Korean J Androl.
2011 Dec;29(3):223-230. 10.5534/kja.2011.29.3.223.
Efficacy and Safety of Biodegradable Microparticles in the Regeneration of Injured Rabbit Corpus Cavernosum: Primary Report
- Affiliations
-
- 1Department of Urology, Ewha Womans University School of Medicine, Seoul, Korea. woochung@ewha.ac.kr
- 2Department of Urology, Kangseo Songdo Hospital, Seoul, Korea.
- 3REGEN Biotech, Seoul, Korea.
- KMID: 2226456
- DOI: http://doi.org/10.5534/kja.2011.29.3.223
Abstract
- PURPOSE
This study analyzed the effectiveness of poly (lactic-co-glycolic acid) (PLGA) as a tissue recovery agent and determines the in vivo safety and efficacy of microparticle-based PLGA.
MATERIALS AND METHODS
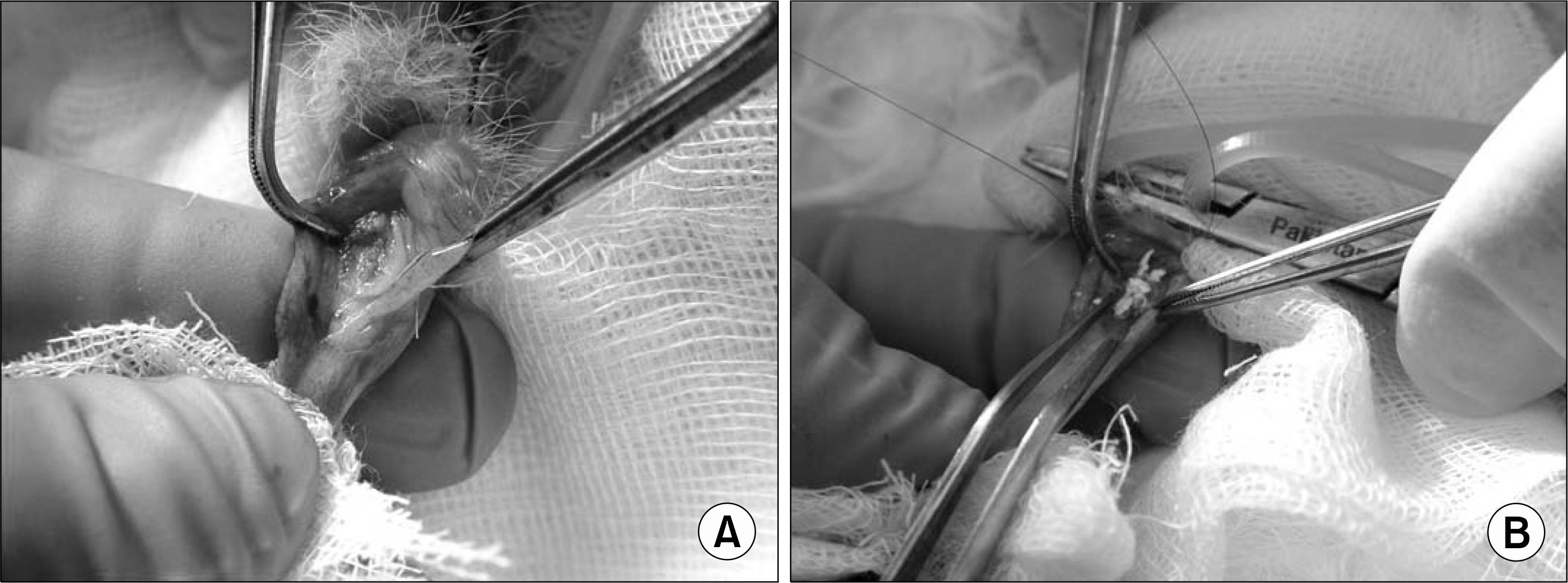
Fifteen 3-month-old male white rabbits were used. Allogenic adipose tissue derived stromal vascular fraction (SVF) was cultured and labeled with the fluorescent dye PKH26. The rabbits were divided into 4 groups: the SVF group, the PLGA group, the normal control group, and the disease control group. The right corpus cavernosal tissue of the rabbits was surgically removed in the selected portion, except in the normal control group. The defect space of each rabbit was replaced with 10(6) SVF cells in the SVF group and 0.1 g of biodegradable polymer solution in the PLGA group. Microscopic confirmation and analysis of tissue regeneration were performed after 8 weeks. Using confocal microscopy, the nuclei of the smooth muscle cells and SVF migration were examined. The composition of smooth muscle and fibrosis of the injured corpus cavernosum were compared and analyzed by Masson's trichrome stain.
RESULTS
There were no signs of migration or rejection of the injected materials in any of the experimental groups. The mean amount of smooth muscle in the normal control group was 15.25+/-1.34 microm2 (right) and 13.90+/-0.703 microm2 (left); in the disease control group it was 11.10+/-0.87 microm2 (right) and 12.80+/-1.01 microm2 (left); in the SVF group it was 13.82+/-4.10 microm2 (right) and 13.96+/-3.94 microm2 (left); and in the PLGA group it was 12.89+/-1.39 microm2 (right) and 13.24+/-1.43 microm2 (left). Only the disease control group showed significant decreased smooth muscle in the left cavernosum (p<0.05). No significant difference was found between the left and right side of each rabbit's cavernosal smooth muscle in the SVF or PLGA group (p>0.05). Furthermore, no difference was found between any two groups (normal control versus SVF (p=0.705), normal control versus PLGA (p=0.88), SVF versus PLGA (p=0.23).
