J Korean Ophthalmol Soc.
2015 Dec;56(12):1945-1952. 10.3341/jkos.2015.56.12.1945.
Long-Term Effect of Preservative-Free Sodium Hyaluronate Eye Drop on Human Corneal Epithelial Cell
- Affiliations
-
- 1Department of Ophthalmology, Pusan National University Hospital, Busan, Korea. jongsool@pusan.ac.kr
- 2Department of Ophthalmology, Pusan National University School of Medicine, Busan, Korea.
- 3Lee Eye Clinic, Busan, Korea.
- KMID: 2148759
- DOI: http://doi.org/10.3341/jkos.2015.56.12.1945
Abstract
- PURPOSE
To investigate the biological effects of preservative-free artificial tear drops on cultured human corneal epithelial cells in vitro.
METHODS
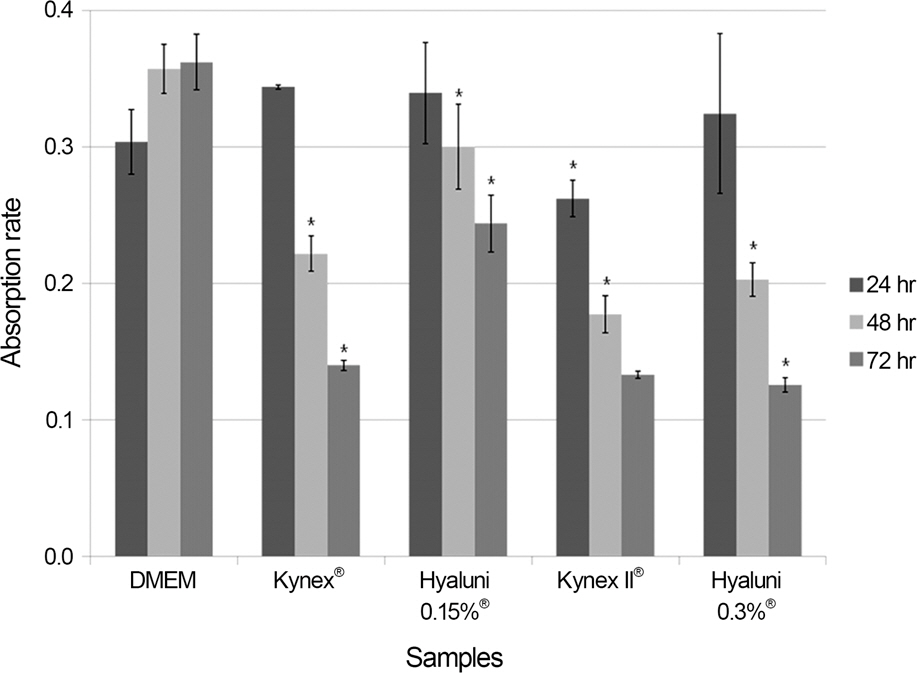
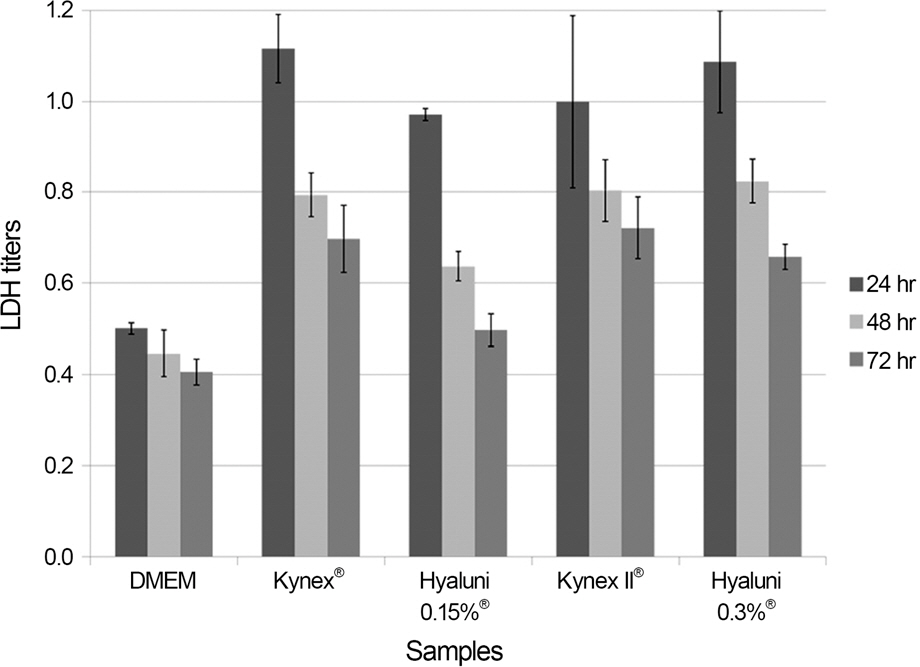
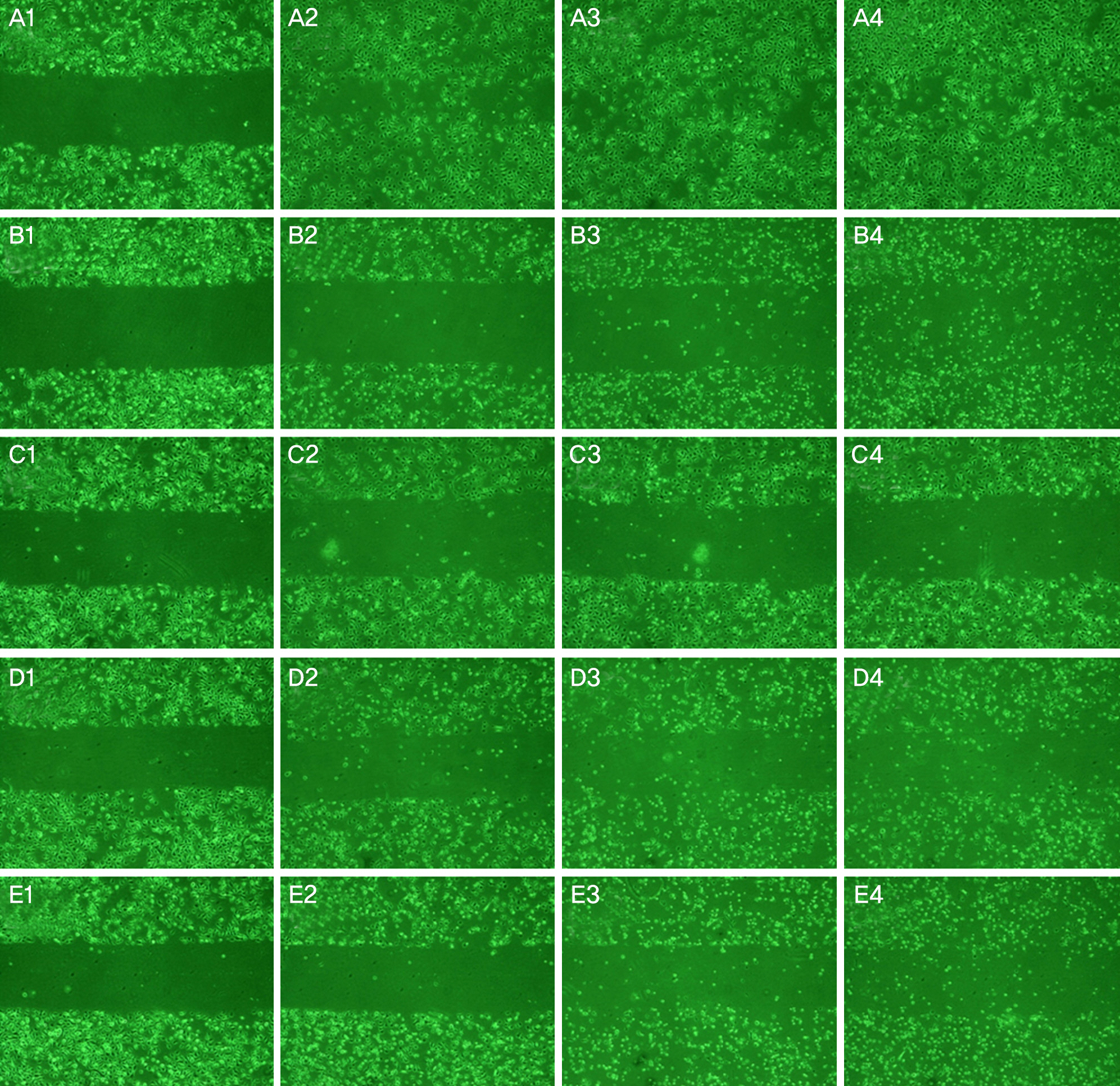
The effects of the preservative-free artificial tear drops (Kynex(R) 0.1%, Kynex II(R) 0.18% [Alcon, Seoul, Korea] and Hyaluni eye drops(R) 0.15%, 0.3% [Taejun, Seoul, Korea]) on the human corneal epithelial cells were evaluated. An methyl thiazolyl tetrazolium (MTT)-based colorimetric assay was performed to assess the cellular metabolic activity and a lactate dehydrogenase (LDH) leakage assay was used to determine cellular toxicity. The eye drop ingredients were analyzed for electrolyte composition, pH, and osmolarity. We performed a scratch assay and cellular morphology test using electronic microscopy.
RESULTS
The metabolic activity of corneal epithelial cells was higher than controls at 24 hours after exposure and then decreased at 48 and 72 hours after exposure (p < 0.05). The LDH titers of the 4 eye drops were higher compared with controls (p < 0.05). Sodium hyaluronate 0.18% contained lower concentrations of Na+ or Cl- and showed lower osmolarity values compared with the other eye drops. The cellular migration based on the scratch assay was more delayed and cellular damage such as loss of microvilli, rough endothelial reticulum (RER), and mitochondria dilatation was greater than controls based on electron microscopy.
