J Korean Soc Spine Surg.
2012 Dec;19(4):145-151. 10.4184/jkss.2012.19.4.145.
The Association of Lumbosacral Sagittal Alignments and the Patterns of Lumbar Disc Degeneration
- Affiliations
-
- 1Department of Orthopaedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Orthopaedic Surgery, National Medical Center, Seoul, Korea. 1435man@hanmail.net
- KMID: 2209549
- DOI: http://doi.org/10.4184/jkss.2012.19.4.145
Abstract
- STUDY DESIGN: Retrospective review and radiological analysis.
OBJECTIVES
We investigated whether the lumbosacral sagittal curvature have any relation to the patterns of lumbar disc degeneration. SUMMARY OF THE LITERATURE REVIEW: Recently, there have been many studies on the correlations between the changes of lumbar disc degeneration and associated factors, such as age, gender, weight, occupation, cigarette smoking, and genetics; but, it is hard to find research into lumbosacral sagittal alignments.
MATERIALS AND METHODS
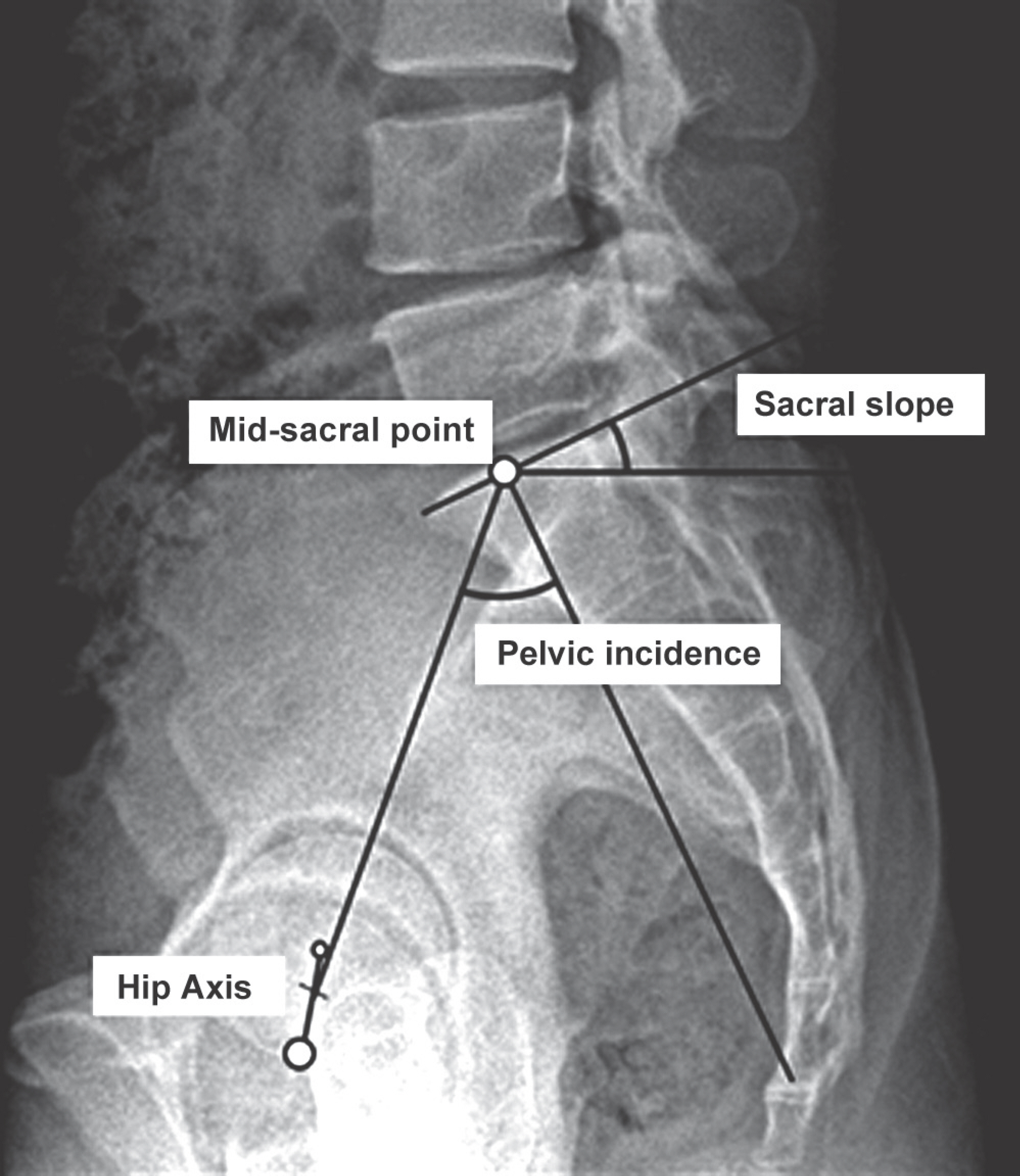
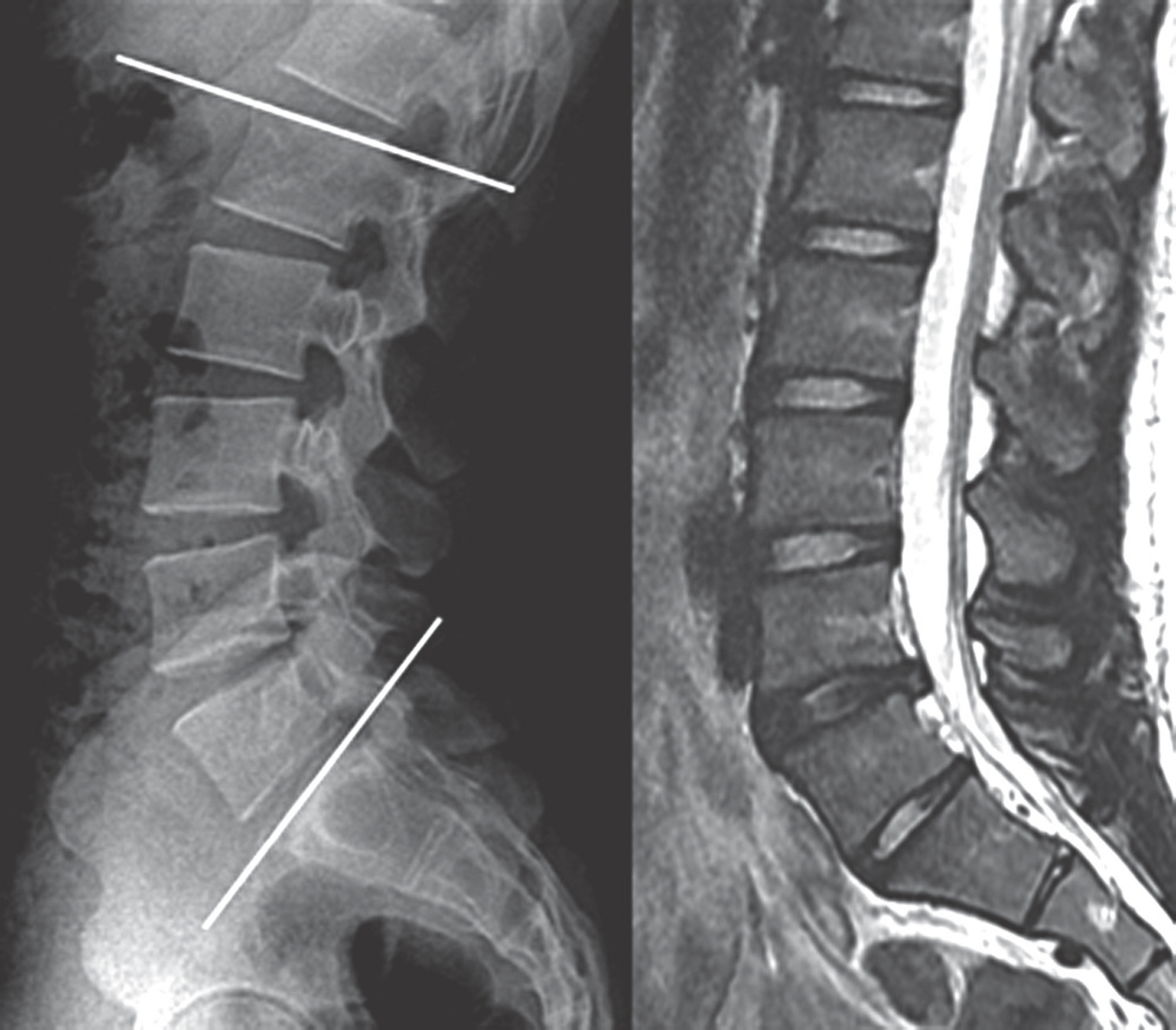
This study enrolled 117 young adult patients limited by age (18-35 years), BMD (<30kg/m2), no smoking, occupation except heavy worker, no prior lumbar surgery and no combined spinal deformity. By measuring the pelvic incidence, sacral slope, lumbar tilt angle, lumbar lordosis and lumbar axis indicating the parameters of sagittal alignments, we investigated the correlation between the number and severity of lumbar disc degeneration and the number of herniated intervertebral discs.
