J Korean Ophthalmol Soc.
2014 Sep;55(9):1384-1387. 10.3341/jkos.2014.55.9.1384.
A Case of Fungal Keratitis Caused by Paecilomyces lilacinus after Penetrating Keratoplasty
- Affiliations
-
- 1Catholic Institute for Visual Science, Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. ckjoo@catholic.ac.kr
- 2Department of Ophthalmology, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2217126
- DOI: http://doi.org/10.3341/jkos.2014.55.9.1384
Abstract
- PURPOSE
To report a case of corneal ulcer caused by Paecilomyces lilacinus after penetrating keratoplasty.
CASE SUMMARY
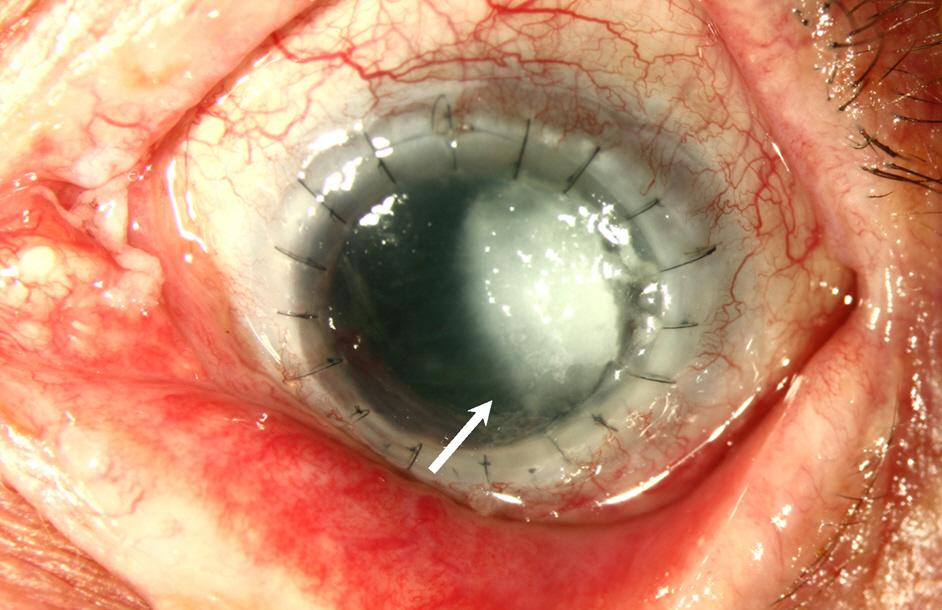
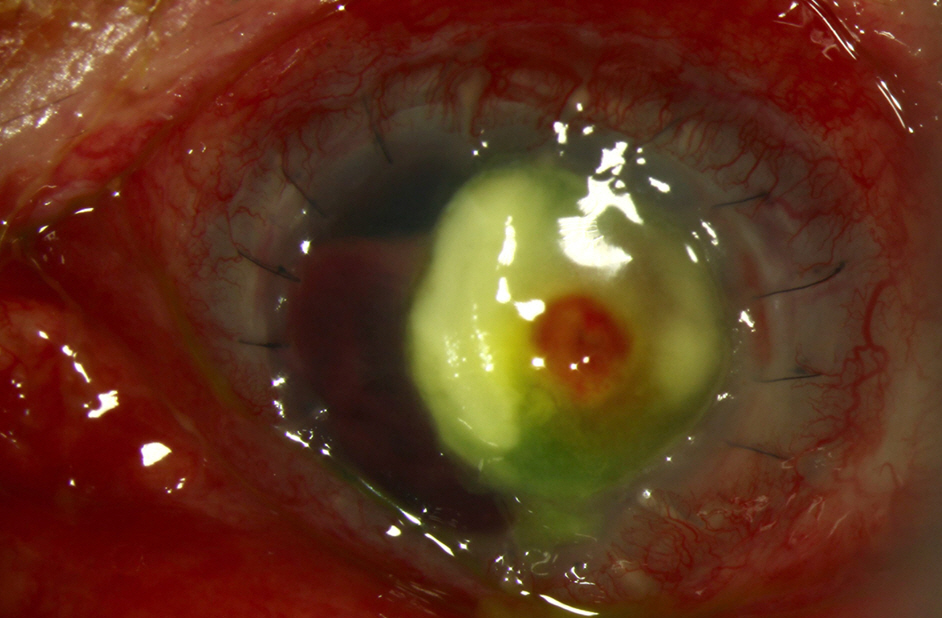
A 67-year-old male with a history of penetrating keratoplasty in the left eye 7 years prior and re-penetrating keratoplasty in the left eye due to graft failure in June 2013, visited our clinic for ocular pain and conjunctival injection in the left eye 3 days in duration. Corneal scrapings were performed for Gram and fungal stains and cultures. The patient was admitted to the hospital for hourly topical fortified ceftazidime and amphotericin B. Despite intensive topical therapy, no improvement was observed. Three days later, fungal culture confirmed Paecilomyces lilacinus and topical voriconazole was prepared from the intravenous formulation and was administered topically and intravenously. Despite medical therapy with voriconazole, perforation occurred requiring a tectonic keratoplasty.
