J Korean Ophthalmol Soc.
2011 Mar;52(3):277-284. 10.3341/jkos.2011.52.3.277.
Intrastromal Corneal Ring Segments (KeraRing(R)) Implantation for the Correction of Keratoconus
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. hereye@inje.ac.kr
- 2Department of Ophthalmology, Masan Samsung Hospital, Sungkyunkwan University School of Medicine, Masan, Korea.
- KMID: 2214291
- DOI: http://doi.org/10.3341/jkos.2011.52.3.277
Abstract
- PURPOSE
To report the outcomes after the implantation of intrastromal corneal ring segments (KeraRing(R)) by manual tunnel creation for the correction of keratoconus.
METHODS
The present retrospective case series was comprised of 12 eyes of 11 consecutive keratoconic patients. Intrastromal corneal ring segments (KeraRing(R)) were implanted for keratoconus correction after manual tunnel creation. Uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), refractive outcome, and complete ophthalmologic examinations were performed before and after surgery at 1 day, 1 week, 3 months, and 6 months. Corneal topography was measured before surgery, 6 months after surgery and during any necessary follow-up visits.
RESULTS
Intrastromal corneal ring segments (KeraRing(R)) implantation significantly increased BCVA from logMAR 0.47 +/- 0.19 to logMAR 0.28 +/- 0.17 (P < 0.05) and decreased the spherical equivalent from -6.03 +/- 3.24 D to -2.24 +/- 1.96 D. The simulated keratometric value in the Orbscan IIz significantly decreased in K maximum from 50.7 +/- 2.93D to 47.65 +/- 3.15 D and in K minimum from 47.65 +/- 3.15 D to 44.92 +/- 2.80 D.
CONCLUSIONS
Intrastromal corneal ring segments implantation (KeraRing(R)) by manual tunnel creation appears to be effective in improving BCVA and reducing corneal astigmatism and keratometric value in keratoconic patients. KeraRing(R) may delay or prevent the need for a corneal graft, and reduce the contact lens intolerance.
MeSH Terms
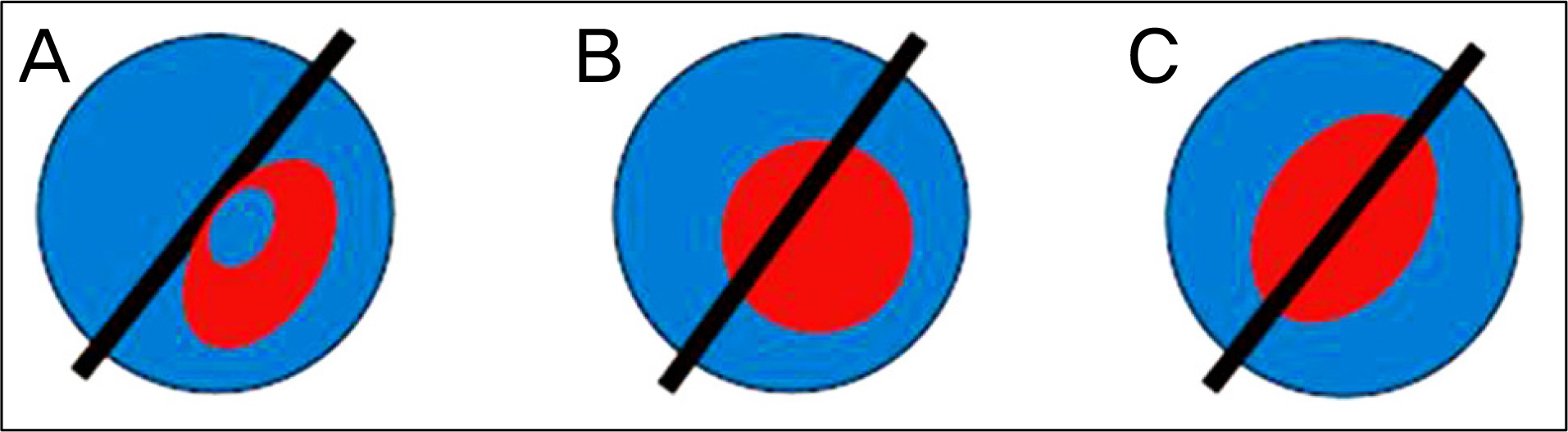
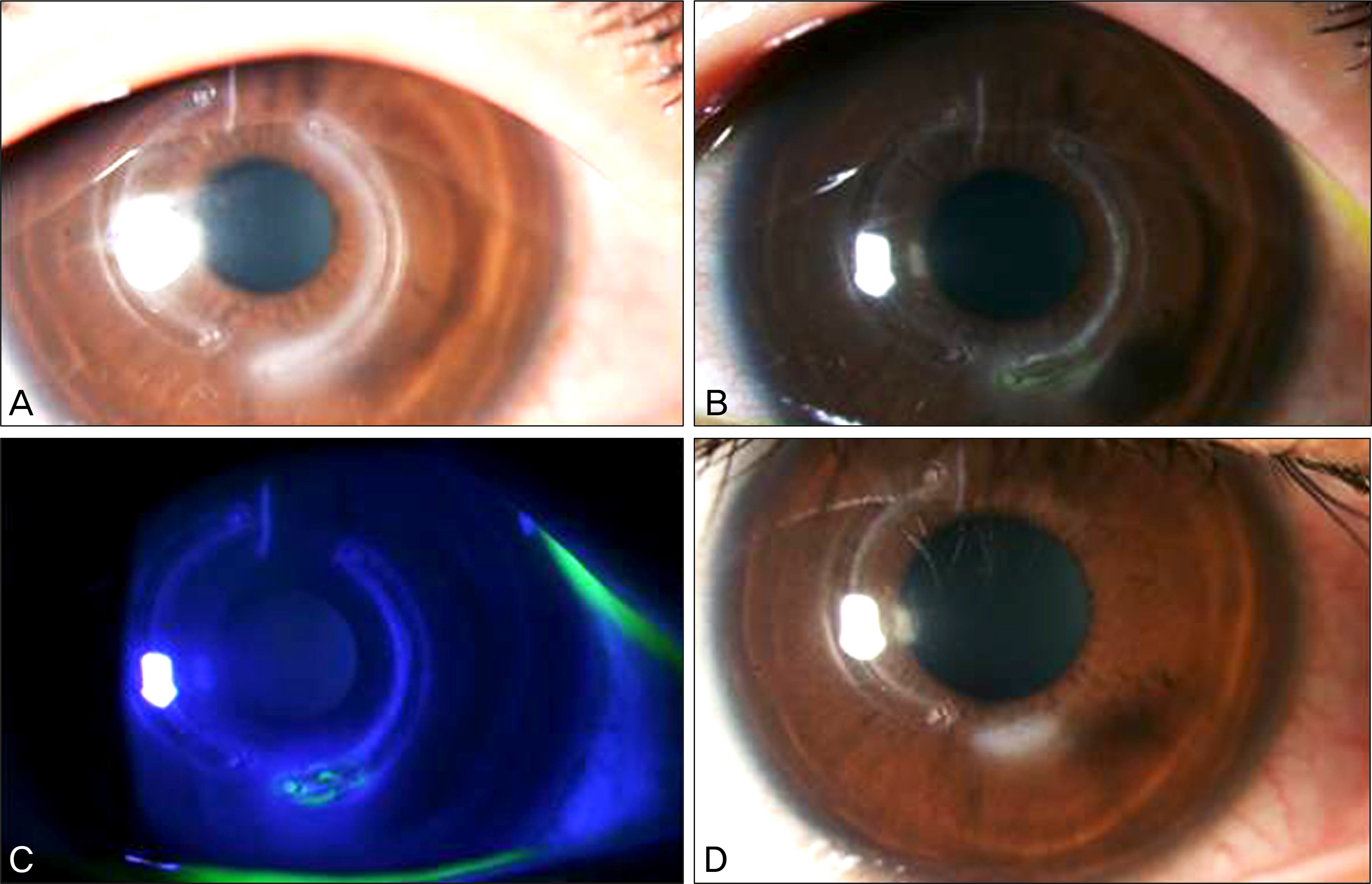
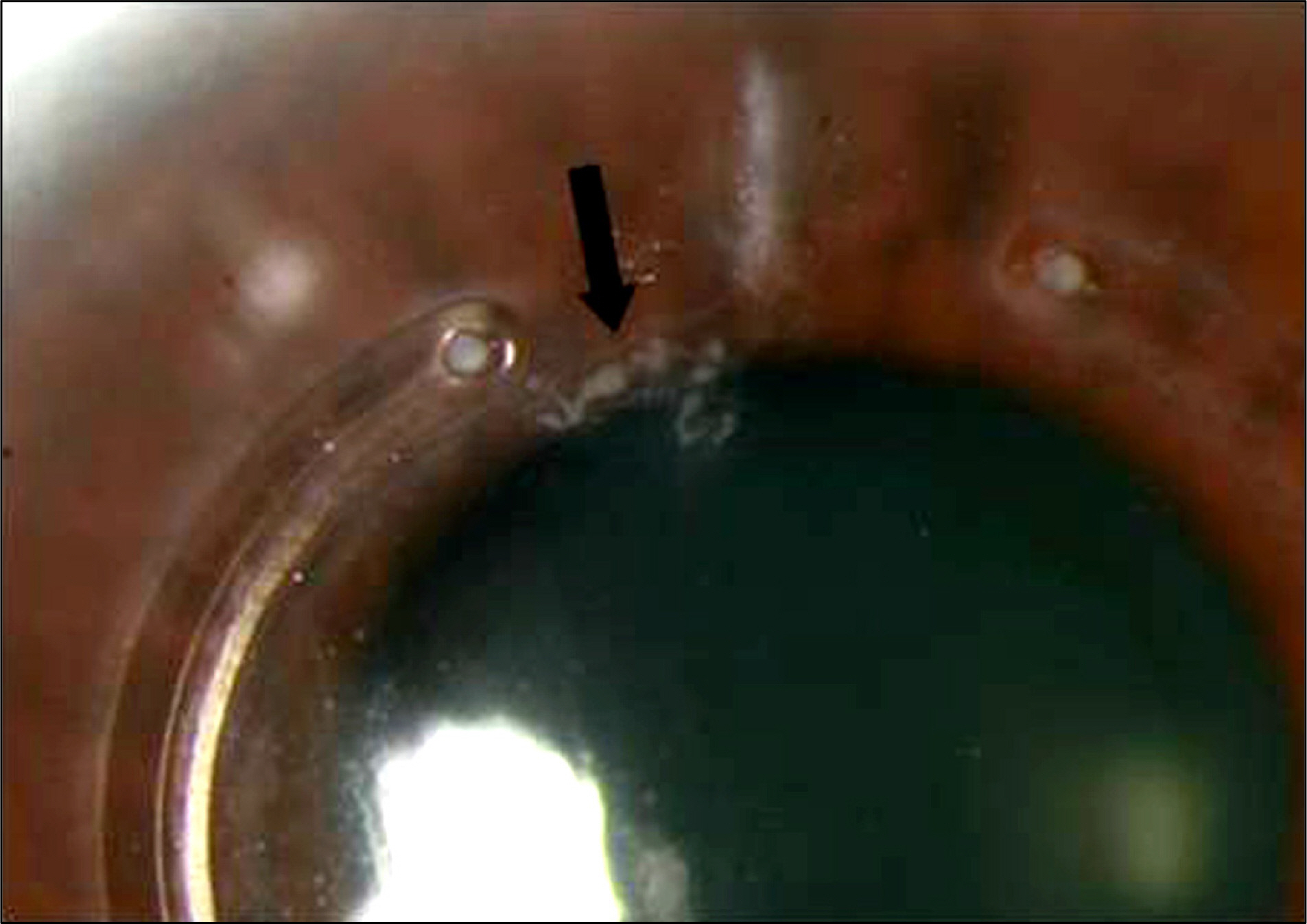
Figure
Reference
-
References
1. Krachmer JH, Feder RS, Belin MW. Keratoconus and related non-inflammatory corneal thinning disorders. Surv Ophthalmol. 1984; 28:293–322.
Article2. Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998; 42:297–319.
Article3. Kim MK, Lee JH. Long-term outcome of graft rejection after penetrating keratoplasty. J Korean Ophthalmol Soc. 1997; 38:1553–60.4. Doyle SJ, Hynes E, Naroo S, Shah S. PRK in patients with a keratoconic topography picture. The concept of a physiological ‘displaced apex syndrome’. Br J Ophthalmol. 1996; 80:25–8.
