J Korean Ophthalmol Soc.
2015 Apr;56(4):499-508. 10.3341/jkos.2015.56.4.499.
Clinical Results of Intacs(R) Ring Implantation in Keratoconus or Keratectasia
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. Kmk9@snu.ac.kr
- 2Laboratory of Ocular Regenerative Medicine and Immunology, Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- KMID: 2215699
- DOI: http://doi.org/10.3341/jkos.2015.56.4.499
Abstract
- PURPOSE
To report the clinical results after the implantation of intrastromal corneal ring segments (Intacs(R)) for the correction of keratoconus or keratectasia.
METHODS
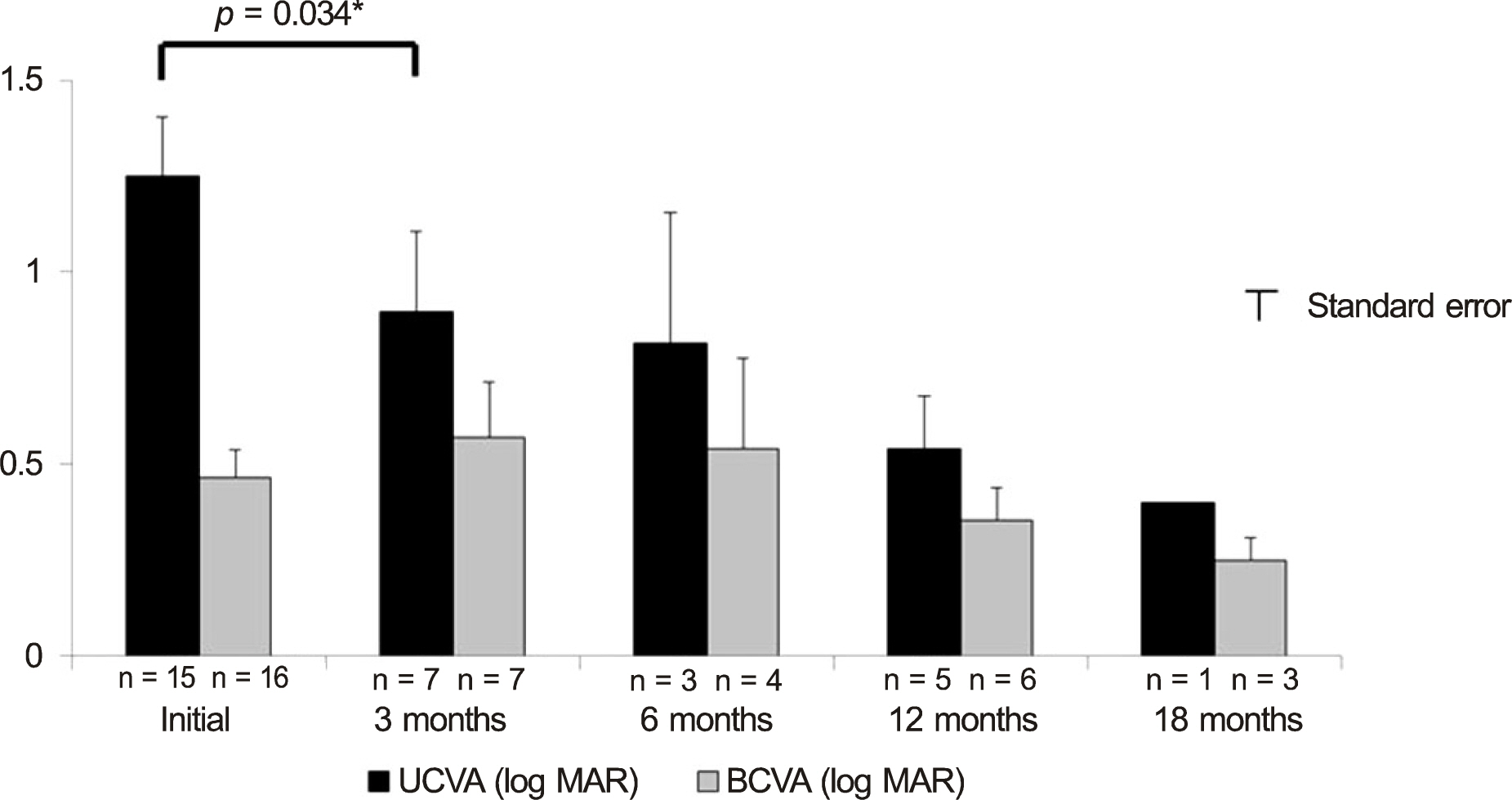
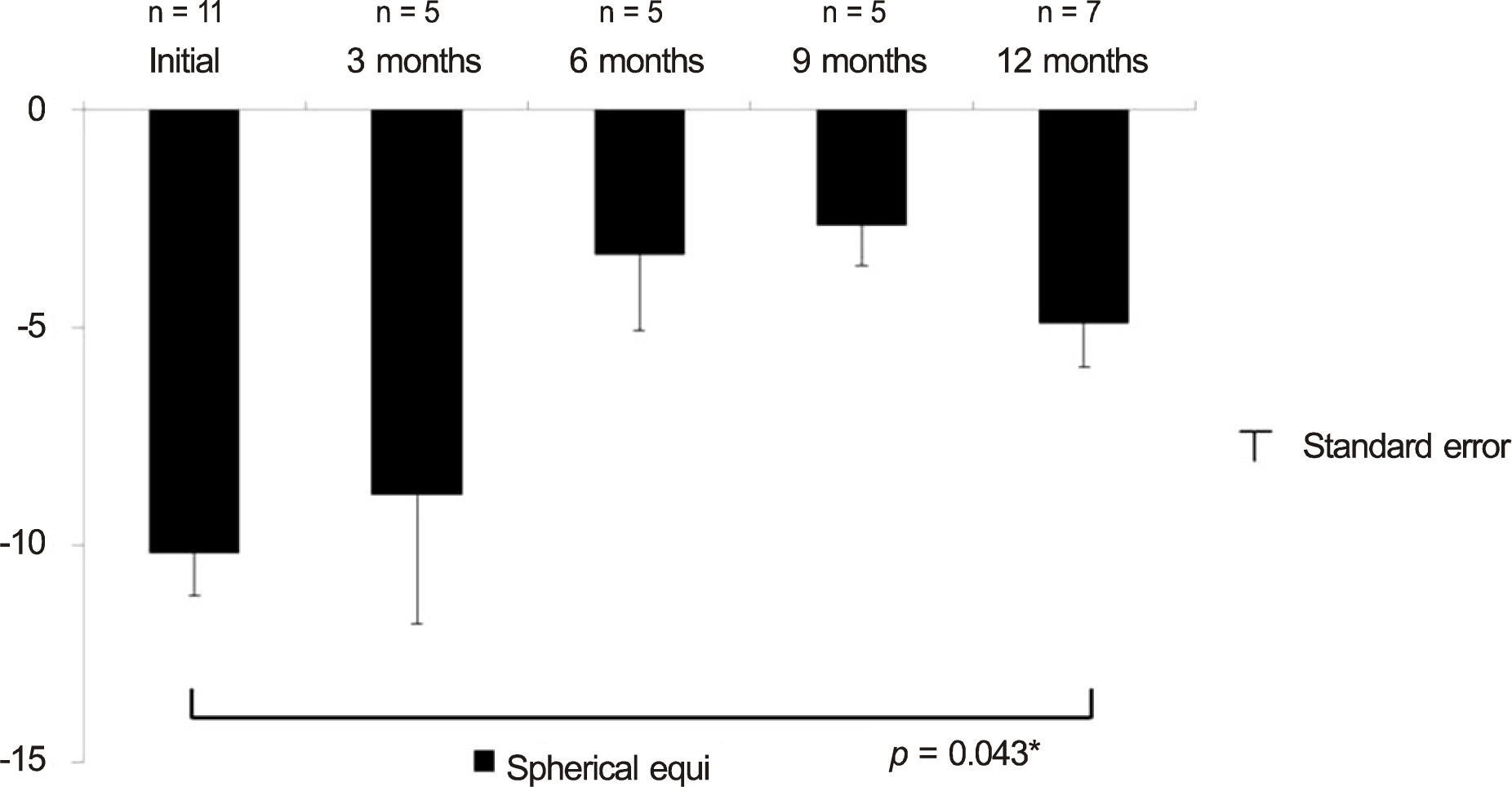
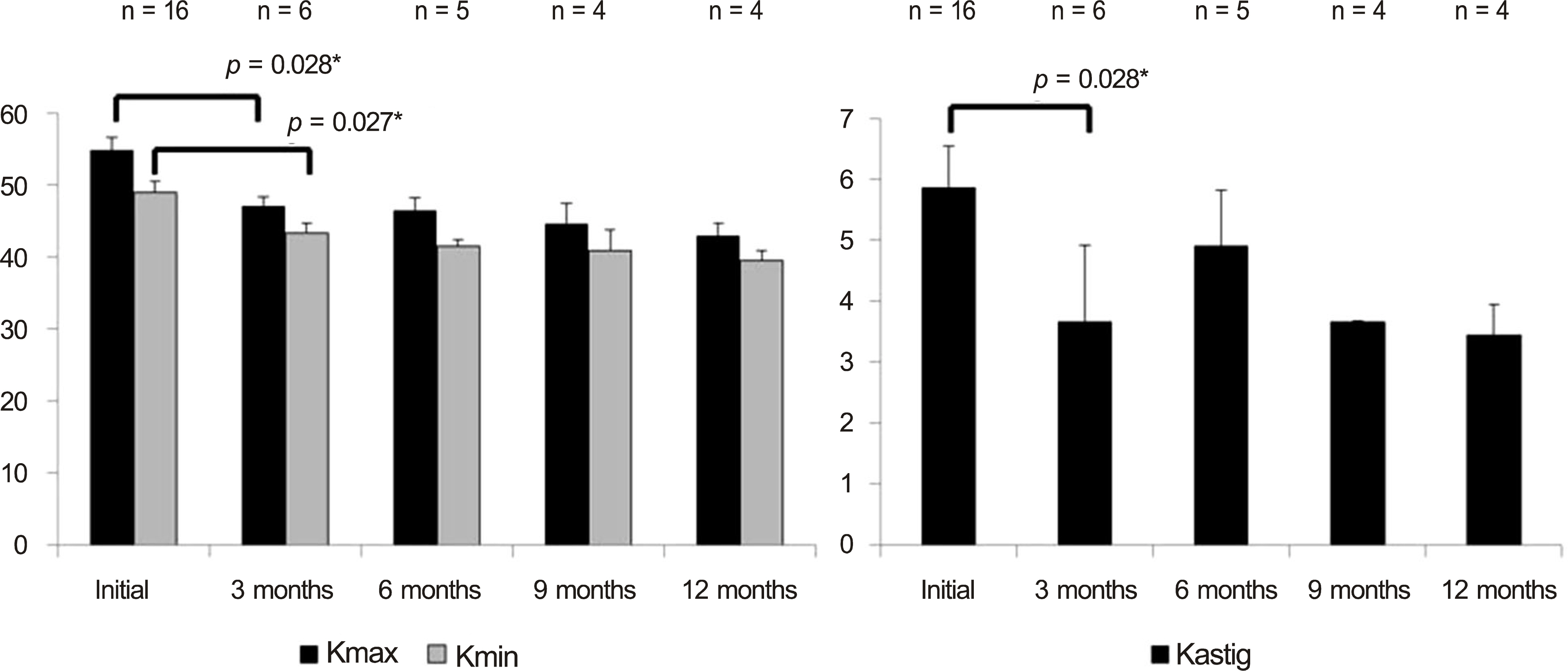
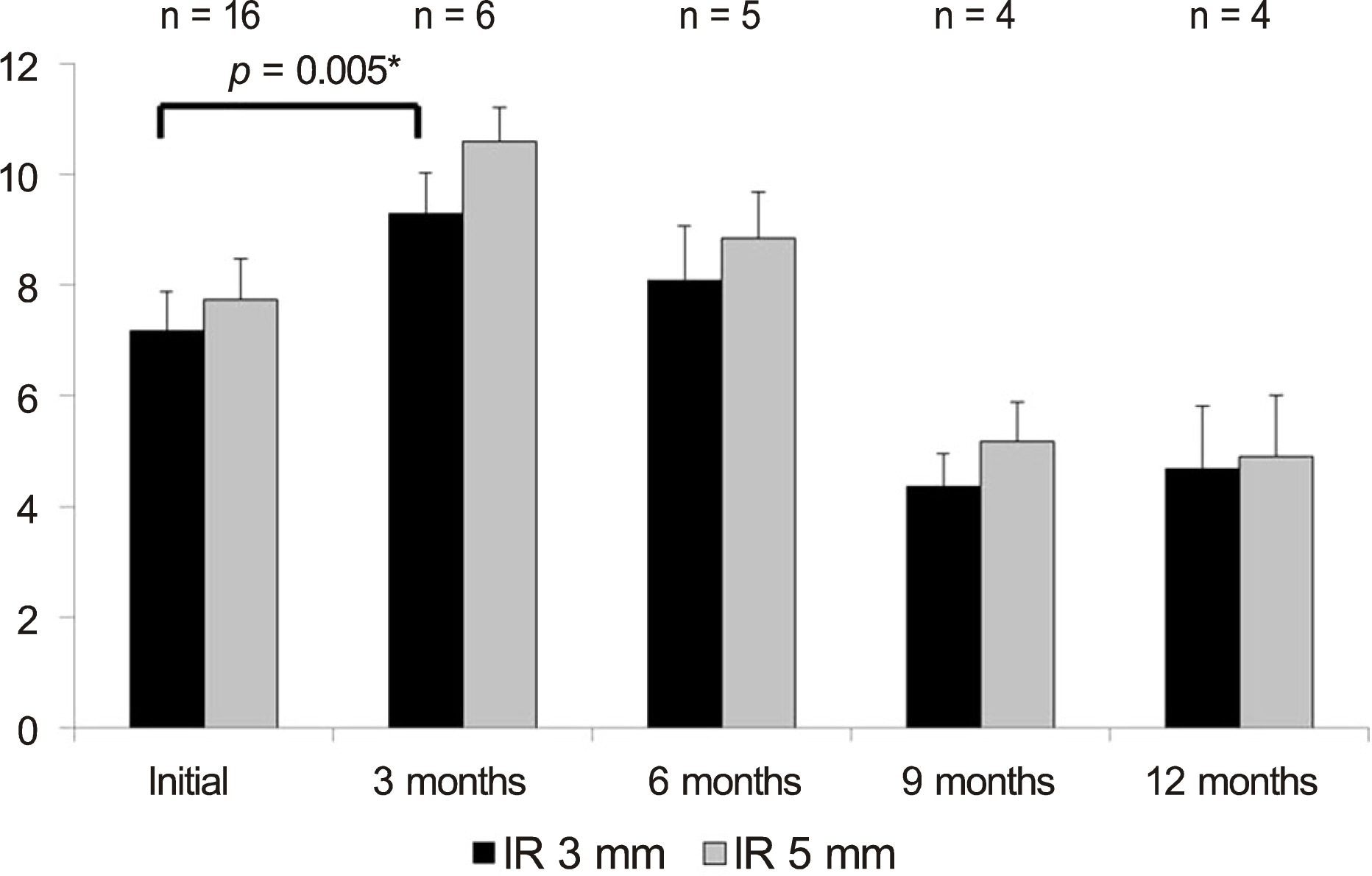
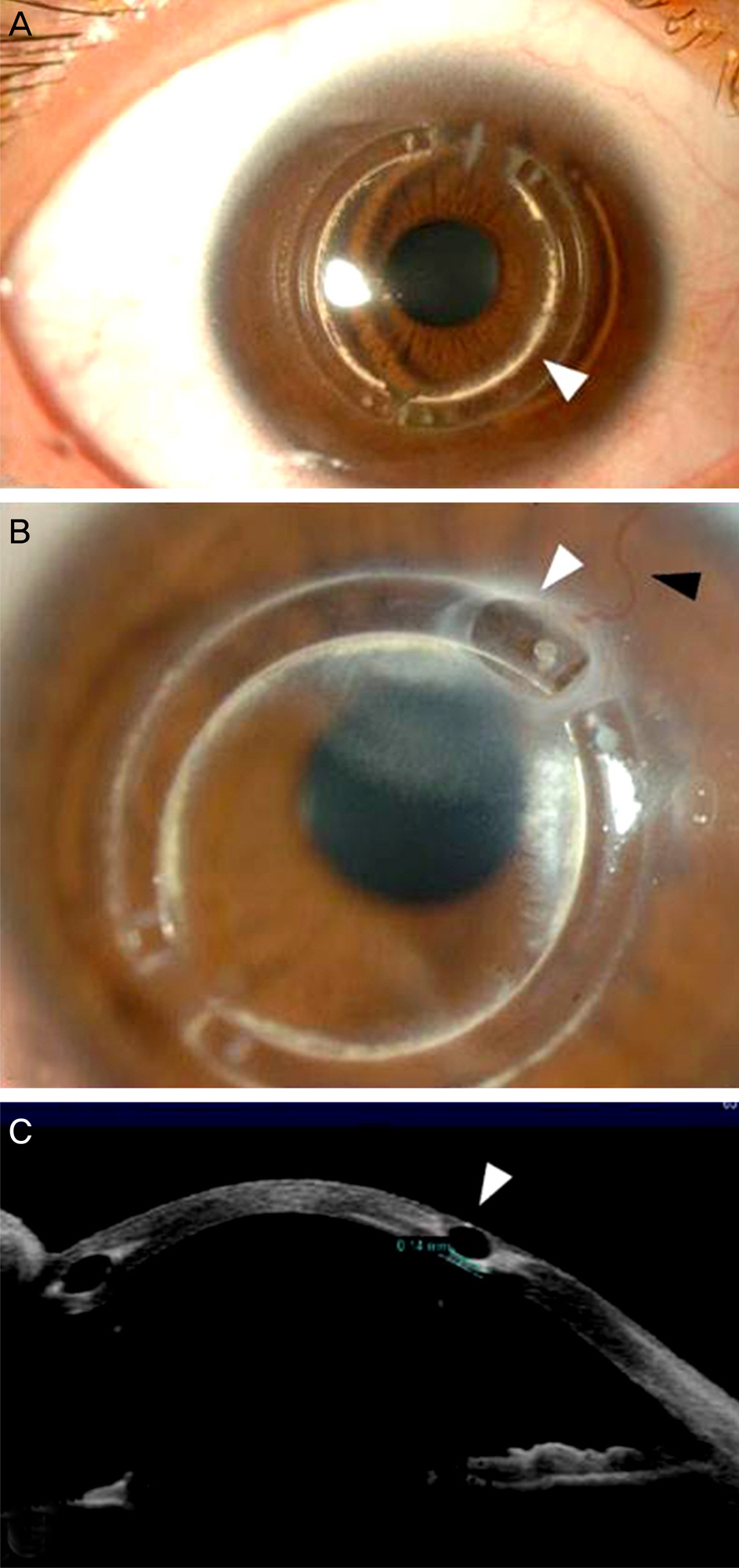
This retrospective study was comprised of 16 eyes treated by insertion of intrastromal corneal ring and 30 eyes treated by penetrating keratoplasty (PKP) who were diagnosed with keratoconus or keratectasia. Visual acuity, refractive outcome, keratometric values were evaluated before and at 3 months, 6 months, and 12 months postoperatively. In addition, the implanted ring segment depth was measured by anterior segment optical coherence tomography and the results were compared based on the depth of the ring.
RESULTS
Twelve months after treatment, best corrected visual acuity (BCVA) was log MAR 0.32 at the ring group and log MAR 0.20 at the PKP group. BCVA change was larger at the PKP group than the ring group. Postoperative keratometric value was smaller at the ring group than at the PKP group. 3 mm irregular astigmatism was larger at the ring group than at the PKP group. The shallowly implanted ring group had a larger effect than the deeply implanted ring group.
CONCLUSIONS
Intrastromal corneal ring segment implantation appears to be effective in improving the visual acuity and refractive outcome, although it cannot substitute for PKP.
