Cancer Res Treat.
2014 Apr;46(2):194-199.
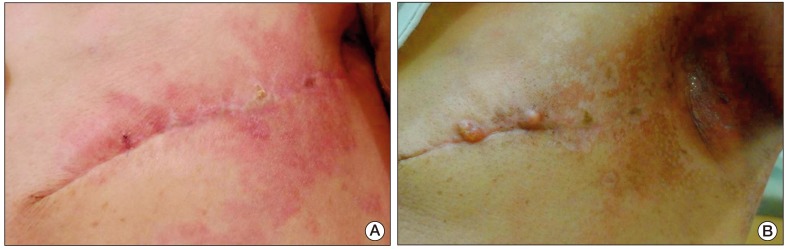
Case Series of Different Onset of Skin Metastasis According to the Breast Cancer Subtypes
- Affiliations
-
- 1Division of Medical Oncology, Department of Internal Medicine, Incheon Sarang Hospital, Incheon, Korea.
- 2Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. socmed0127@gmail.com
Abstract
- We report on five cases of skin metastasis according to the breast cancer (BC) subtype. Two cases of HER2 positive BC showed only skin metastasis after immediate postoperative period and rapid clinical response to targeted therapy. Another two cases of triple negative BC showed thyroid and lung metastasis in addition to skin metastasis, and their response of cytotoxic chemotherapy was not definite. The other hormone positive BC showed skin metastasis only, with a longer, slower, less progressive pattern than other subtypes. Most cases of skin metastasis were detected at terminal stage of malignancy and were considered to have a limited survival period. However, some BC patients can survive longer if the targeted agents are effective. Therefore, physicians should provide detailed follow up of BC after curative treatment and understand the metastatic pattern of BC according to the subtype.
Keyword
MeSH Terms
Figure
Reference
-
1. Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, Anderson K, et al. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res. 2005; 11:5678–5685. PMID: 16115903.
Article2. Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, et al. Molecular portraits of human breast tumours. Nature. 2000; 406:747–752. PMID: 10963602.
Article3. Sørlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci U S A. 2001; 98:10869–10874. PMID: 11553815.4. Sørlie T, Wang Y, Xiao C, Johnsen H, Naume B, Samaha RR, et al. Distinct molecular mechanisms underlying clinically relevant subtypes of breast cancer: gene expression analyses across three different platforms. BMC Genomics. 2006; 7:127. PMID: 16729877.
Article5. Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci U S A. 2003; 100:8418–8423. PMID: 12829800.6. Sotiriou C, Neo SY, McShane LM, Korn EL, Long PM, Jazaeri A, et al. Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc Natl Acad Sci U S A. 2003; 100:10393–10398. PMID: 12917485.
Article7. Lookingbill DP, Spangler N, Helm KF. Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patients. J Am Acad Dermatol. 1993; 29(2 Pt 1):228–236. PMID: 8335743.
Article8. Braverman IM. Skin manifestations of internal malignancy. Clin Geriatr Med. 2002; 18:1–19. PMID: 11913734.
Article9. Nanda R. "Targeting" triple-negative breast cancer: the lessons learned from BRCA1-associated breast cancers. Semin Oncol. 2011; 38:254–262. PMID: 21421115.
Article10. Kong JH, Park YH, Kim JA, Kim JH, Yun J, Sun JM, et al. Patterns of skin and soft tissue metastases from breast cancer according to subtypes: relationship between EGFR overexpression and skin manifestations. Oncology. 2011; 81:55–62. PMID: 21934337.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Alopecia Neoplastica Metastasis from Breast Carcinoma
- Mouse models of breast cancer in preclinical research
- Two Cases of Cutaneous Metastasis from Small Cell Lung Cancer
- Treatment Approach for Rare Histologic Subtypes of Breast Cancer: A Review
- An Unusual Case of Gastric Cancer Presenting with Breast Metastasis with Pleomorphic Microcalcifications