Article5. Kremer I, Shochot Y, Kaplan A, Blumenthal M. Three year results of photoastigmatic refractive keratectomy for mild and atypical keratoconus. J Cataract Refract Surg. 1998; 24:1581–8.
Article6. Boxer Wachler BS, Christie JP, Chandra NS, et al. Intacs for keratoconus. Ophthalmology. 2003; 110:1031–40.
Article7. Kymionis GD, Tsiklis NS, Pallikaris AI, et al. Long-term followup of Intacs for post-LASIK corneal ectasia. Ophthalmology. 2006; 113:1909–17.
Article8. Coskunseven E, Kymionis GD, Tsiklis NS, et al. One-year results of intrastromal corneal ring segment implantation (KeraRing) using femtosecond laser in patients with keratoconus. Am J Ophthalmol. 2008; 145:775–9.
Article9. Shabayek MH, Alió JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction. Ophthalmology. 2007; 114:1643–52.
Article10. Maguire LJ, Lowry JC. Identifying progression of subclinical keratoconus by serial topography analysis. Am J Ophthalmol. 1991; 112:41–5.
Article11. Nosé W, Neves RA, Schanzlin DJ, Belfort Júnior R. Intrastromal corneal ring–one-year results of first implants in humans: a pre-liminary nonfunctional eye study. Refract Corneal Surg. 1993; 9:452–8.
Article12. Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000; 26:1117–22.
