J Korean Med Assoc.
2013 Jul;56(7):583-591. 10.5124/jkma.2013.56.7.583.
The efficacy of dialysis adequacy
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University, Seoul, Korea.
- 2Department of Internal Medicine, The Catholic University of Korea, Seoul, Korea. yangch@catholic.ac.kr
- KMID: 2193048
- DOI: http://doi.org/10.5124/jkma.2013.56.7.583
Abstract
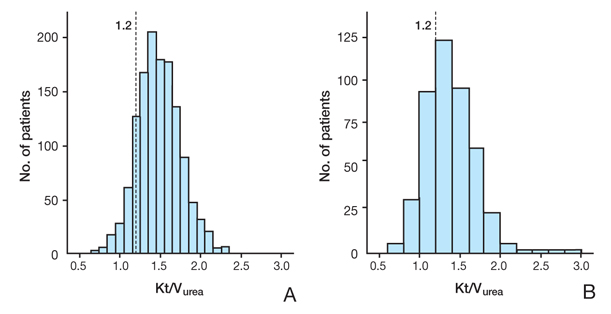
- Adequate dialysis is essential for improving dialysis therapies and reducing all-cause mortality in end-stage renal disease (ESRD) patients. Efficient removal of the uremic toxins in the blood remains the fundamental role of dialysis therapies. Therefore, urea clearance as assessed by urea kinetic modeling (Kt/Vurea) is a surrogate marker for dialysis adequacy in ESRD patients undergoing dialysis, and the NKF-DOQI recommends a Kt/Vurea of no less than 1.2. The current status of dialysis adequacy in Korea has not been fully investigated. Our Clinical Research Center for End Stage Renal Disease revealed that the mean Kt/Vurea in maintenance hemodialysis patients was 1.49+/-0.28, and 91.5% of patients satisfied the target level of Kt/Vurea. In addition to Kt/Vurea, clinical parameters such as the volume status, residual renal function, blood pressure, acid-base disorders, anemia, nutrition, inflammation, mineral metabolism, and middle molecule clearance are important for determining adequate dialysis treatment. Further evaluation of clinical parameters is needed to improve dialysis adequacy.
Keyword
MeSH Terms
Figure
Reference
-
1. Jin DC. Current status of dialysis therapy in Korea. Korean J Intern Med. 2011; 26:123–131.
Article2. Foley RN, Hakim RM. Why is the mortality of dialysis patients in the United States much higher than the rest of the world? J Am Soc Nephrol. 2009; 20:1432–1435.
Article3. Seok SJ, Kim JH, Gil HW, Yang JO, Lee EY, Hong SY. Comparison of patients starting hemodialysis with those underwent hemodialysis 15 years ago at the same dialysis center in Korea. Korean J Intern Med. 2010; 25:188–194.
Article4. Chin HJ. The chronic kidney disease in elderly population. J Korean Med Assoc. 2007; 50:549–555.
Article5. Vanholder R, De Smet R, Glorieux G, Argiles A, Baurmeister U, Brunet P, Clark W, Cohen G, De Deyn PP, Deppisch R, Descamps-Latscha B, Henle T, Jorres A, Lemke HD, Massy ZA, Passlick-Deetjen J, Rodriguez M, Stegmayr B, Stenvinkel P, Tetta C, Wanner C, Zidek W. European Uremic Toxin Work Group (EUTox). Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int. 2003; 63:1934–1943.
Article6. Choe TS, Kim SS, Kwon YJ, Cho WY, Kim HK, Woo DJ. Effect of continuous ambulatory peritoneal dialysis on beta-2-microglobulin in the patients with diabetic renal failure. Korean J Intern Med. 1991; 41:406–414.7. Kang SH, Park CW. Adequacy of dialysis: beyond Kt/V. Korean J Nephrol. 2010; 29:544–550.8. Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, Kusek JW, Allon M, Bailey J, Delmez JA, Depner TA, Dwyer JT, Levey AS, Levin NW, Milford E, Ornt DB, Rocco MV, Schulman G, Schwab SJ, Teehan BP, Toto R. Hemodialysis (HEMO) Study Group. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002; 347:2010–2019.
