Ann Surg Treat Res.
2014 Apr;86(4):184-191. 10.4174/astr.2014.86.4.184.
Outcomes of living donor liver transplantation using elderly donors
- Affiliations
-
- 1Department of Surgery, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. yky602@catholic.ac.kr
- KMID: 2167124
- DOI: http://doi.org/10.4174/astr.2014.86.4.184
Abstract
- PURPOSE
Living donor liver transplantation (LDLT) using elderly donors is increasing in frequency in response to organ shortage. However, elderly donor graft has been reported to negatively affect graft patency and patient survival.
METHODS
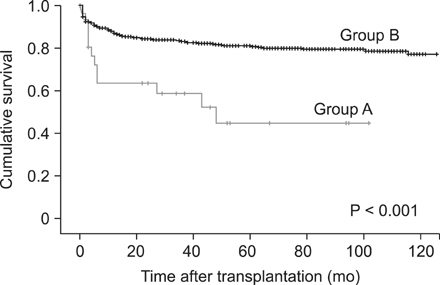
We retrospectively reviewed the medical records of 604 patients who underwent LDLT at Seoul St. Mary's Hospital, The Catholic University of Korea between May 1999 and September 2012. Elderly donors were defined as those > or =55 years of age. Here, we evaluate the survival differences and causes of death of recipients of elderly donor grafts.
RESULTS
The overall mortality rate of the recipients was significantly higher in the elderly donor group (group A) than in the younger donor group (group B: 46.2% vs. 18.1%, P = 0.004). The survival length of group A was significantly shorter than that of group B (31.2 +/- 31.3 and 51.4 +/- 40.8 months, P = 0.014). The significantly common causes of death in group A were biliary (41.7%) and arterial complication (16.7%), and it was higher than those in group B (P = 0.000 and P = 0.043, respectively).
CONCLUSION
LDLT using elderly donors could induce more serious complications and higher mortality rates than those at using younger donors. As such, careful donor selection is needed, especially with regard to assessing the condition of potential elderly donor livers. Furthermore, a large-volume and multicenter study of complications and outcomes of LDLT using elderly donor liver is required.
Keyword
MeSH Terms
Figure
Reference
-
1. Nadig SN, Bratton CF, Karp SJ. Marginal donors in liver transplantation: expanding the donor pool. J Surg Educ. 2007; 64:46–50.2. Montalti R, Nardo B, Bertelli R, Beltempo P, Puviani L, Vivarelli M, et al. Donor pool expansion in liver transplantation. Transplant Proc. 2004; 36:520–522.3. Li C, Wen TF, Yan LN, Li B, Yang JY, Xu MQ, et al. Safety of living donor liver transplantation using older donors. J Surg Res. 2012; 178:982–987.4. Yoshizumi T, Shirabe K, Soejima Y, Taketomi A, Yamashita N, Ikegami T, et al. Living donor liver transplantation in patients older than 60 years. Transplantation. 2010; 90:433–437.5. Keswani RN, Ahmed A, Keeffe EB. Older age and liver transplantation: a review. Liver Transpl. 2004; 10:957–967.6. Serrano MT, Garcia-Gil A, Arenas J, Ber Y, Cortes L, Valiente C, et al. Outcome of liver transplantation using donors older than 60 years of age. Clin Transplant. 2010; 24:543–549.7. Cescon M, Zanello M, Grazi GL, Cucchetti A, Ravaioli M, Ercolani G, et al. Impact of very advanced donor age on hepatic artery thrombosis after liver transplantation. Transplantation. 2011; 92:439–445.8. Stewart ZA, Locke JE, Segev DL, Dagher NN, Singer AL, Montgomery RA, et al. Increased risk of graft loss from hepatic artery thrombosis after liver transplantation with older donors. Liver Transpl. 2009; 15:1688–1695.9. Yersiz H, Shaked A, Olthoff K, Imagawa D, Shackleton C, Martin P, et al. Correlation between donor age and the pattern of liver graft recovery after transplantation. Transplantation. 1995; 60:790–794.10. Woodhouse KW, Wynne HA. Age-related changes in liver size and hepatic blood flow. The influence on drug metabolism in the elderly. Clin Pharmacokinet. 1988; 15:287–294.11. Schmucker DL. Liver function and phase I drug metabolism in the elderly: a paradox. Drugs Aging. 2001; 18:837–851.12. Deschênes M, Forbes C, Tchervenkov J, Barkun J, Metrakos P, Tector J, et al. Use of older donor livers is associated with more extensive ischemic damage on intraoperative biopsies during liver transplantation. Liver Transpl Surg. 1999; 5:357–361.13. Ikegami T, Nishizaki T, Yanaga K, Shimada M, Kishikawa K, Nomoto K, et al. The impact of donor age on living donor liver transplantation. Transplantation. 