Article13. Alió JL, Artola A, Ruiz-Moreno JM, et al. Changes in keratoconic corneas after intracorneal ring segment explantation and reimplantation. Ophthalmology. 2004; 111:747–51.14. Alió JL, Shabayek MH, Artola A. Intracorneal ring segments for keratoconus correction: long-term followup. J Cataract Refract Surg. 2006; 32:978–85.
Article15. Patel S, Marshall J, Fitzke FW 3rd. Model for deriving the optical performance of the myopic eye corrected with an intracorneal ring. J Refract Surg. 1995; 11:248–52.16. Alió JL, Artola A, Hassanein A, et al. One or 2 Intacs segments for the correction of keratoconus. J Cataract Refract Surg. 2005; 31:943–53.
Article17. Colin J. European clinical evaluation: use of Intacs for the treatment of keratoconus. J Cataract Refract Surg. 2006; 32:747–55.
Article18. Colin J, Malet FJ. Intacs for the correction of keratoconus: two-year followup. J Cataract Refract Surg. 2007; 33:69–74.
Article19. Rabinowitz YS, Li X, Ignacio TS, Maguen E. INTACS inserts using the femtosecond laser compared to the mechanical spreader in the treatment of keratoconus. J Refract Surg. 2006; 22:764–71.
Article20. Kwitko S, Severo NS. Ferrara intracorneal ring segments for keratoconus. J Cataract Refract Surg. 2004; 30:812–20.
Article21. Siganos D, Ferrara P, Chatzinikolas K, et al. Ferrara intrastromal corneal rings for the correction of keratoconus. J Cataract Refract Surg. 2002; 28:1947–51.
Article22. Alió JL, Shabayek MH, Belda JI, et al. Analysis of results related to good and bad outcomes of Intacs implantation for keratoconus correction. J Cataract Refract Surg. 2006; 32:756–61.
Article23. Colin J, Cochener B, Savary G, et al. INTACS inserts for treating keratoconus: one-year results. Ophthalmology. 2001; 108:1409–14.24. Hellstedt T, Mäkelä J, Uusitalo R, et al. Treating keratoconus with intacs corneal ring segments. J Refract Surg. 2005; 21:236–46.
Article25. Kanellopoulos AJ, Pe LH, Perry HD, Donnenfeld ED. Modified intracorneal ring segment implantations (INTACS) for the management of moderate to advanced keratoconus: efficacy and complications. Cornea. 2006; 25:29–33.
Article26. Kymionis GD, Siganos CS, Tsiklis NS, et al. Long-term followup of Intacs in keratoconus. Am J Ophthalmol. 2007; 143:236–44.
Article27. Miranda D, Sartori M, Francesconi C, et al. Ferrara intrastromal corneal ring segments for severe keratoconus. J Refract Surg. 2003; 19:645–53.
Article28. Siganos CS, Kymionis GD, Kartakis N, et al. Management of keratoconus with Intacs. Am J Ophthalmol. 2003; 135:64–70.
Article29. Zare MA, Hashemi H, Salari MR. Intracorneal ring segment implantation for the management of keratoconus: safety and efficacy. J Cataract Refract Surg. 2007; 33:1886–91.
Article30. Ertan A, Bahadir M. Topography-guided vertical implantation of Intacs using a femtosecond laser for the treatment of keratoconus. J Cataract Refract Surg. 2007; 33:148–51.
Article31. Ertan A, Kamburoğ lu G, Bahadir M. Intacs insertion with the femtosecond laser for the management of keratoconus: one-year results. J Cataract Refract Surg. 2006; 32:2039–42.32. Piñero DP, Alio JL, El Kady B, et al. Refractive and aberrometric outcomes of intracorneal ring segments for keratoconus: mechanical versus femtosecond-assisted procedures. Ophthalmology. 2009; 116:1675–87.
Article33. Budo C, Bartels MC, van Rij G. Implantation of Artisan toric phakic intraocular lenses for the correction of astigmatism and spherical errors in patients with keratoconus. J Refract Surg. 2005; 21:218–22.
Article34. Colin J, Velou S. Implantation of Intacs and a refractive intraocular lens to correct keratoconus. J Cataract Refract Surg. 2003; 29:832–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sequential Intrastromal Corneal Ring Implantation and Cataract Surgery in a Severe Keratoconus Patient with Cataract
- The Clinical Results of Intacs(R) Ring Implantation by Manual Tunnel Creation in Patients with Keratoconus
- Clinical Results of Intacs(R) Ring Implantation in Keratoconus or Keratectasia
- The Clinical Results of Intrastromal Corneal Ring Segment Implantation Using a Femtosecond Laser in Keratectasia
- Effect of Sequential Intrastromal Corneal Ring Segment Implantation and Corneal Collagen Crosslinking in Corneal Ectasia