J Korean Ophthalmol Soc.
2010 Jan;51(1):1-7.
The Clinical Results of Intrastromal Corneal Ring Segment Implantation Using a Femtosecond Laser in Keratectasia
- Affiliations
-
- 1Department of Ophthalmology, Ilsan Paik Hospital, Inje University College of Medicine, Ilsan, Korea. jhk0924@hanmail.net
Abstract
- PURPOSE
To evaluate the clinical results of intrastromal ring segment (Keraring(R)) implantation using a femtosecond laser in patients with keratectasia.
METHODS
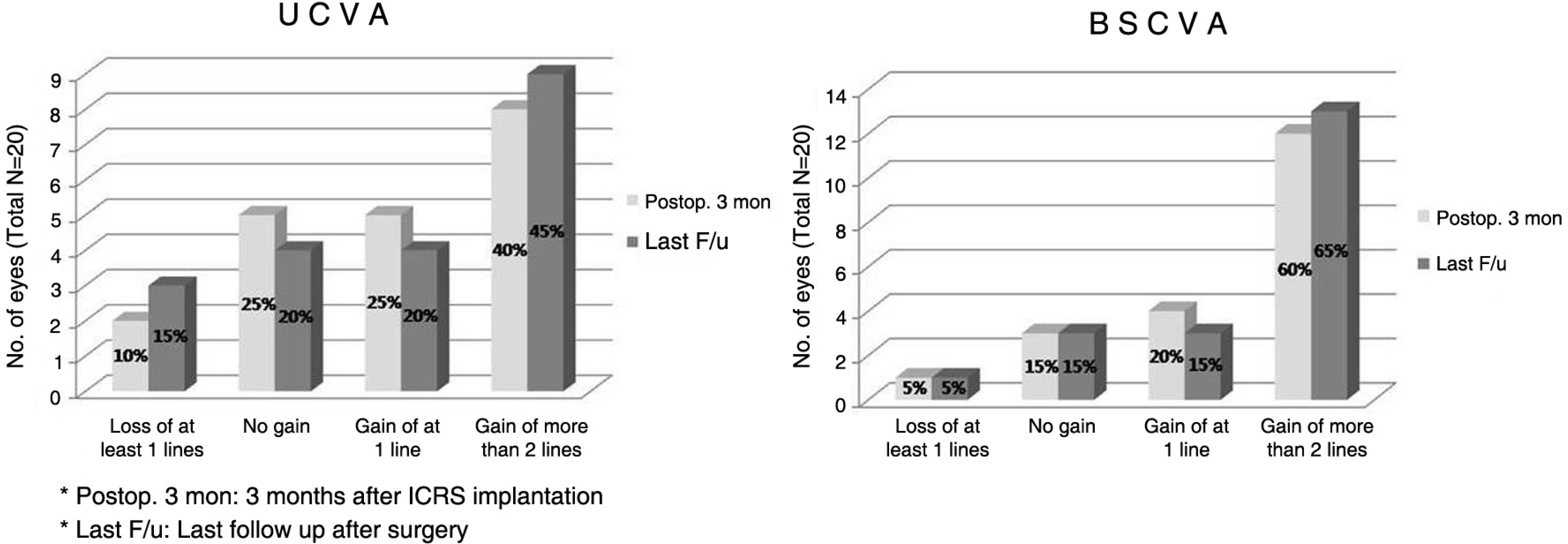
Twenty eyes of 19 keratectatic patients (15 eyes of keratoconus and five eyes of post-LASIK keratectasia) who completed at least three months of postoperative follow-up were included in this study. Uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BSCVA), spherical equivalent, keratometric value, corneal astigmatism, corneal higher order aberrations (HOA) and specular microscopy were determined or performed before and after surgery. In addition, intraoperative and postoperative adverse complications were recorded.
RESULTS
UCVA improved in 13 out of 20 eyes (65%), and BSCVA improved in 16 out of 20 eyes (80%). At the postoperative examination there was no statistically significant reduction in the spherical equivalent with that observed at the examination before implantation. Conversely, there were statistically significant reductions in topographic mean K value and Sim K astigmatism, corneal total and coma-like HOA (p<0.05). On specular microscopy, there was no statistically significant difference between preoperative and postoperative endothelial cell density. There was one case of partial Descemet membrane detachment and one case of microperforation as a complication during surgery, which recovered over time without any treatment.
CONCLUSION
Keraring(R) implantation appears to be an effective and safe procedure for improving visual acuity and stabilizing corneal refractive power in keratectactic patients.
MeSH Terms
Figure
Reference
-
References
1. Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998; 42:297–319.
