Ann Rehabil Med.
2015 Jun;39(3):432-439. 10.5535/arm.2015.39.3.432.
Effect of Repetitive Transcranial Magnetic Stimulation According to the Stimulation Site in Stroke Patients With Dysphagia
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation and Regional Cardiocerebrovascular Center, Dong-A University College of Medicine, Busan, Korea. bobo-0416@hanmail.net
- KMID: 2165647
- DOI: http://doi.org/10.5535/arm.2015.39.3.432
Abstract
OBJECTIVE
To investigate the effect of repetitive transcranial magnetic stimulation (rTMS) according to the stimulation site in subacute stroke patients with dysphagia.
METHODS
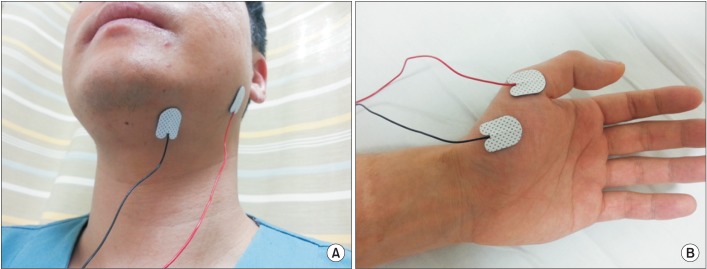
This study was designed as a matched comparative study. Twenty-four patients who had dysphagia after ischemic stroke were recruited, and they were divided into two groups after matching for age and stroke lesion. The patients in group A received rTMS over the brain cortex where motor evoked potential (MEP) was obtained from the suprahyoid muscle. Group B received rTMS over the brain cortex where MEP was obtained from the abductor pollicis brevis muscle. rTMS was performed at 110% of MEP threshold, 10 Hz frequency for 10 seconds, and then repeated every minute for 10 minutes. Dysphagia status was measured by the Functional Dysphagia Scale (FDS), the Penetration-Aspiration Scale (PAS), and the Dysphagia Outcome and Severity Scale (DOSS) using the results of a videofluoroscopic swallowing study. These evaluations were measured before, immediately, and 4 weeks after rTMS.
RESULTS
Group A showed significant improvement compared to group B in the DOSS score immediately and 4 weeks after rTMS. There were no significant differences in the changes of FDS and PAS scores between groups A and B immediately and 4 weeks after rTMS.
CONCLUSION
rTMS over a hot spot for the suprahyoid muscle caused more improvement in swallowing function when compared to that over the interconnected site.
MeSH Terms
Figure
Reference
-
1. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.2. Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW. Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil. 1995; 76:310–316. PMID: 7717830.
Article3. Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. Br Med J (Clin Res Ed). 1987; 295:411–414.
Article4. Kidd D, Lawson J, Nesbitt R, MacMahon J. The natural history and clinical consequences of aspiration in acute stroke. QJM. 1995; 88:409–413. PMID: 7648232.5. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996; 27:1200–1204. PMID: 8685928.6. Sharma JC, Fletcher S, Vassallo M, Ross I. What influences outcome of stroke: pyrexia or dysphagia? Int J Clin Pract. 2001; 55:17–20. PMID: 11219313.7. Hamdy S, Rothwell JC, Aziz Q, Thompson DG. Organization and reorganization of human swallowing motor cortex: implications for recovery after stroke. Clin Sci (Lond). 2000; 99:151–157. PMID: 10918049.
Article8. Barwood CH, Murdoch BE. rTMS as a treatment for neurogenic communication and swallowing disorders. Acta Neurol Scand. 2013; 127:77–91. PMID: 22881826.
Article9. Khedr EM, Abo-Elfetoh N, Rothwell JC. Treatment of post-stroke dysphagia with repetitive transcranial magnetic stimulation. Acta Neurol Scand. 2009; 119:155–161. PMID: 18771521.
Article10. Khedr EM, Abo-Elfetoh N. Therapeutic role of rTMS on recovery of dysphagia in patients with lateral medullary syndrome and brainstem infarction. J Neurol Neurosurg Psychiatry. 2010; 81:495–499. PMID: 19828479.
