Ann Dermatol.
2010 Feb;22(1):73-76. 10.5021/ad.2010.22.1.73.
Oral Hairy Leukoplakia Which Occurred as a Presenting Sign of Acute Myeloid Leukemia in a Child
- Affiliations
-
- 1Department of Dermatology, School of Medicine, Pusan National University, Busan, Korea. drkmp@hanmail.net
- KMID: 2172044
- DOI: http://doi.org/10.5021/ad.2010.22.1.73
Abstract
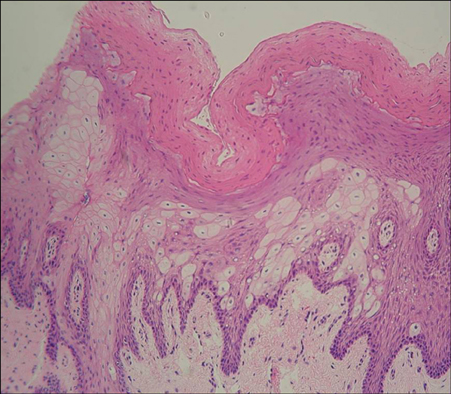
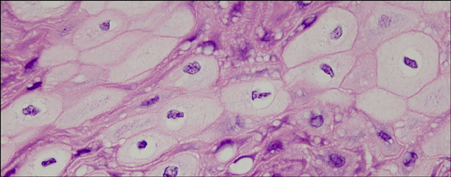
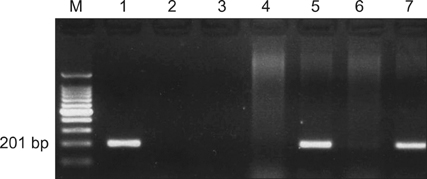
- Oral hairy leukoplakia (OHL) is caused by the reactivation of a previous Epstein-Barr virus (EBV) infection in the epithelium of the tongue. Most lesions are characterized by corrugated whitish patches on the lateral border of the tongue. It is frequently associated with AIDS, but cases in patients with other immunosuppressed states have also been reported. In leukemia patients, OHL is rarely encountered, and appears only after chemotherapy. We report a case of OHL which occurred as a presenting sign of acute myeloid leukemia (AML) in a previously healthy 15-year-old child. A 15-year-old boy presented with a whitish patch on the left lateral border of the tongue. The biopsy specimen revealed papillomatosis, hyperkeratosis, acanthosis and ballooning degeneration in the stratum spinosum. The patient was EBV seropositive, and PCR analysis of EBV DNA in the lesional tissue was positive. After the diagnosis of OHL in dermatologic department, the patient was referred to pediatrics due to the abnormal peripheral blood smear, and was diagnosed with AML.
MeSH Terms
Figure
Reference
-
1. Greenspan D, Greenspan JS, Conant M, Petersen V, Silverman S Jr, de Souza Y. Oral "hairy" leucoplakia in male homosexuals: evidence of association with both papillomavirus and a herpes-group virus. Lancet. 1984. 2:831–834.2. Woo SB. McKee PH, Calonje E, Granter S, editors. Diseases of the oral mucosa. Pathology of the skin: with clinical correlations. 2005. 3rd ed. Philadelphia: Elsevier Mosby;430–431.
Article3. Mabruk MJ, Flint SR, Toner M, Balluz I, Coleman D, Sullivan D, et al. In situ hybridization and the polymerase chain reaction (PCR) in the analysis of biopsies and exfoliative cytology specimens for definitive diagnosis of oral hairy leukoplakia (OHL). J Oral Pathol Med. 1994. 23:302–308.
Article4. Alessi E, Berti E, Cusini M, Zerboni R, Cavicchini S, Tomasini D, et al. Oral hairy leukoplakia. J Am Acad Dermatol. 1990. 22:79–86.
Article5. Syrjanen S, Laine P, Niemela M, Happonen RP. Oral hairy leukoplakia is not a specific sign of HIV-infection but related to immunosuppression in general. J Oral Pathol Med. 1989. 18:28–31.
Article6. Schiodt M, Norgaard T, Greenspan JS. Oral hairy leukoplakia in an HIV-negative woman with Behcet's syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995. 79:53–56.7. Markowski TR, Martin DB, Kao GF, Lutz L, Deng A, Gaspari AA. Leukemia cutis: a presenting sign in acute promyelocytic leukemia. Arch Dermatol. 2007. 143:1220–1221.
Article8. Fox LP, Geyer AS, Husain S, Grossman ME. Bullous pyoderma gangrenosum as the presenting sign of fatal acute myelogenous leukemia. Leuk Lymphoma. 2006. 47:147–150.