CONCLUSIONS
Keratitis caused by Paecilomyces lilacinus is difficult to eradicate and refractory to amphotericin B. We suggest early use of topical eyedrops, intracameral, and intravitreal injections of voriconazole may be an appropriate treatment for patients with Paecilomyces lilacinus keratitis.
MeSH Terms
Figure
Reference
-
References
1. Lee DC, Lee JW, Chang SD. A case of fusarium keratitis treated with moxifloxacin 0.5% ophthalmic solution. J Korean Ophthalmol Soc. 2012; 53:338–41.
Article2. Kozarsky AM, Stulting RD, Waring GO 3rd, et al. Penetrating keratoplasty for exogenous Paecilomyces keratitis followed by postoperative endophthalmitis. Am J Ophthalmol. 1984; 98:552–7.
Article3. Hariprasad SM, Mieler WF, Lin TK, et al. Voriconazole in the treatment of fungal eye infections: a review of current literature. Br J Ophthalmol. 2008; 92:871–8.
Article4. Srinivasan M. Fungal keratitis. Curr Opin Ophthalmol. 2004; 15:321–7.
Article5. Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001; 79:214–21.6. Oh DH, Kim JC, Chun YS. A case of fusarium deep keratitis following scleral graft. J Korean Ophthalmol Soc. 2010; 51:606–10.
Article7. O'Day DM, Head WS, Robinson RD, Clanton JA. Corneal penetration of topical amphotericin B and natamycin. Curr Eye Res. 1986; 5:877–82.8. Hariprasad SM, Mieler WF, Lin TK, et al. Voriconazole in the treatment of fungal eye infections: a review of current literature. Br J Ophthalmol. 2008; 92:871–8.
Article9. Aydin S, Ertugrul B, Gultekin B, et al. Treatment of two postoperative endophthalmitis cases due to Aspergillus flavus and Scopulariopsis spp. with local and systemic antifungal therapy. BMC Infect Dis. 2007; 7:87.
Article10. Sabo JA, Abdel-Rahman SM. Voriconazole: a new triazole antifungal. Ann Pharmacother. 2000; 34:1032–43.
Article11. Jurkunas UV, Langston DP, Colby K. Use of voriconazole in the treatment of fungal keratitis. Int Ophthalmol Clin. 2007; 47:47–59.
Article12. Johnson LB, Kauffman CA. Voriconazole: a new triazole anti-fungal agent. Clin Infect Dis. 2003; 36:630–7.
Article13. Deng SX, Kamal KM, Hollander DA. The use of voriconazole in the management of post-penetrating keratoplasty Paecilomyces keratitis. J Ocul Pharmacol Ther. 2009; 25:175–7.
Article14. Pastor FJ, Guarro J. Clinical manifestations, treatment and outcome of Paecilomyces lilacinus infections. Clin Microbiol Infect. 2006; 12:948–60.
Article15. Byun DS, Yang HN, Cho HG, Cha YJ. A case of corneal ulcer caused by Paecilomyces in diabetic patient wearing soft contact lens. J Korean Ophthalmol Soc. 1987; 28:667–71.16. Bunya VY, Hammersmith KM, Rapuano CJ, et al. Topical and oral voriconazole in the treatment of fungal keratitis. Am J Ophthalmol. 2007; 143:151–3.
Article17. Ozbek Z, Kang S, Sivalingam J, et al. Voriconazole in the management of Alternaria keratitis. Cornea. 2006; 25:242–4.
Article18. Sponsel W, Chen N, Dang D, et al. Topical voriconazole as a novel treatment for fungal keratitis. Antimicrob Agents Chemother. 2006; 50:262–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Keratitis Caused by Paecilomyces lilacinus after Cataract Surgery in a Patient with Systemic and Autoimmune Disease
- A Case of Fusarium solani Keratitis mixed by Acremonium falciforme
- A Localized Cutaneous Paecilomyces lilacinus Infection Treated with Voriconazole
- Paecilomyces Keratitis: Cases in Korea and Literature Review
- Cataract Extraction after Penetrating Keratoplasty