Article11. Verin E, Leroi AM. Poststroke dysphagia rehabilitation by repetitive transcranial magnetic stimulation: a noncontrolled pilot study. Dysphagia. 2009; 24:204–210. PMID: 18956227.
Article12. Hamdy S, Mikulis DJ, Crawley A, Xue S, Lau H, Henry S, et al. Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Physiol. 1999; 277(1 Pt 1):G219–G225. PMID: 10409170.13. Zald DH, Pardo JV. The functional neuroanatomy of voluntary swallowing. Ann Neurol. 1999; 46:281–286. PMID: 10482257.
Article14. Martin RE, Goodyear BG, Gati JS, Menon RS. Cerebral cortical representation of automatic and volitional swallowing in humans. J Neurophysiol. 2001; 85:938–950. PMID: 11160524.
Article15. Mosier K, Bereznaya I. Parallel cortical networks for volitional control of swallowing in humans. Exp Brain Res. 2001; 140:280–289. PMID: 11681303.
Article16. Bestmann S, Baudewig J, Siebner HR, Rothwell JC, Frahm J. Subthreshold high-frequency TMS of human primary motor cortex modulates interconnected frontal motor areas as detected by interleaved fMRI-TMS. Neuroimage. 2003; 20:1685–1696. PMID: 14642478.
Article17. Reithler J, Peters JC, Sack AT. Multimodal transcranial magnetic stimulation: using concurrent neuroimaging to reveal the neural network dynamics of noninvasive brain stimulation. Prog Neurobiol. 2011; 94:149–165. PMID: 21527312.
Article18. Triggs WJ, McCoy KJ, Greer R, Rossi F, Bowers D, Kortenkamp S, et al. Effects of left frontal transcranial magnetic stimulation on depressed mood, cognition, and corticomotor threshold. Biol Psychiatry. 1999; 45:1440–1446. PMID: 10356626.
Article19. Beom J, Kim SJ, Han TR. Electrical stimulation of the suprahyoid muscles in brain-injured patients with dysphagia: a pilot study. Ann Rehabil Med. 2011; 35:322–327. PMID: 22506140.
Article20. Park SH, Song KS, Seo JH. Characteristics of motor evoked potential recording from swallowing muscles obtained by transcranial magnitic stimulation in healthy subjects. J Korean Acad Rehabil Med. 2009; 33:154–158.21. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article22. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–98. PMID: 8721066.
Article23. O'Neil KH, Purdy M, Falk J, Gallo L. The dysphagia outcome and severity scale. Dysphagia. 1999; 14:139–145. PMID: 10341109.24. Ludlow CL, Humbert I, Saxon K, Poletto C, Sonies B, Crujido L. Effects of surface electrical stimulation both at rest and during swallowing in chronic pharyngeal Dysphagia. Dysphagia. 2007; 22:1–10. PMID: 16718620.
Article25. Humbert IA, Poletto CJ, Saxon KG, Kearney PR, Crujido L, Wright-Harp W, et al. The effect of surface electrical stimulation on hyolaryngeal movement in normal individuals at rest and during swallowing. J Appl Physiol (1985). 2006; 101:1657–1663. PMID: 16873602.
Article26. Kim SJ, Han TR. Effect of surface electrical stimulation of suprahyoid muscles on hyolaryngeal movement. Neuromodulation. 2009; 12:134–140. PMID: 22151287.
Article27. Kim JH, Lee KJ, Kim SJ. Electrical stimulation on suprahyoid muscles of the brain injury patients with dysphagia. Korean J Stroke. 2007; 9:134–141.28. Jang SH, Ahn SH, Lee SJ, Ha JS, Lee H, Lee JH. The motor cortex mapping using transcranial magnetic stimulation in normal subjects. J Korean Acad Rehabil Med. 2000; 24:219–224.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Non-invasive Brain Stimulation on Dysphagia after Stroke
- Diagnosis With Manometry and Treatment With Repetitive Transcranial Magnetic Stimulation in Dysphagia
- Effect of Low-Frequency rTMS and NMES on Subacute Unilateral Hemispheric Stroke With Dysphagia
- Modulating Neural Network through rTMS
- Stroke Update 2011: Stroke Rehabilitation