MeSH Terms
Figure
Reference
-
References
1. Kenney MC, Brown DJ, Rajeev B. Everett Kinsey lecture. The elu-sive causes of keratoconus: a working hypothesis. CLAO J. 2000; 26:10–3.2. Troutman RC, Gaster RN. Surgical advances and results of keratoconus. Am J Ophthalmol. 1980; 90:131–6.
Article3. Wagoner MD, Ba-Abbad R, Al-Mohaimeed M, et al. Postoperative complications after primary adult optical penetrating keratoplasty: prevalence and impact on graft survival. Cornea. 2009; 28:385–94.
Article4. Wollensak G, Spoerl E, Reber F, Seiler T. Keratocyte cytotoxicity of riboflavin/UVA-treatment in vitro. Eye (Lond). 2004; 18:718–22.
Article5. Godoy CS, Wahab SA, Moreira H, et al. [Analysis of corneal curvature alteration following intrastromal corneal ring implantation: experimental study in rabbits]. Arq Bras Oftalmol. 2007; 70:303–11.6. Kim EJ, Koo SH, Lee GJ, et al. The clinical results of Intacs(R) ring implantation by manual tunnel creation in patients with keratoconus. J Korean Ophthalmol Soc. 2012; 53:1756–65.7. Kim HS, Lee TH, Lee KH. Intracorneal ring segment implantation for the management of keratoconus: short-term safety and efficacy. J Korean Ophthalmol Soc. 2009; 50:1505–9.
Article8. Torquetti L, Ferrara G, Almeida F, et al. Intrastromal corneal ring segments implantation in patients with keratoconus: 10-year fol-low-up. J Refract Surg. 2014; 30:22–6.
Article9. Siganos D, Ferrara P, Chatzinikolas K, et al. Ferrara intrastromal corneal rings for the correction of keratoconus. J Cataract Refract Surg. 2002; 28:1947–51.
Article10. McMahon TT, Szczotka-Flynn L, Barr JT, et al. A new method for grading the severity of keratoconus: the Keratoconus Severity Score (KSS). Cornea. 2006; 25:794–800.11. Thibos LN, Horner D. Power vector analysis of the optical outcome of refractive surgery. J Cataract Refract Surg. 2001; 27:80–5.
Article12. Fleming JF, Wan WL, Schanzlin DJ. The theory of corneal curvature change with the Intrastromal Corneal Ring. CLAO J. 1989; 15:146–50.13. Twa MD, Karpecki PM, King BJ, et al. One-year results from the phase III investigation of the KeraVision Intacs. J Am Optom Assoc. 1999; 70:515–24.14. Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000; 26:1117–22.
Article15. Torquetti L, Berbel RF, Ferrara P. Long-term follow-up of intrastromal corneal ring segments in keratoconus. J Cataract Refract Surg. 2009; 35:1768–73.
Article16. Coskunseven E, Kymionis GD, Tsiklis NS, et al. One-year results of intrastromal corneal ring segment implantation (KeraRing) using femtosecond laser in patients with keratoconus. Am J Ophthalmol. 2008; 145:775–9.
Article17. Piñero DP, Alio JL, El Kady B, et al. Refractive and aberrometric outcomes of intracorneal ring segments for keratoconus: mechan-ical versus femtosecond-assisted procedures. Ophthalmology. 2009; 116:1675–87.
Article18. Coskunseven E, Jankov MR 2nd, Hafezi F, et al. Effect of treatment sequence in combined intrastromal corneal rings and corneal collagen crosslinking for keratoconus. J Cataract Refract Surg. 2009; 35:2084–91.
Article19. MacIntyre R, Chow SP, Chan E, Poon A. Long-term outcomes of deep anterior lamellar keratoplasty versus penetrating keratoplasty in Australian keratoconus patients. Cornea. 2014; 33:6–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracorneal Ring Segment Implantation for the Management of Keratoconus: Short-Term Safety and Efficacy
- The Clinical Results of Intacs(R) Ring Implantation by Manual Tunnel Creation in Patients with Keratoconus
- The Clinical Results of Intrastromal Corneal Ring Segment Implantation Using a Femtosecond Laser in Keratectasia
- A Case of Fungal Keratitis after Intracorneal Ring Segment Implantation for Keratoconus
- A Case of Keratectasia 5 Years after Photorefractive Keratectomy