibrosis and non-cystic fibrosis patients after lung transplantation. J Heart Lung transplant. 2007; 26:890–7.
Article10. Palmer SM, Alexander BD, Sanders LL, Edwards LJ, Reller LB, Davis RD, et al. Significance of blood stream infection after lung transplantation: analysis in 176 consecutive patients. Transplantation. 2000; 69:2360–6.11. Vos R, Vanaudenaerde BM, Geudens N, Dupont LJ, Van Raemdonck DE, Verleden GM. Pseudomonal airway colonisation: risk factor for bronchiolitis obliterans syndrome after lung transplantation? Eur Respir J. 2008; 31:1037–45.
Article12. Murray S, Charbeneau J, Marshall BC, LiPuma JJ. Impact of burkholderia infection on lung transplantation in cystic fibrosis. Am J Respir Crit Care Med. 2008; 178:363–71.13. Kennedy MP, Coakley RD, Donaldson SH, Aris RM, Hohneker K, Wedd JP, et al. Burkholderia gladioli: five year experience in a cystic fibrosis and lung transplantation center. J Cyst Fibros. 2007; 6:267–73.
Article14. Sopirala MM, Pope-Harman A, Nunley DR, Moffatt- Bruce S, Ross P, Martin SI. Multidrug-resistant Acinetobacter baumannii pneumonia in lung transplant recipients. J Heart Lung Transplant. 2008; 27:804–7.
Article15. Martins N, Martins IS, de Freitas WV, de Matos JA, Magalhães AC, Girão VB, et al. Severe infection in a lung transplant recipient caused by donor-transmitted carbapenem-resistant Acinetobacter baumannii. Transpl Infect Dis. 2012; 14:316–20.
Article16. Michalopoulos A, Falagas ME. Treatment of Acinetobacter infections. Expert Opin Pharmacother. 2010; 11:779–88.17. Petrosillo N, Ioannidou E, Falagas ME. Colistin monotherapy vs. combination therapy: evidence from microbiological, animal and clinical studies. Clin Microbiol Infect. 2008; 14:816–27.
Article18. Gordon NC, Wareham DW. A review of clinical and microbiological outcomes following treatment of infections involving multidrug-resistant Acinetobacter baumannii with tigecycline. J Antimicrob Chemother. 2009; 63:775–80.
Article19. Gallagher JC, Rouse HM. Tigecycline for the treatment of Acinetobacter infections: a case series. Ann Pharmacother. 2008; 42:1188–94.
Article20. Falagas ME, Kasiakou SK. Toxicity of polymyxins: a systematic review of the evidence from old and recent studies. Crit Care. 2006; 10:R27.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Carbapenem-Resistant Acinetobacter baumannii
- Clinical Features of Acinetobacter Baumannii Keratitis
- Epidemiology and treatment of antimicrobialresistant gram-negative bacteria in Korea
- Clinical and Economic Evaluation of Multidrug-Resistant Acinetobacter baumannii Colonization in the Intensive Care Unit
- Update on the Epidemiology, Treatment, and Outcomes of Carbapenem-resistant Acinetobacter infections