Diabetes Metab J.
2015 Oct;39(5):395-404. 10.4093/dmj.2015.39.5.395.
The Association between Hypertension Comorbidity and Microvascular Complications in Type 2 Diabetes Patients: A Nationwide Cross-Sectional Study in Thailand
- Affiliations
-
- 1Faculty of Public Health, Khon Kaen University, Khon Kaen, Thailand. cphurst@gmail.com
- 2Clinical Epidemiology Unit, Khon Kaen University Faculty of Medicine, Khon Kaen, Thailand.
- 3Faculty of Public Health, Thai Nguyen University of Medicine and Pharmacy, Thai Nguyen, Vietnam.
- KMID: 2174013
- DOI: http://doi.org/10.4093/dmj.2015.39.5.395
Abstract
- BACKGROUND
Type 2 diabetes mellitus (T2DM) is a global pandemic and its prevalence is rapidly increasing in developing countries, including Thailand. The most common comorbidity of T2DM is hypertension. T2DM with a hypertension comorbidity is likely to exacerbate the development of, or more severe microvascular complications. This study aims to determine the association between the hypertension comorbidity and microvascular complication among T2DM patients in Thailand.
METHODS
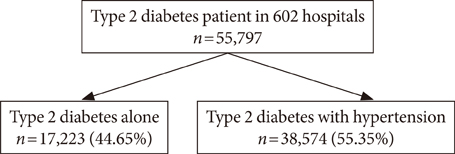
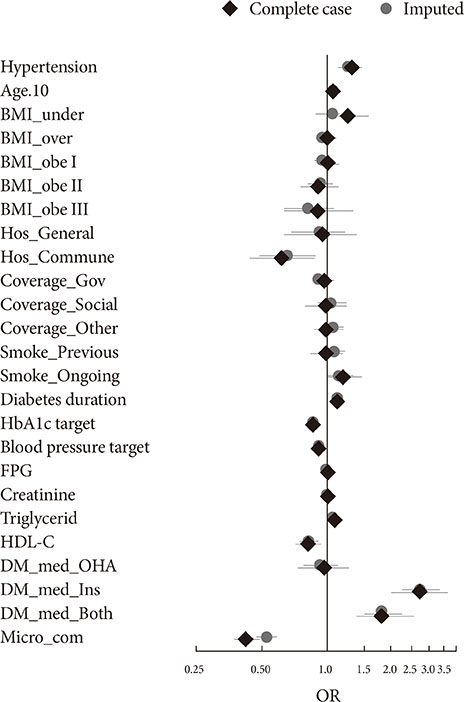
The present study is a nationwide, multicenter, cross-sectional survey of T2DM outpatients across Thailand. Binary logistic mixed effect regression was used to investigate the effect of hypertension and other risk factors on the presence of microvascular complications. Imputation was used to investigate potential bias introduced by missing values.
RESULTS
Of the 55,797 T2DM patients included in our sample, 55.35% were hypertensive. Prevalence of microvascular complication diagnosis in the last 12 months was higher in T2DM patients with hypertension than those without hypertension (12.12% vs. 9.80%, respectively). Patient with a hypertension comorbidity had 1.32 time the odds of developing microvascular complication (adjusted odds ratio [OR], 1.32; 95% confidence interval [CI], 1.20 to 1.46; P<0.001). Older age, longer diabetes duration had 1.07 and 1.21 times the odds of developing microvascular complication, per 10 years (age) and 5 years (duration), respectively (OR(age), 1.07; 95% CI, 1.03 to 1.12; P<0.001; and OR(duration), 1.12; 95% CI, 1.07 to 1.16; P<0.001; respectively). Minimal bias was introduced by missing values, and did not influence to the magnitude of effect of hypertension on the presence microvascular complication.
CONCLUSION
Hypertension comorbidity is highly associated with microvascular complication among T2DM patients. Patients with T2DM and physicians should pay attention to blood pressure control.
MeSH Terms
Figure
Cited by 1 articles
-
Association of Combined
TCF7L2 andKCNQ1 Gene Polymorphisms with Diabetic Micro- and Macrovascular Complications in Type 2 Diabetes Mellitus
Rujikorn Rattanatham, Nongnuch Settasatian, Nantarat Komanasin, Upa Kukongviriyapan, Kittisak Sawanyawisuth, Phongsak Intharaphet, Vichai Senthong, Chatri Settasatian
Diabetes Metab J. 2021;45(4):578-593. doi: 10.4093/dmj.2020.0101.
