J Korean Ophthalmol Soc.
2014 Nov;55(11):1698-1705. 10.3341/jkos.2014.55.11.1698.
Effect of Preservative-Free Healon Eye Drop on Human Corneal Epithelial Cell in Vitro
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University Hospital, Busan, Korea. jongsool@pusan.ac.kr
- 2Department of Ophthalmology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 3Department of Ophthalmology, Pusan National University School of Medicine, Busan, Korea.
- KMID: 2216621
- DOI: http://doi.org/10.3341/jkos.2014.55.11.1698
Abstract
- PURPOSE
To investigate the biologic effects of preservative-free artificial tear drops on cultured human corneal epithelial cells in vitro.
METHODS
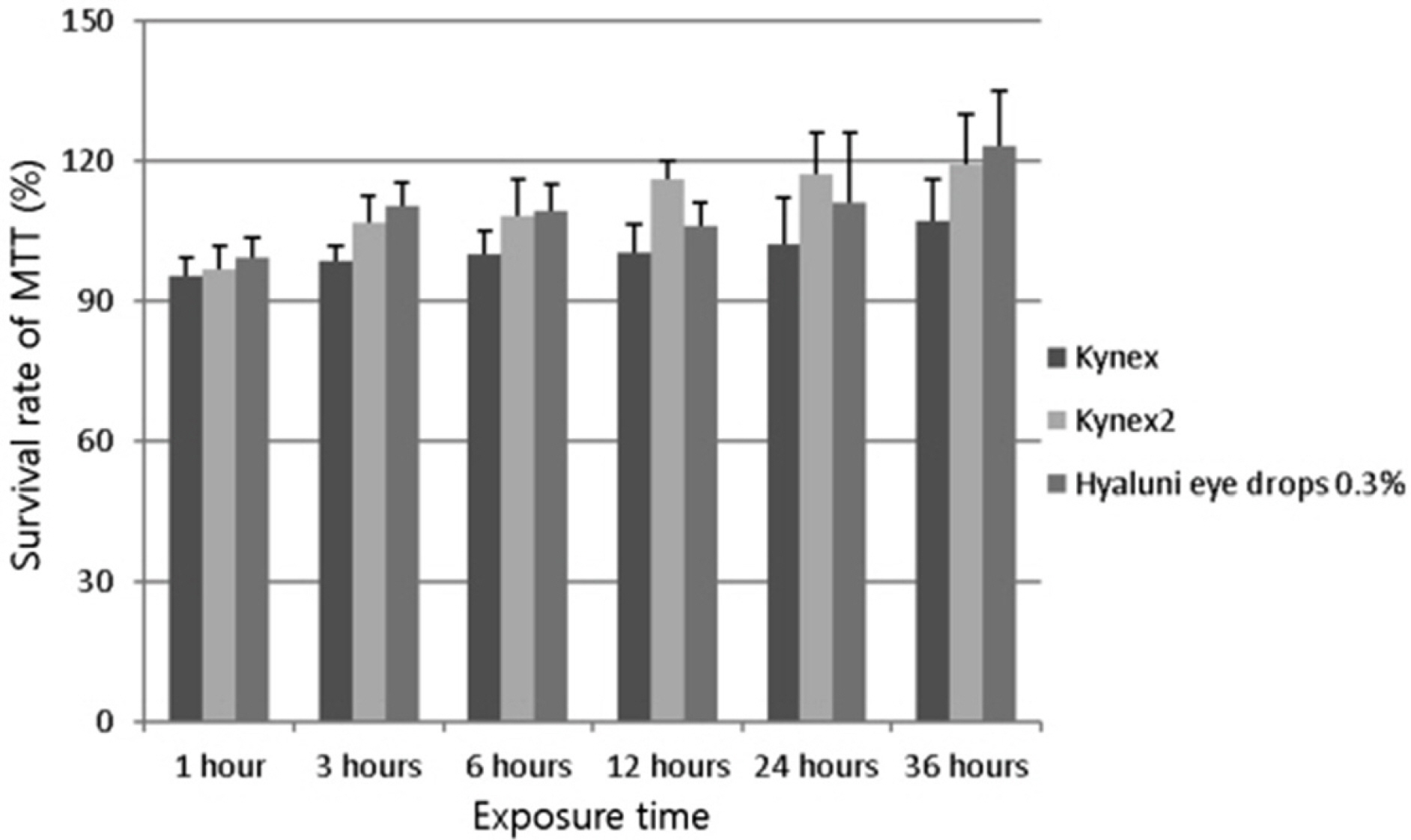
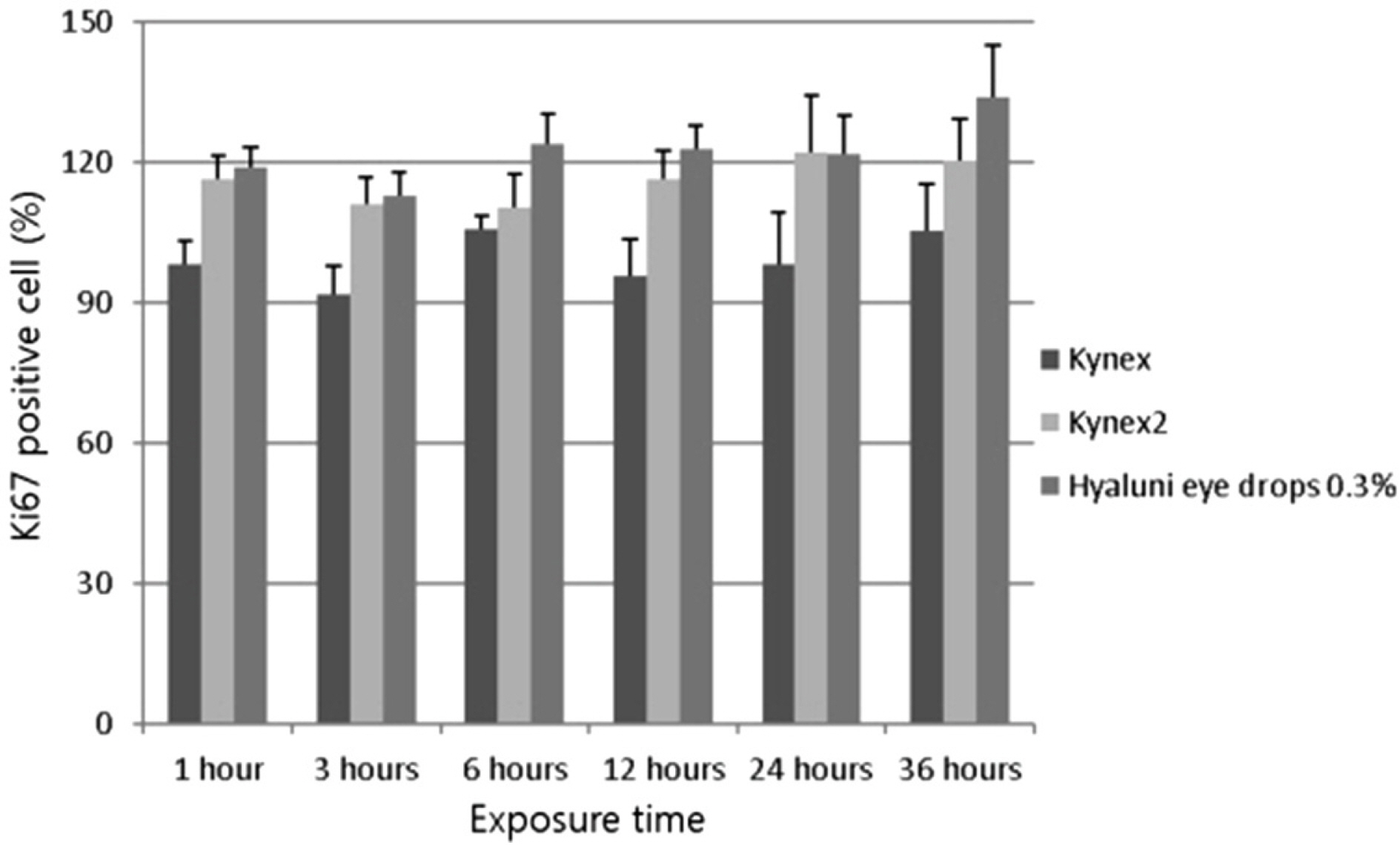
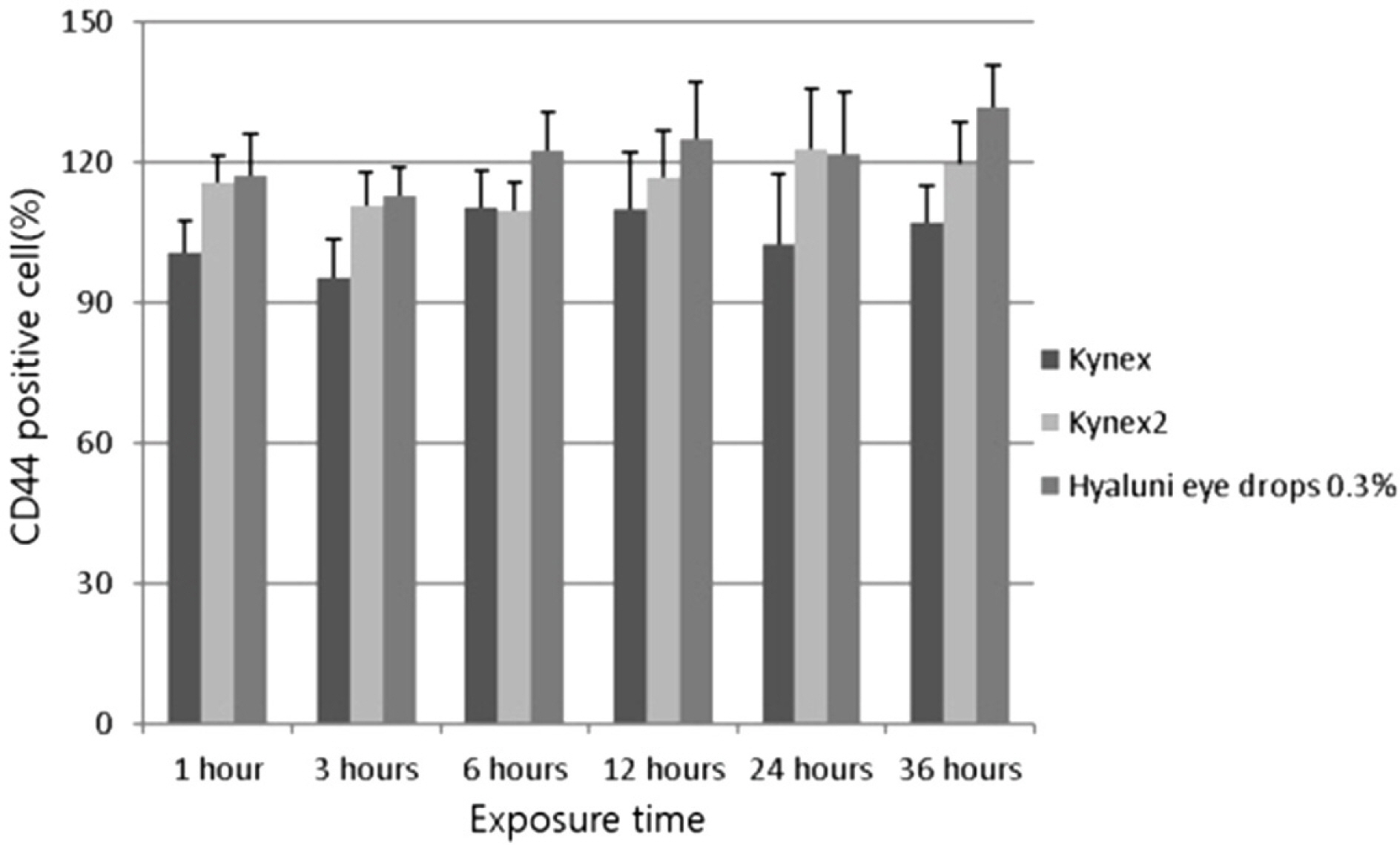
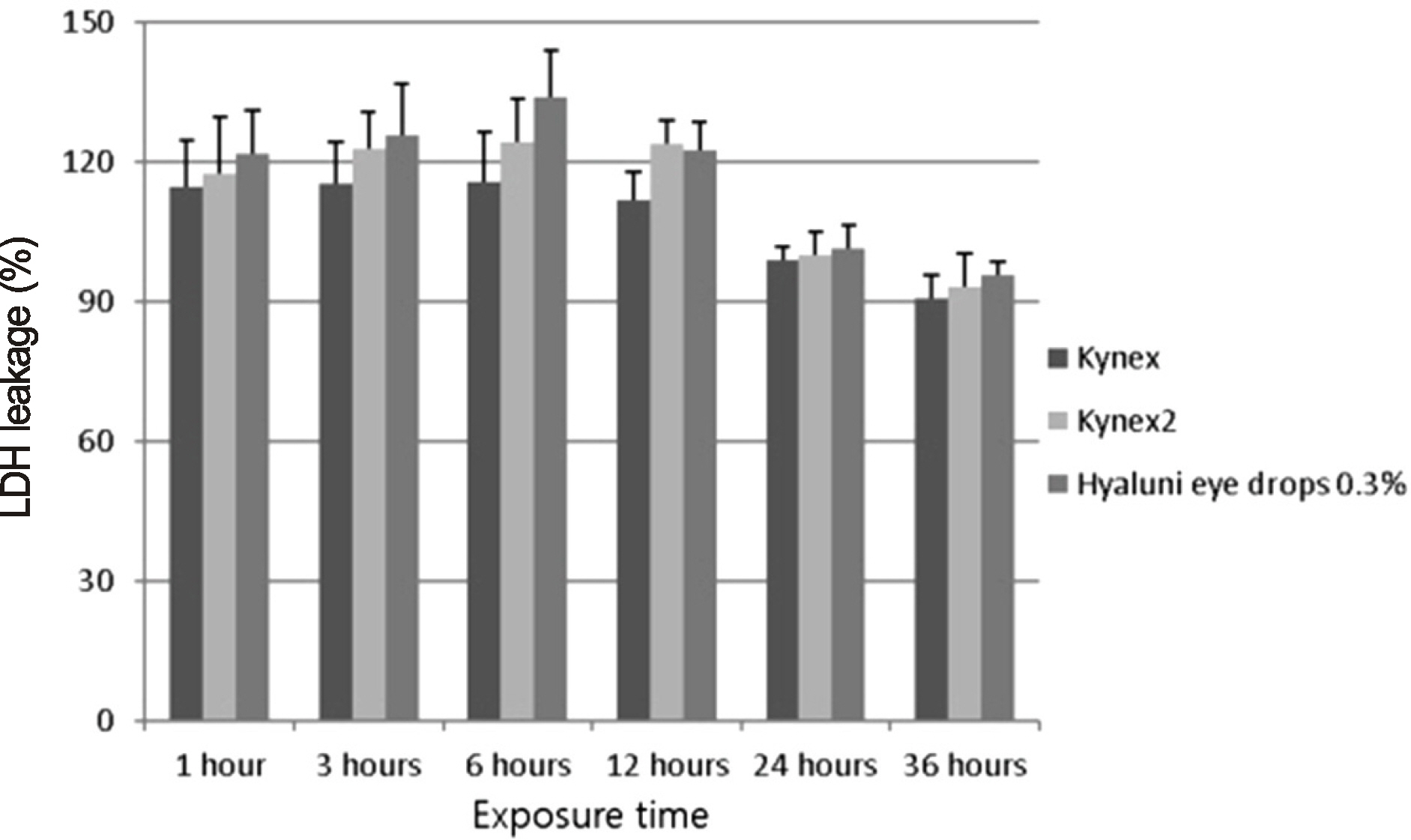
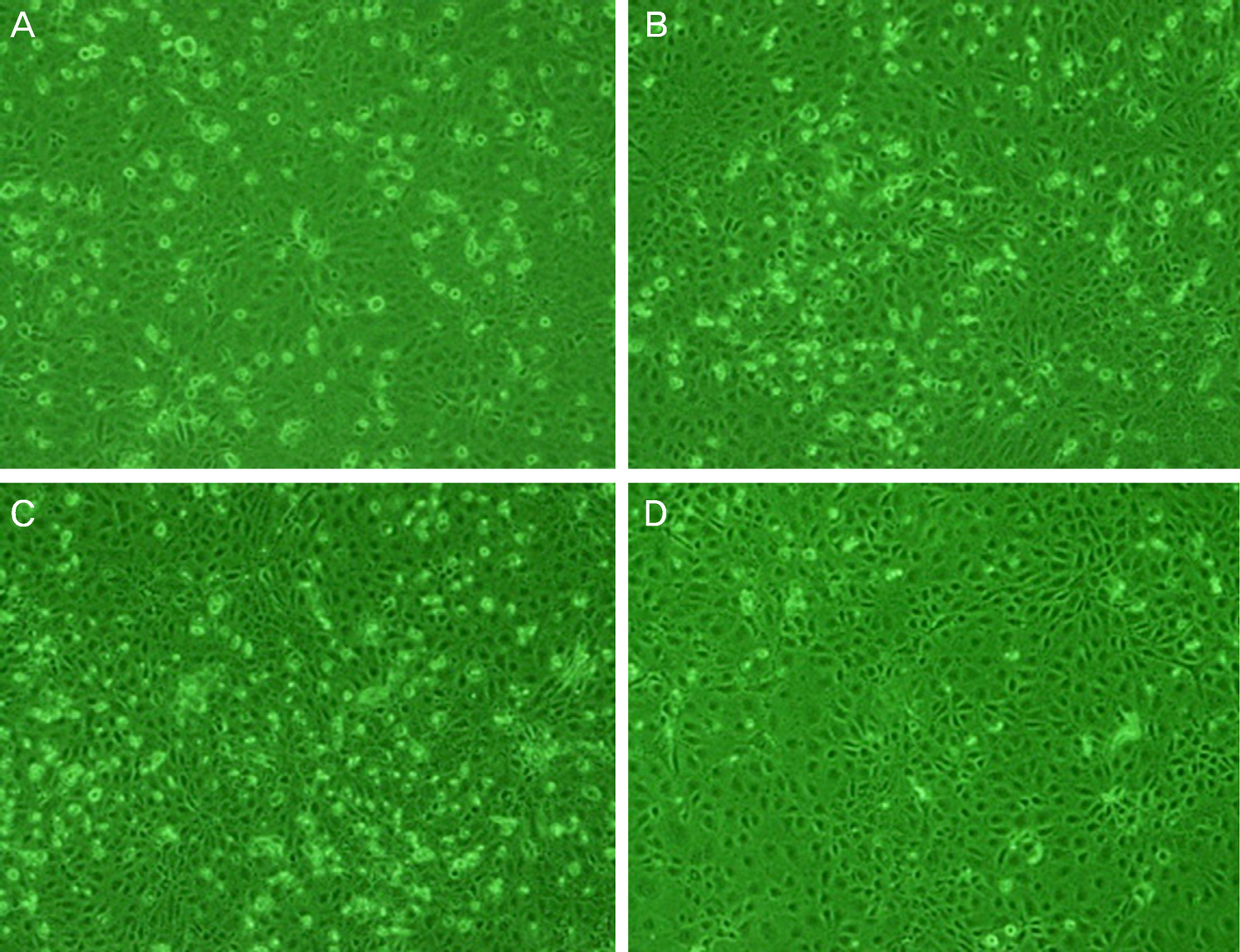
The effects of preservative-free artificial tear drops (sodium hyaluronate 0.1% (Kynex(R), Alcon, Seoul, Korea), sodium hyaluronate 0.18% (Kynex2(R), Alcon, Seoul, Korea), and sodium hyaluronate 0.3% (Hyaluni eye drops 0.3%(R), Taejoon, Seoul, Korea)) on