2000; 70:1703–1707.14. Grazi GL, Ravaioli M, Zanello M, Ercolani G, Cescon M, Varotti G, et al. Using elderly donors in liver transplantation. Transplant Proc. 2005; 37:2582–2583.15. Kuramitsu K, Egawa H, Keeffe EB, Kasahara M, Ito T, Sakamoto S, et al. Impact of age older than 60 years in living donor liver transplantation. Transplantation. 2007; 84:166–172.16. Santori G, Andorno E, Morelli N, Bottino G, Mondello R, Gianelli Castiglione A, et al. Impact of different cadaveric donor age cut-offs on adult recipient survival after liver transplantation: a single-center analysis. Transplant Proc. 2005; 37:2576–2581.17. Hesse UJ, Berrevoet F, Pattyn P, de Hemptinne B. Results of liver transplantation in elderly patients (> 55 years of age). Langenbecks Arch Chir Suppl Kongressbd. 1996; 113:419–421.18. Adam R, Karam V, Delvart V, O'Grady J, Mirza D, Klempnauer J, et al. Evolution of indications and results of liver transplantation in Europe: a report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012; 57:675–688.19. Kim do Y, Choi MS, Lee JH, Koh KC, Paik SW, Yoo BC, et al. Older donor allografts are associated with poor patient survival after living donor liver transplantation for hepatitis B virus-related liver diseases. Liver Int. 2007; 27:260–267.20. Mutimer DJ, Gunson B, Chen J, Berenguer J, Neuhaus P, Castaing D, et al. Impact of donor age and year of transplantation on graft and patient survival following liver transplantation for hepatitis C virus. Transplantation. 2006; 81:7–14.21. Cassuto JR, Patel SA, Tsoulfas G, Orloff MS, Abt PL. The cumulative effects of cold ischemic time and older donor age on liver graft survival. J Surg Res. 2008; 148:38–44.22. Shah SA, Levy GA, Greig PD, Smith R, McGilvray ID, Lilly LB, et al. Reduced mortality with right-lobe living donor compared to deceased-donor liver transplantation when analyzed from the time of listing. Am J Transplant. 2007; 7:998–1002.23. Mizuno S, Yokoi H, Shiraki K, Usui M, Sakurai H, Tabata M, et al. Prospective study on the outcome of patients with hepatocellular carcinoma registered for living donor liver transplantation: how long can they wait? Transplantation. 2010; 89:650–654.24. Kasahara M, Egawa H, Tanaka K, Ogawa K, Uryuhara K, Fujimoto Y, et al. Variations in biliary anatomy associated with trifurcated portal vein in right-lobe living-donor liver transplantation. Transplantation. 2005; 79:626–627.25. Radtke A, Sgourakis G, Sotiropoulos GC, Molmenti EP, Nadalin S, Schroeder T, et al. Vascular and biliary anatomy of the right hilar window: its impact on recipient morbidity and mortality for right graft live donor liver transplantation. World J Surg. 2009; 33:1941–1951.26. Boin IF, Ataide EC, Leonardi MI, Stucchi R, Seva-Pereira T, Pereira IW, et al. Elderly donors for HCV(+) versus non-HCV recipients: patient survival following liver transplantation. Transplant Proc. 2008; 40:792–796.27. Lake JR. Should liver transplantation be performed for patients with chronic hepatitis B? Yes! Liver Transpl Surg. 1995; 1:260–265.28. Ono Y, Kawachi S, Hayashida T, Wakui M, Tanabe M, Itano O, et al. The influence of donor age on liver regeneration and hepatic progenitor cell populations. Surgery. 2011; 150:154–161.29. Duailibi DF, Ribeiro MA Jr. Biliary complications following deceased and living donor liver transplantation: a review. Transplant Proc. 2010; 42:517–520.30. Takatsuki M, Eguchi S, Kawashita Y, Kanematsu T. Biliary complications in recipients of living-donor liver transplantation. J Hepatobiliary Pancreat Surg. 2006; 13:497–501.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver retransplantation for adult recipients
- Endoscopic management of anastomotic stricture after living-donor liver transplantation
- Decreasing the operation time of living donor liver transplantation in the era of laparoscopic living donor hepatectomy
- Pediatric liver transplantation in Korea: long-term outcomes and allocations
- A Single Center Experience for a Feasibility of Totally Laparoscopic Living Donor Right Hepatectomy