RESULTS
This study found a moderate correlation between pelvic incidence, sacral slope, lumbar lordosis, and the number of lumbardegenerative disc (r=-0.451, p<0.001; r=-0.433, p<0.001; r=-0.425, p<0.001). We calculated the most proper cut-off value of pelvic incidence associated with more than three segments of multiple lumbar disc degeneration, using a minimum p-value approach.
CONCLUSIONS
As pelvic incidence, sacral slope, and lumbar lordosis indicating the parameters of lumbosacral sagittal alignments get smaller, the numbers of lumbar disc degenerations and herniated intervertebral discs increase. When pelvic incidence is below 45.6 degrees, it is more likely for degenerative changes of lumbar disc to affect more than three segments.
MeSH Terms
Figure
Cited by 1 articles
-
The Role of the Pelvis in Sagittal Alignment of Lumbar Degenerative Disease Patients
Yong-Chan Kim, Ki-Han You, Chulyoung Jang, Ji Hao Cui, Sirichai Wilartratsami, Tae-Hwan Kim, Jae-Keun Oh, Moon-Soo Park, Seok Woo Kim
J Korean Soc Spine Surg. 2016;23(2):131-138. doi: 10.4184/jkss.2016.23.2.131.
Reference
-
1.Salminen JJ., Erkintalo MO., Pentti J., Oksanen A., Kormano MJ. Recurrent low back pain and early disc degeneration in the young. Spine (Phila Pa 1976). 1999. 24:1316–21.
Article2.Bezer M., Erol B., Kocaoglu B, et al. [Low back pain among children and adolescents]. Acta Orthop Traumatol Turc. 2004. 38:136–44.3.Videman T., Battie MC. The influence of occupation on lumbar degeneration. Spine (Phila Pa 1976). 1999. 24:1164–8.4.Ala-Kokko L. Genetic risk factors for lumbar disc disease. Ann Med. 2002. 34:42–7.
Article5.Elfering A., Semmer N., Birkhofer D., Zanetti M., Hodler J., Boos N. Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine (Phila Pa 1976). 2002. 27:125–34.6.Battie MC., Videman T. Lumbar disc degeneration: epidemiology and genetics. J Bone Joint Surg Am. 2006. 88(Suppl 2):3–9.7.Djurasovic MO., Carreon LY., Glassman SD., Dimar JR 2nd., Puno RM., Johnson JR. Sagittal alignment as a risk factor for adjacent level degeneration: a case-control study. Or-thopedics. 2008. 31:546.
Article8.Battie MC., Videman T., Gill K, et al. 1991 Volvo Award in clinical sciences. Smoking and lumbar intervertebral disc degeneration: an MRI study of identical twins. Spine (Phila Pa 1976). 1991. 16:1015–21.9.Sward L., Hellstrom M., Jacobsson B., Nyman R., Peterson L. Disc degeneration and associated abnormalities of the spine in elite gymnasts. A magnetic resonance imaging study. Spine (Phila Pa 1976). 1991. 16:437–43.10.Battié MC., Videman T., Gibbons LE., Fisher LD., Manninen H., Gill K. 1995 Volvo Award in clinical sciences. Determi-nants of lumbar disc degeneration. A study relating lifetime exposures and magnetic resonance imaging findings in identical twins. Spine (Phila Pa 1976). 2006. 88(Suppl):3–9.11.Ong A., Anderson J., Roche J. A pilot study of the prevalence of lumbar disc degeneration in elite athletes with lower back pain at the Sydney 2000 Olympic Games. Br J Sports Med. 2003. 37:263–6.
Article12.Liuke M., Solovieva S., Lamminen A, et al. Disc degeneration of the lumbar spine in relation to overweight. Int J Obes (Lond). 2005. 29:903–8.
Article13.Rajnics P., Templier A., Skalli W., Lavaste F., Illes T. The im-portance of spinopelvic parameters in patients with lumbar disc lesions. Int Orthop. 2002. 26:104–8.14.Barrey C., Jund J., Noseda O., Roussouly P. Sagittal bal-ance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007. 16:1459–67.