Article9. Sullivan R, Clowers-Webb H, Davis MD. Erythema nodosum: a presenting sign of acute myelogenous leukemia. Cutis. 2005. 76:114–116.10. Callen JP, Bernardi DM, Clark RA, Weber DA. Adult-onset recalcitrant eczema: a marker of noncutaneous lymphoma or leukemia. J Am Acad Dermatol. 2000. 43:207–210.
Article11. Clore LS Jr, Stafford CT. Chronic urticaria as a presenting sign of hairy cell leukemia. Allergy Asthma Proc. 1999. 20:51–55.
Article12. Sumner WT, Grichnik JM, Shea CR, Moore JO, Miller WS, Burton CS. Follicular mucinosis as a presenting sign of acute myeloblastic leukemia. J Am Acad Dermatol. 1998. 38:803–805.
Article13. Young LS, Clark D, Sixbey JW, Rickinson AB. Epstein-Barr virus receptors on human pharyngeal epithelia. Lancet. 1986. 1:240–242.
Article14. Lozada-Nur F, Robinson J, Regezi JA. Oral hairy leukoplakia in nonimmunosuppressed patients. Report of four cases. Oral Surg Oral Med Oral Pathol. 1994. 78:599–602.15. Lee KH, Polonowita AD. Oral hairy leukoplakia arising in an oral lichen planus lesion in an otherwise immune-competent patient. N Z Dent J. 2007. 103:58–59.16. Nicolatou O, Nikolatos G, Fisfis M, Belegrati M, Papadaki T, Oikonomaki E, et al. Oral hairy leukoplakia in a patient with acute lymphocytic leukemia. Oral Dis. 1999. 5:76–79.
Article17. Greenspan D, Greenspan JS, de Souza Y, Levy JA, Ungar AM. Oral hairy leukoplakia in an HIV-negative renal transplant recipient. J Oral Pathol Med. 1989. 18:32–34.
Article18. Pan L, Milligan L, Michaeli J, Cesarman E, Knowles DM. Polymerase chain reaction detection of Kaposi's sarcoma-associated herpesvirus-optimized protocols and their application to myeloma. J Mol Diagn. 2001. 3:32–38.
Article19. Moura MD, Guimaraes TR, Fonseca LM, de Almeida Pordeus I, Mesquita RA. A random clinical trial study to assess the efficiency of topical applications of podophyllin resin (25%) versus podophyllin resin (25%) together with acyclovir cream (5%) in the treatment of oral hairy leukoplakia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. 103:64–71.
Article20. Bhandarkar SS, MacKelfresh J, Fried L, Arbiser JL. Targeted therapy of oral hairy leukoplakia with gentian violet. J Am Acad Dermatol. 2008. 58:711–712.
Article21. Pastore L, De Benedittis M, Petruzzi M, Fiore JR, Serpico R. Efficacy of famciclovir in the treatment of oral hairy leukoplakia. Br J Dermatol. 2006. 154:378–379.
Article22. Greenspan D, Greenspan JS, Hearst NG, Pan LZ, Conant MA, Abrams DI, et al. Relation of oral hairy leukoplakia to infection with the human immunodeficiency virus and the risk of developing AIDS. J Infect Dis. 1987. 155:475–481.
Article23. Nokta M. Oral manifestations associated with HIV infection. Curr HIV/AIDS Rep. 2008. 5:5–12.
Article24. Gennaro S, Naidoo S, Berthold P. Oral health & HIV/AIDS. MCN Am J Matern Child Nurs. 2008. 33:50–57.25. Blomgren J, Back H. Oral hairy leukoplakia in a patient with multiple myeloma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996. 82:408–410.
Article26. Jaff N, Chelghoum Y, Elhamri M, Tigaud I, Michallet M, Thomas X. Trisomy 8 as sole anomaly or with other clonal aberrations in acute myeloid leukemia: impact on clinical presentation and outcome. Leuk Res. 2007. 31:67–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Secondary Syphilis Presenting as a "Leukoplakia-like" Plaque on the Tongue in a HIV Patient
- Acute Myeloid Leukemia with Intracardiac Thrombus Presenting as Acute Limb Ischemia
- A Case of Leukemia Cutis in Myelodysplastic Syndrome Evolving into An Atypical Chronic Myeloid Leukemia
- Facial palsy as the presenting symptom of acute myeloid leukemia in children: Three cases with stem cell transplantations
- Sweet's Syndrome with Myelodysplastic Syndrome Progressing to Acute Myelogenous Leukemia