Article2. Kim HJ, Cho SH, Kim JH, Joo CK. Risk factors and clinical aberrations for corneal ectasia after LASIK. J Korean Ophthalmol Soc. 2005; 46:589–96.3. Kim HJ, Song IK, Joo CK. Keratectasia after laser in situ aberrations: clinicopathologic case report. J Korean Ophthalmol Soc. 2005; 46:910–4.4. Kymionis GD, Siganos CS, Kounis G, et al. Management of post-LASIK corneal ectasia with intacts inserts. Arch Ophthalmol. 2003; 121:322–6.5. Kymionis GD, Tsiklis NS, Pallikaris AI, et al. Long-term follow-up of Intacs for post-LASIK corneal ectasia. Ophthalmology. 2006; 113:1909–17.
Article6. Kymionis GD, Siganos CS, Tsiklis NS, et al. Long-term follow-up of Intacs in keratoconus. Am J Ophthalmol. 2007; 143:236–44.
Article7. Krachmer JH, Feder RS, Belin MW. Keratoconus and related non-inflammatory corneal thinning disorders. Surv Ophthalmol. 1984; 28:293–322.
Article8. Edrington TB, Szczotka LB, Barr JT, et al. Rigid contact lens fitting relationships in keratoconus. collaborative longitudinal evaluation of keratoconus (CLEK) study group. Optom Vis Sci. 1999; 76:692–9.9. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J aberrations. 2003; 135:620–7.
Article10. Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000; 26:1117–22.
Article11. Hellstedt T, Makela J, Uusitalo R, et al. Treating keratoconus with Intacs corneal ring segments. J Refract Surg. 2005; 21:236–46.
Article12. Alió JL, Artola A, Hassanein A, et al. One or two Intacs segments for the correction of keratoconus. J Cataract Refract Surg. 2005; 31:943–53.13. Burris TE, Ayer CT, Evensen DA, Davenport JM. Effects of intrastromal corneal ring size and thickness on corneal flattening in human eyes. Refract Corneal Surg. 1991; 7:46–50.
Article14. Burris TE, Baker PC, Ayer CT, et al. Flattening of central corneal curvature with intrastromal corneal rings of increasing thickness: an eye-bank eye study. J Cataract Refract Surg. 1993; 19:182–7.
Article15. Siganos CS, Kymionis GD, Kartakis N, et al. Management of keratoconus with Intacs. Am J Ophthalmol. 2003; 135:64–70.
Article16. Shabayek MH, Alió JL. Intrastromal corneal ring segment aberrations by femtosecond laser for keratoconus correction. aberrationsmology. 2007; 114:1643–52.17. Coskunseven E, Kymionis GD, Tsiklis NS, et al. One-year result of intrastromal corneal ring segment implantation(Keraring) aberrations femtosecond laser in patients with keratoconus. Am J aberrations. 2008; 145:775–9.18. Ertan A, Kamburoglu G, Bahadir M. Intacs insertion with the aberrations laser for the management of keratoconus: one-year aberrations. J Cataract Refract Surg. 2006; 32:2039–42.19. Ertan A, Bahadir M. Topography-guided vertical implantation of Intacs using a femtosecond laser for the treatment of keratoconus. J Cataract Refract Surg. 2007; 33:148–51.
Article20. Carrasquillo KG, Rand J, Talamo JH. Intacs for keratoconus and post-LASIK ectasia: mechanical versus femtosecond laser-assisted channel creation. Cornea. 2007; 26:956–62.21. Hiraoka T, Okamoto C, Ishii Y, et al. Time course of changes in ocular higher-order aberrations and contrast sensitivity after aberrations orthokeratology. Invest Ophthalmol Vis Sci. 2008; 49:4314–20.22. Siganos D, Ferrara P, Chatzinikolas K, et al. Ferrara intrastromal corneal rings for the correction of keratoconus. J Cataract Refract Surg. 2002; 28:1947–51.
Article23. Kwitko S, Severo NS. Ferrara intracorneal ring segments for aberrations. J Cataract Refract Surg. 2004; 30:812–20.24. Dua HS, Azuara-Blanco A. Corneal allograft rejection: risk aberrations, diagnosis, prevention, and treatment. Indian J Ophthalmol. 1999; 47:3–9.25. Colin J, Velou S. Utilization of refractive surgery technology in keratoconus and corneal transplants. Curr Opin Ophthalmol. 2002; 13:230–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Results of Intacs(R) Ring Implantation in Keratoconus or Keratectasia
- Effect of Sequential Intrastromal Corneal Ring Segment Implantation and Corneal Collagen Crosslinking in Corneal Ectasia
- Sequential Intrastromal Corneal Ring Implantation and Cataract Surgery in a Severe Keratoconus Patient with Cataract
- The Clinical Results of Intacs(R) Ring Implantation by Manual Tunnel Creation in Patients with Keratoconus
- Surgical treatment for myopia