Reference
-
1. Zimmet P. The burden of type 2 diabetes: are we doing enough? Diabetes Metab. 2003; 29(4 Pt 2):6S9–618.2. Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001; 414:782–787.3. Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014; 103:137–149.4. Holt RI. Chapter 36, Pathogenesis of microvascular complications. Textbook of diabetes. 4th ed. Chichester: Wiley-Blackwell;2010. p. 553–574.5. Del Canizo Gomez FJ, Fernandez Perez C, Moreno Ruiz I, de Gorospe Perez-Jauregui C, Silveira Rodriguez B, Gonzalez Losada T, Segura Galindo A. Microvascular complications and risk factors in patients with type 2 diabetes. Endocrinol Nutr. 2011; 58:163–168.6. Raman R, Gupta A, Krishna S, Kulothungan V, Sharma T. Prevalence and risk factors for diabetic microvascular complications in newly diagnosed type II diabetes mellitus. Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetic Study (SN-DREAMS, report 27). J Diabetes Complications. 2012; 26:123–128.7. Amini M, Parvaresh E. Prevalence of macro- and microvascular complications among patients with type 2 diabetes in Iran: a systematic review. Diabetes Res Clin Pract. 2009; 83:18–25.8. Leelawattana R, Pratipanawatr T, Bunnag P, Kosachunhanun N, Suwanwalaikorn S, Krittiyawong S, Chetthakul T, Plengvidhya N, Benjasuratwong Y, Deerochanawong C, Mongkolsomlit S, Ngarmukos C, Rawdaree P. Thailand diabetes registry project: prevalence of vascular complications in long-standing type 2 diabetes. J Med Assoc Thai. 2006; 89:Suppl 1. S54–S59.9. Liu Z, Fu C, Wang W, Xu B. Prevalence of chronic complications of type 2 diabetes mellitus in outpatients: a cross-sectional hospital based survey in urban China. Health Qual Life Outcomes. 2010; 8:62.10. Tapp RJ, Shaw JE, Harper CA, de Courten MP, Balkau B, McCarty DJ, Taylor HR, Welborn TA, Zimmet PZ. AusDiab Study Group. The prevalence of and factors associated with diabetic retinopathy in the Australian population. Diabetes Care. 2003; 26:1731–1737.11. Campbell RK. Type 2 diabetes: where we are today: an overview of disease burden, current treatments, and treatment strategies. J Am Pharm Assoc (2003). 2009; 49:Suppl 1. S3–S9.12. Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. 2010; 87:302–312.13. Hussain A, Hydrie MZ, Clausen B, Asphar S. Type 2 diabetes and obesity: a review. J Diabetol. 2010; 2:1.14. Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in southeast asian and african regions: need for effective strategies for prevention and control in primary health care settings. Int J Hypertens. 2013; 2013:409083.15. Lastra G, Syed S, Kurukulasuriya LR, Manrique C, Sowers JR. Type 2 diabetes mellitus and hypertension: an update. Endocrinol Metab Clin North Am. 2014; 43:103–122.16. Shera AS, Jawad F, Maqsood A, Jamal S, Azfar M, Ahmed U. Prevalence of chronic complications and associated factors in type 2 diabetes. J Pak Med Assoc. 2004; 54:54–59.17. Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, Wright AD, Turner RC, Holman RR. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000; 321:412–419.18. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998; 317:703–713.19. Rawdaree P, Ngarmukos C, Deerochanawong C, Suwanwalaikorn S, Chetthakul T, Krittiyawong S, Benjasuratwong Y, Bunnag P, Kosachunhanun N, Plengvidhya N, Leelawatana R, Prathipanawatr T, Likitmaskul S, Mongkolsomlit S. Thailand diabetes registry (TDR) project: clinical status and long term vascular complications in diabetic patients. J Med Assoc Thai. 2006; 89:Suppl 1. S1–S9.20. DAMUS Central (Data Archival for Maximum Utilization System): sharing raw data of research projects. cited 2015 Jul 7. Available from: http://www.damus.in.th/damus/index.php.21. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289:2560–2572.22. American Diabetes Association. Standards of medical care in diabetes: 2012. Diabetes Care. 2012; 35:Suppl 1. S11–S63.23. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.24. Meng XL, Rubin DB. Performing likelihood ratio tests with multiply-imputed data sets. Biometrika. 1992; 79:103–111.25. Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008; 3:17.26. R Core Team. R: a language and environment for statistical computing. 3.0.2013-05-12 ed. Vienna: R Foundation for Statistical Computing;2013.27. Bates D, Maechler M, Bolker B, Walker S. lme4: Linear mixed-effects models using Eigen and S4. R package version 1.0-6. Vienna: R Foundation;2014.28. Su YS, Gelman A, Hill J, Yajima M. Multiple imputation with diagnostics (mi) in R: opening windows into the black box. J Stat Softw. 2011; 45:1–31.29. Aekplakorn W, Stolk RP, Neal B, Suriyawongpaisal P, Chongsuvivatwong V, Cheepudomwit S, Woodward M. INTERASIA Collaborative Group. The prevalence and management of diabetes in Thai adults: the international collaborative study of cardiovascular disease in Asia. Diabetes Care. 2003; 26:2758–2763.30. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006; 368:1681–1688.31. Cardoso CR, Salles GF. Predictors of development and progression of microvascular complications in a cohort of Brazilian type 2 diabetic patients. J Diabetes Complications. 2008; 22:164–170.32. American Diabetes Association. Standards of medical care in diabetes: 2010. Diabetes Care. 2010; 33:Suppl 1. S11–S61.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Frequencies and Risk Factors for Microvascular Complications in Patients with Type 1 Diabetes Mellitus
- Hyperfibrinogenemia as an Important Risk Factor for Microvascular Complications in NIDDM Patients
- Associations between diabetes self-management and microvascular complications in patients with type 2 diabetes
- The Association between Serum Uric Acid and Peripheral Neuropathy in Patients with Type 2 Diabetes Mellitus: A Multicenter Nationwide CrossSectional Study
- Effects of circadian blood pressure patterns on development of microvascular complications in pediatric patients with type 1 diabetes mellitus