Article9. Depner T, Daugirdas J, Greene T, Allon M, Beck G, Chumlea C, Delmez J, Gotch F, Kusek J, Levin N, Macon E, Milford E, Owen W, Star R, Toto R, Eknoyan G. Hemodialysis Study Group. Dialysis dose and the effect of gender and body size on outcome in the HEMO Study. Kidney Int. 2004; 65:1386–1394.
Article10. Termorshuizen F, Dekker FW, van Manen JG, Korevaar JC, Boeschoten EW, Krediet RT. NECOSAD Study Group. Relative contribution of residual renal function and different measures of adequacy to survival in hemodialysis patients: an analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD)-2. J Am Soc Nephrol. 2004; 15:1061–1070.
Article11. Port FK, Wolfe RA, Hulbert-Shearon TE, McCullough KP, Ashby VB, Held PJ. High dialysis dose is associated with lower mortality among women but not among men. Am J Kidney Dis. 2004; 43:1014–1023.
Article12. Lowrie EG, Laird NM, Parker TF, Sargent JA. Effect of the hemodialysis prescription of patient morbidity: report from the National Cooperative Dialysis Study. N Engl J Med. 1981; 305:1176–1181.
Article13. Gotch FA, Sargent JA. A mechanistic analysis of the National Cooperative Dialysis Study (NCDS). Kidney Int. 1985; 28:526–534.
Article14. Hemodialysis Adequacy 2006 Work Group. Clinical practice guidelines for hemodialysis adequacy, update 2006. Am J Kidney Dis. 2006; 48:Suppl 1. S2–S90.15. Oh JS, Kim SM, Sin YH, Kim JK, Son YK, An WS, Kim SE, Kim KH. Reliability of hemodialysis adequacy measured by ionic dialysance. Korean J Nephrol. 2011; 30:278–284.16. Locatelli F, Canaud B. Dialysis adequacy today: a European perspective. Nephrol Dial Transplant. 2012; 27:3043–3048.
Article17. Canada-USA (CANUSA) Peritoneal Dialysis Study Group. Adequacy of dialysis and nutrition in continuous peritoneal dialysis: association with clinical outcomes. J Am Soc Nephrol. 1996; 7:198–207.18. Paniagua R, Amato D, Vonesh E, Correa-Rotter R, Ramos A, Moran J, Mujais S. Mexican Nephrology Collaborative Study Group. Effects of increased peritoneal clearances on mortality rates in peritoneal dialysis: ADEMEX, a prospective, randomized, controlled trial. J Am Soc Nephrol. 2002; 13:1307–1320.
Article19. Lo WK, Ho YW, Li CS, Wong KS, Chan TM, Yu AW, Ng FS, Cheng IK. Effect of Kt/V on survival and clinical outcome in CAPD patients in a randomized prospective study. Kidney Int. 2003; 64:649–656.
Article20. Park HC, Kang SW, Choi KH, Ha SK, Han DS, Lee HY. Clinical outcome in continuous ambulatory peritoneal dialysis patients is not influenced by high peritoneal transport status. Perit Dial Int. 2001; 21:Suppl 3. S80–S85.
Article21. Bargman JM, Thorpe KE, Churchill DN. CANUSA Peritoneal Dialysis Study Group. Relative contribution of residual renal function and peritoneal clearance to adequacy of dialysis: a reanalysis of the CANUSA study. J Am Soc Nephrol. 2001; 12:2158–2162.