CONCLUSIONS
PLGA microparticles had the same tissue restoring effect when compared with SVF and no adverse effect or migration of particles was found through the injection of PLGA or SVF. PLGA is safe and has the proper tissue recovery effect, saving additional tissue harvesting.
Keyword
MeSH Terms
Figure
Reference
-
1). Woodward SC, Brewer PS, Moatamed F, Schindler A, Pitt CG. The intracellular degradation of poly (epsilon-caprolactone). J Biomed Mater Res. 1985; 19:437–44.2). Pitt CG, Gratzl MM, Kimmel GL, Surles J, Schindler A. Aliphatic polyesters II. The degradation of poly (DL-lactide), poly (epsilon-caprolactone), and their copolymers in vivo. Biomaterials. 1981; 2:215–20.3). Kershen RT, Yoo JJ, Moreland RB, Krane RJ, Atala A. Reconstitution of human corpus cavernosum smooth muscle in vitro and in vivo. Tissue Eng. 2002; 8:515–24.4). Perovic SV, Byun JS, Scheplev P, Djordjevic ML, Kim JH, Bubanj T. New perspectives of penile enhancement surgery: tissue engineering with biodegradable scaffolds. Eur Urol. 2006; 49:139–47.
Article5). Lee KE, Kim BK, Yuk SH. Biodegradable polymeric nanospheres formed by temperature-induced phase transition in a mixture of poly(lactide-co-glycolide) and poly(ethylene oxide)-poly(propylene oxide)-poly(ethylene oxide) triblock copolymer. Bio-macromolecules. 2002; 3:1115–9.
Article6). Oh SH, Lee JY, Ghil SH, Lee SS, Yuk SH, Lee JH. PCL microparticle-dispersed PLGA solution as a potential injectable urethral bulking agent. Biomaterials. 2006; 27:1936–44.
Article7). Kershen RT, Yoo JJ, Moreland RB, Krane RJ, Atala A. Reconstitution of human corpus cavernosum smooth muscle in vitro and in vivo. Tissue Eng. 2002; 8:515–24.8). Kuzyk PR, Schemitsch EH, Davies JE. A biodegradable scaffold for the treatment of a diaphyseal bone defect of the tibia. J Orthop Res. 2010; 28:474–80.
Article9). Lin WJ, Flanagan DR, Linhardt RJ. A novel fabrication of poly(epsilon-caprolactone) microspheres from blends of poly(epsilon-caprolactone) and poly (ethyleneglycol)s. Polymer. 1999; 40:1731–5.10). Gilding DK. Biodegradable polymers. Willams DF, editor. editor.Biocompatibility of clinical implant materials. Boca Raton, Fla: CRC Press;1981. p. 209–32.11). Freed LE, Vunjak-Novakovic G, Biron RJ, Eagles DB, Lesnoy DC, Barlow SK, et al. Biodegradable polymer scaffolds for tissue engineering. Biotechnology (NY). 1994; 12:689–93.
Article12). Tanaka T, Hirose M, Kotobuki N, Tadokoro M, Ohgushi H, Fukuchi T, et al. Bone augmentation by bone marrow mesenchymal stem cells cultured in three-dimensional biodegradable polymer scaffolds. J Biomed Mater Res A. 2009; 91:428–35.
Article13). Lee SW, Kim BS, Park HJ. Preliminary evaluation for New Injectable Material: PLGA Microsphere. Korean J Urol. 2003; 44:1167–71.14). Chung HJ, Park TG. Injectable cellular aggregates prepared from biodegradable porous microspheres for adipose tissue engineering. Tissue Eng Part A. 2009; 15:1391–400.
Article15). Krebs MD, Sutter KA, Lin AS, Guldberg RE, Alsberg E. Injectable poly(lactic-co-glycolic) acid scaffolds with in situ pore formation for tissue engineering. Acta Biomater. 2009; 5:2847–59.
Article16). Casteilla L, Planat-Bénard V, Cousin B, Laharrague P, Bourin P. Vascular and endothelial regeneration. Curr Stem Cell Res Ther. 2010; 5:141–4.
Article17). Bacou F, el Andalousi RB, Daussin PA, Micallef JP, Levin JM, Chammas M, et al. Transplantation of adipose tissue-derived stromal cells increases mass and functional capacity of damaged skeletal muscle. Cell Transplant. 2004; 13:103–11.
Article18). Fraser JK, Wulur I, Alfonso Z, Hedrick MH. Fat tissue: an underappreciated source of stem cells for biotechnology. Trends Biotechnol. 2006; 24:150–4.
Article19). Planat-Benard V, Silvestre JS, Cousin B, André M, Nibbelink M, Tamarat R, et al. Plasticity of human adipose lineage cells toward endothelial cells: physiological and therapeutic perspectives. Circulation. 2004; 109:656–63.20). Chen KL, Eberli D, Yoo JJ, Atala A. Bioengineered corporal tissue for structural and functional restoration of the penis. Proc Natl Acad Sci USA. 2010; 107:3346–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect and Mechanism of the Specific Phosphodiesterase (PDE) III-Inhibitor Milrinone on Human and Rabbit Corpus Cavernosum
- Pharmacologic Effect of Phentolamine on Norepinephrine Induced Contraction of Corpus Cavernosum
- The Effects of Endothelium Dependent Vasodilator Substances on Rabbit Corpora Cavernosa
- Effects of Ginseng Alkaloid on the Tension of Rabbit Corpus Cavernosum
- Local Effect of Psychotherapeutic Agents on Rabbit Penile Corpus Cavernosum