human corneal epithelial cells were evaluated. Cellular proliferation was determined using MTT (3- (4,5-dimethylthiazol-2yl)-2,5-diphenyl-2H-tetrazolium bromide) and Ki-67 assays. Cellular migration was determined using CD44 and scratch wound assays. Cell damage was determined using the lactate dehydrogenase (LDH) assay and cellular morphologies using electronic microscopy and inverted microscopy.
RESULTS
Proliferation of corneal epithelial cells, as determined by the MTT and Ki-67 assays, was not significantly different between the different eye drops (p > 0.05). The measured value of cellular migration after exposure of the sodium hyaluronate 0.3%, as determined by mean CD44 percentage and scratch wound assay, was higher than that of the sodium hyaluronate 0.1% and sodium hyaluronate 0.18%, but the CD44 value was not significantly different (p > 0.05). The LDH titer tended to increase as the concentration of sodium hyaluronate increased (p > 0.05), but influence on cytoplasm, as determined by electronic microscopy, was not different.
CONCLUSIONS
Among 3 preservative-free artificial tear drops, sodium hyaluronate 0.3% demonstrated increased migration of corneal epithelial cells. As the concentration of sodium hyaluronate in eye drops increased, the corneal cytotoxicity of corneal epithelial cells also increased. However, there was no significant difference among the 3 tear drops.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Long-Term Effect of Preservative-Free Sodium Hyaluronate Eye Drop on Human Corneal Epithelial Cell
Jong Soo Lee, Jae Sung Park, Ho Yun Kim
J Korean Ophthalmol Soc. 2015;56(12):1945-1952. doi: 10.3341/jkos.2015.56.12.1945.