CONCLUSIONS
Long-term exposure to preservative-free sodium hyaluronate eye drops may induce decreased metabolic activity and cellular damage. Thus, preservative-free artificial tears should be used carefully to prevent cellular toxicity.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Sand BB, Marner K, Norn MS. Sodium hyaluronate in the treat-ment of keratoconjunctivitis sicca. A double masked clinical trial. Acta Ophthalmol (Copenh). 1989; 67:181–3.2. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye Workshop (2007) Ocul Surf. 2007; 5:75–92.3. Ayaki M, Yaguchi S, Iwasawa A, Koide R. Cytotoxicity of oph-thalmic solutions with and without preservatives to human corneal endothelial cells, epithelial cells and conjunctival epithelial cells. Clin Experiment Ophthalmol. 2008; 36:553–9.
Article4. Lee JK, Ryu YH. The effect of antiglaucoma medication on cul-tured human conjunctival epithelial cells. J Korean Ophthalmol Soc. 2006; 47:1811–8.5. Roh YR, Lee SM, Han YK. . Changes in clinical manifes-tations of dry eye syndrome after cataract surgery and the affecting factors. J Korean Ophthalmol Soc. 2011; 52:1030–8.
Article6. Lemp MA. Artificial tear solutions. Int Ophthalmol Clin. 1973; 13:221–9.
Article7. Nakamura M, Hikida M, Nakano T. . Characterization of water retentive properties of hyaluronan. Cornea. 1993; 12:433–6.
Article8. Papa V, Aragona P, Russo S. . Comparison of hypotonic and isotonic solutions containing sodium hyaluronate on the sympto-matic treatment of dry eye patients. Ophthalmologica. 2001; 215:124–7.
Article9. Aragona P, Papa V, Micali A. . Long term treatment with so-dium hyaluronate-containing artificial tears reduces ocular surface damage in patients with dry eye. Br J Ophthalmol. 2002; 86:181–4.
Article10. Brignole F, Pisella PJ, Dupas B. . Efficacy and safety of 0.18% sodium hyaluronate in patients with moderate dry eye syndrome and superficial keratitis. Graefes Arch Clin Exp Ophthalmol. 2005; 243:531–8.
Article11. Yokoi N, Yamada J, Nishida K, Kinoshita S. Effect of sodium hya-luronate on diffuse epithelial keratitis after penetrating keratoplasty. Transplant Proc. 1995; 27:1412–3.12. Inoue M, Katakami C. The effect of hyaluronic acid on corneal epi-thelial cell proliferation. Invest Ophthalmol Vis Sci. 1993; 34:2313–5.13. Gomes JA, Amankwah R, Powell-Richards A, Dua HS. Sodium hyaluronate (hyaluronic acid) promotes migration of human cor-neal epithelial cells in vitro. Br J Ophthalmol. 2004; 88:821–5.
Article14. Kim HY, Park YM, Lee JS. Effect of preservative-free healon eye drop on human corneal epithelial cell in vitro. J Korean Ophthalmol Soc. 2014; 55:1698–705.
Article15. Camillieri G, Bucolo C, Rossi S, Drago F. Hyaluronan-induced stimulation of corneal wound healing is a pure pharmacological effect. J Ocul Pharmacol Ther. 2004; 20:548–53.
Article16. Thompson CB. Apoptosis in the pathogenesis and treatment of disease. Science. 1995; 267:1456–62.
Article17. Wee WR, Wang XW, McDonnell PJ. Effect of artificial tears on cultured keratocytes in vitro. Cornea. 1995; 14:273–9.
Article18. Lee JE, Han HJ, Lee JS, Oum BS. Effect of tranilast on the pro-liferation of human corneal keratocytes in vitro. J Korean Ophthalmol Soc. 2005; 46:510–20.19. Wang L, Li T, Lu L. UV-induced corneal epithelial cell death by ac-tivation of potassium channels. Invest Ophthalmol Vis Sci. 2003; 44:5095–101.
Article20. Huang-Lee LL, Wu JH, Nimni ME. Effects of hyaluronan on colla-gen fibrillar matrix contraction by fibroblasts. J Biomed Mater Res. 1994; 28:123–32.
Article21. Mummert ME. Immunologic roles of hyaluronan. Immunol Res. 2005; 31:189–206.
Article22. Sidwell RU, Dhillon AP, Butler PE, Rustin MH. Localized gran-ulomatous reaction to a semi-permanent hyaluronic acid and acryl-ic hydrogel cosmetic filler. Clin Exp Dermatol. 2004; 29:630–2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Preservative-Free Healon Eye Drop on Human Corneal Epithelial Cell in Vitro
- Effect of Preservative-free Artificial Eye Drop on Human Corneal Epithelial Cell in vitro
- Efficacy of 0.15% Sodium Hyaluronate Eye Drops in Patients’ Ocular Surface after Upper Eyelid Surgery
- Effect of combined sodium hyaluronate and carboxymethyl cellulose on ocular surface in rat dry eye model
- Effect of 0.15% Preservative-free Sodium Hyaluronate on Dry Eye Disease after Femtosecond Laser-assisted Cataract Surgery