Article22. Dombros N, Dratwa M, Feriani M, Gokal R, Heimbürger O, Krediet R, Plum J, Rodrigues A, Selgas R, Struijk D, Verger C. EBPG Expert Group on Peritoneal Dialysis. European best practice guidelines for peritoneal dialysis. 7 Adequacy of peritoneal dialysis. Nephrol Dial Transplant. 2005; 20:Suppl 9. ix24–ix27.23. Clinical practice recommendations for peritoneal dialysis adequacy. Am J Kidney Dis. 2006; 48:Suppl 1. S130–S158.24. Termorshuizen F, Korevaar JC, Dekker FW, van Manen JG, Boeschoten EW, Krediet RT. NECOSAD Study Group. The relative importance of residual renal function compared with peritoneal clearance for patient survival and quality of life: an analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD )-2. Am J Kidney Dis. 2003; 41:1293–1302.
Article25. Kim SG, Kim NH. The effect of residual renal function at the initiation of dialysis on patient survival. Korean J Intern Med. 2009; 24:55–62.
Article26. Medcalf JF, Harris KP, Walls J. Role of diuretics in the preservation of residual renal function in patients on continuous ambulatory peritoneal dialysis. Kidney Int. 2001; 59:1128–1133.
Article27. Suzuki H, Kanno Y, Sugahara S, Okada H, Nakamoto H. Effects of an angiotensin II receptor blocker, valsartan, on residual renal function in patients on CAPD. Am J Kidney Dis. 2004; 43:1056–1064.
Article28. Goldberg R, Yalavarthy R, Teitelbaum I. Adequacy of peritoneal dialysis: beyond small solute clearance. Contrib Nephrol. 2009; 163:147–154.
Article29. Lo WK, Bargman JM, Burkart J, Krediet RT, Pollock C, Kawanishi H, Blake PG. ISPD Adequacy of Peritoneal Dialysis Working Group. Guideline on targets for solute and fluid removal in adult patients on chronic peritoneal dialysis. Perit Dial Int. 2006; 26:520–522.
Article30. Ates K, Nergizoglu G, Keven K, Sen A, Kutlay S, Erturk S, Duman N, Karatan O, Ertug AE. Effect of fluid and sodium removal on mortality in peritoneal dialysis patients. Kidney Int. 2001; 60:767–776.
Article31. Brown EA, Davies SJ, Rutherford P, Meeus F, Borras M, Riegel W, Divino Filho JC, Vonesh E, van Bree M. EAPOS Group. Survival of functionally anuric patients on automated peritoneal dialysis: the European APD Outcome Study. J Am Soc Nephrol. 2003; 14:2948–2957.
Article32. Charra B, Laurent G, Chazot C, Calemard E, Terrat JC, Vanel T, Jean G, Ruffet M. Clinical assessment of dry weight. Nephrol Dial Transplant. 1996; 11:Suppl 2. 16–19.
Article33. Rocco MV, Yan G, Heyka RJ, Benz R, Cheung AK. HEMO Study Group. Risk factors for hypertension in chronic hemodialysis patients: baseline data from the HEMO study. Am J Nephrol. 2001; 21:280–288.
Article34. Eloot S, Van Biesen W, Vanholder R. A sad but forgotten truth: the story of slow-moving solutes in fast hemodialysis. Semin Dial. 2012; 25:505–509.
Article35. Locatelli F, Martin-Malo A, Hannedouche T, Loureiro A, Papadimitriou M, Wizemann V, Jacobson SH, Czekalski S, Ronco C, Vanholder R. Membrane Permeability Outcome (MPO) Study Group. Effect of membrane permeability on survival of hemodialysis patients. J Am Soc Nephrol. 2009; 20:645–654.
Article36. Park JS, Kim GH, Kang CM, Lee CH. Application of cystatin C reduction ratio to high-flux hemodialysis as an alternative indicator of the clearance of middle molecules. Korean J Intern Med. 2010; 25:77–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationships among Handgrip Strength, Blood Pressure, Dialysis Adequacy, Dialysis Symptoms, and Depression in Hemodialysis Patients
- Association between Dialysis Adequacy and Cognition in Patients with Peritoneal Dialysis
- Peritoneal dialysis in children and adolescents
- Relatioship between Dialysis Adequacy and Anemia in Patients with Hemodialysis
- The Effect of Increasing Blood Flow Rate on Dialysis Adequacy in Hemodialysis Patients with Low Kt/V