Reference
-
References
1. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.2. Sand BB, Marner K, Norn MS. Sodium hyaluronate in the treatment of keratoconjunctivitis sicca. A double masked clinical trial. Acta Ophthalmol (Copenh). 1989; 67:181–3.3. Nishida T, Nakamura M, Mishima H, Otori T. Hyaluronan stimulates corneal epithelial migration. Exp Eye Res. 1991; 53:753–8.
Article4. Camillieri G, Bucolo C, Rossi S, Drago F. Hyaluronan-induced stimulation of corneal wound healing is a pure pharmacological effect. J Ocul Pharmacol Ther. 2004; 20:548–53.
Article5. Inoue M, Katakami C. The effect of hyaluronic acid on corneal epithelial cell proliferation. Invest Ophthalmol Vis Sci. 1993; 34:2313–5.6. Johnson ME, Murphy PJ, Boulton M. Effectiveness of sodium hyaluronate eyedrops in the treatment of dry eye. Graefes Arch Clin Exp Ophthalmol. 2006; 244:109–12.
Article7. Nakamura M, Hikida M, Nakano T, et al. Characterization of water retentive properties of hyaluronan. Cornea. 1993; 12:433–6.
Article8. Snibson GR, Greaves JL, Soper ND, et al. Precorneal residence times of sodium hyaluronate solutions studied by quantitative gamma scintigraphy. Eye (Lond). 1990; 4(Pt 4):594–602.
Article9. Avisar R, Creter D, Levinsky H, Savir H. Comparative study of tear substitutes and their immediate effect on the precorneal tear film. Isr J Med Sci. 1997; 33:194–7.10. Gomes JA, Amankwah R, Powell-Richards A, Dua HS. Sodium hyaluronate (hyaluronic acid) promotes migration of human corneal epithelial cells in vitro. Br J Ophthalmol. 2004; 88:821–5.
Article11. Joseph A, Powell-Richards AO, Shanmuganathan VA, Dua HS. Epithelial cell characteristics of cultured human limbal explants. Br J Ophthalmol. 2004; 88:393–8.
Article12. Sugiyama T, Miyauchi S, Machida A, et al. The effect of sodium hyaluronate on the migration of rabbit corneal epithelium. II. The effect of topical administration. J Ocul Pharmacol. 1991; 7:53–64.
Article13. Algawi K, Agrell B, Goggin M, O'Keefe M. Randomized clinical trial of topical sodium hyaluronate after excimer laser photorefractive keratectomy. J Refract Surg. 1995; 11:42–4.
Article14. Miyauchi S, Sugiyama T, Machida A, et al. The effect of sodium hyaluronate on the migration of rabbit corneal epithelium. I. An in vitro study. J Ocul Pharmacol. 1990; 6:91–9.
Article15. Asari A, Morita M, Sekiguchi T, et al. Hyaluronan, CD44 and fibronectin in rabbit corneal epithelial wound healing. Jpn J Ophthalmol. 1996; 40:18–25.16. Brignole F, Pisella PJ, Dupas B, et al. Efficacy and safety of 0.18% sodium hyaluronate in patients with moderate dry eye syndrome and superficial keratitis. Graefes Arch Clin Exp Ophthalmol. 2005; 243:531–8.
Article17. Zhu SN, Nölle B, Duncker G. Expression of adhesion molecule CD44 on human corneas. Br J Ophthalmol. 1997; 81:80–4.
Article18. Adler R. Mechanisms of photoreceptor death in retinal degenerations. From the cell biology of the 1990s to the ophthalmology of the 21st century? Arch Ophthalmol. 1996; 114:79–83.
Article19. Thompson CB. Apoptosis in the pathogenesis and treatment of disease. Science. 1995; 267:1456–62.
Article20. Wee WR, Wang XW, McDonnell PJ. Effect of artificial tears on cultured keratocytes in vitro. Cornea. 1995; 14:273–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Preservative-free Artificial Eye Drop on Human Corneal Epithelial Cell in vitro
- Long-Term Effect of Preservative-Free Sodium Hyaluronate Eye Drop on Human Corneal Epithelial Cell
- The changes of Corneal Endothelial Morphology after Phacoemulsification by using Healon GV of Viscoat
- Effect of Artificial Tears Used in Contact Lens-wearing Eyes on Human Corneal Epithelial Cells in Vitro
- Effects of Corneal Toxicity and Conjunctival Injection of Preservative-free 0.1% Fluorometholone after Pediatric Strabismus Surgery