Article15.Ergun T., Lakadamyali H., Sahin MS. The relation between sagittal morphology of the lumbosacral spine and the degree of lumbar intervertebral disc degeneration. Acta Orthop Traumatol Turc. 2010. 44:293–9.
Article16.Schneiderman G., Flannigan B., Kingston S., Thomas J., Dillin WH., Watkins RG. Magnetic resonance imaging in the di-agnosis of disc degeneration: correlation with discography. Spine (Phila Pa 1976). 1987. 12:276–81.17.Kawaguchi Y., Kanamori M., Ishihara H., Ohmori K., Matsui H., Kimura T. The association of lumbar disc disease with vitamin-D receptor gene polymorphism. J Bone Joint Surg Am. 2002. 84-A:2022–8.
Article18.Cheung KM., Chan D., Karppinen J, et al. Association of the Taq I allele in vitamin D receptor with degenerative disc disease and disc bulge in a Chinese population. Spine (Phila Pa 1976). 2006. 31:1143–8.
Article19.Sambrook PN., MacGregor AJ., Spector TD. Genetic influences on cervical and lumbar disc degeneration: a magnetic resonance imaging study in twins. Arthritis Rheum. 1999. 42:366–72.
Article20.Solovieva S., Lohiniva J., Leino-Arjas P, et al. COL9A3 gene polymorphism and obesity in intervertebral disc degeneration of the lumbar spine: evidence of gene-environment interaction. Spine (Phila Pa 1976). 2002. 27:2691–6.
Article21.Battie MC., Videman T., Parent E. Lumbar disc degeneration: epidemiology and genetic influences. Spine (Phila Pa 1976). 2004. 29:2679–90.22.Seki S., Kawaguchi Y., Chiba K, et al. A functional SNP in CILP, encoding cartilage intermediate layer protein, is associated with susceptibility to lumbar disc disease. Nat Genet. 2005. 37:607–12.
Article23.Videman T., Sarna S., Battie MC, et al. The long-term effects of physical loading and exercise lifestyles on back-related symptoms, disability, and spinal pathology among men. Spine (Phila Pa 1976). 1995. 20:699–709.
Article24.Miyakoshi N., Itoi E., Murai H., Wakabayashi I., Ito H., Mi-nato T. Inverse relation between osteoporosis and spon-dylosis in postmenopausal women as evaluated by bone mineral density and semiquantitative scoring of spinal degeneration. Spine (Phila Pa 1976). 2003. 28:492–5.
Article25.Jhawar BS., Fuchs CS., Colditz GA., Stampfer MJ. Cardio-vascular risk factors for physician-diagnosed lumbar disc herniation. Spine J. 2006. 6:684–91.
Article26.Lee CS., Lee CK., Kim YT., Hong YM., Yoo JH. Dynamic sagittal imbalance of the spine in degenerative flat back: significance of pelvic tilt in surgical treatment. Spine (Phila Pa 1976). 2001. 26:2029–35.27.Roussouly P., Gollogly S., Berthonnaud E., Dimnet J. Clas-sification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005. 30:346–53.
Article28.Lee CS., Chung SS., Kang KC., Park SJ., Shin SK. Normal patterns of Sagittal Alignment of the Spine in Young Adults Radiological analysis in a Korean population. Spine (Phila Pa 1976). 2011. 36:1648–54.
Article29.Duval-Beaupere G., Robain G. Visualization on full spine radiographs of the anatomical connections of the centres of the segmental body mass supported by each vertebra and measured in vivo. Int Orthop. 1987. 11:261–9.30.Lazennec JY., Ramare S., Arafati N, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000. 9:47–55.
Article31.Gelb DE., Lenke LG., Bridwell KH., Blanke K., McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976). 1995. 20:1351–8.
Article32.Legaye J., Duval-Beaupere G., Hecquet J., Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998. 7:99–103.
Article33.Jackson RP., Hales C. Congruent spinopelvic alignment on standing lateral radiographs of adult volunteers. Spine (Phila Pa 1976). 2000. 25:2808–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of the Various Configurations of Lower Lumbar and Lumbosacral Spine on the Disc Degeneration: Multifactorial Analysis
- Lumbosacral Sagittal Alignment in Association to Intervertebral Disc Diseases
- Analysis of the Sagittal Alignment of Normal Spines
- Correlation of Cervical Disc Degeneration with Sagittal Alignments of Cervical Spine
- Relative Contribution of Upper and Lower Lumbar Spinal Segments to Flexion/Extension: Comparison between Normal Spines and Spines with Disc Disease in Asian Patients