Ann Rehabil Med.
2013 Dec;37(6):907-912. 10.5535/arm.2013.37.6.907.
Diagnosis With Manometry and Treatment With Repetitive Transcranial Magnetic Stimulation in Dysphagia
- Affiliations
-
- 1Department of Rehabilitation Medicine, Yeouido St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. sae_byuk@hotmail.com
- KMID: 2266573
- DOI: http://doi.org/10.5535/arm.2013.37.6.907
Abstract
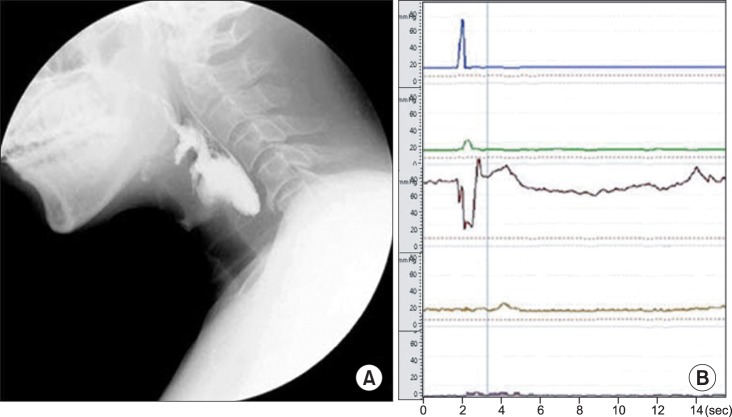
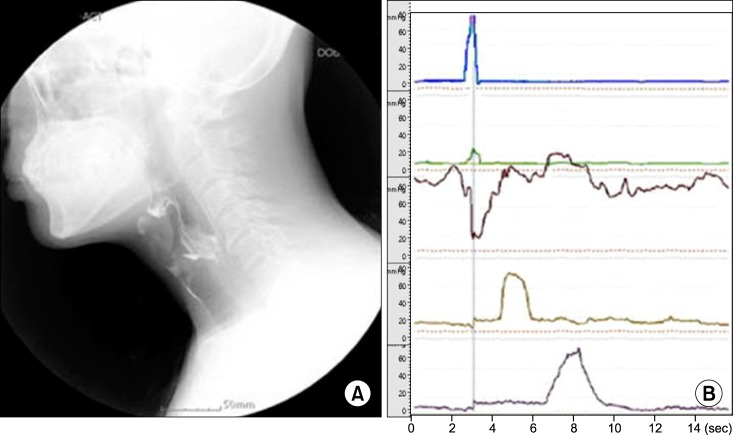
- Videofluoroscopic swallowing study (VFSS) used for the diagnosis of dysphagia has limitations in objectively assessing the contractility of the pharyngeal muscle or the degree of the upper esophageal sphincter relaxation. With a manometer, however, it is possible to objectively assess the pressure changes in the pharynx caused by pharyngeal muscle contraction during swallowing or upper esophageal sphincter relaxation, hence remedying the limitations of VFSS. The following case report describes a patient diagnosed with lateral medullar infarction presenting a 52-year-old male who had dysphagia. We suggested that the manometer could be used to assess the specific site of dysfunction in patients with dysphagia complementing the limitations of VFSS. We also found that repetitive transcranial magnetic stimulation was effective in treating patients refractory to traditional dysphagia rehabilitation.
MeSH Terms
Figure
Reference
-
1. Singh S, Hamdy S. Dysphagia in stroke patients. Postgrad Med J. 2006; 82:383–391. PMID: 16754707.
Article2. Sessle BJ, Henry JL. Neural mechanisms of swallowing: neurophysiological and neurochemical studies on brain stem neurons in the solitary tract region. Dysphagia. 1989; 4:61–75. PMID: 2484181.
Article3. Higo R, Tayama N, Watanabe T. Manometric abnormality in dysphagic patients after medullary cerebrovascular accidents. ORL J Otorhinolaryngol Relat Spec. 2002; 64:368–372. PMID: 12417783.
Article4. Jean A. Brainstem organization of the swallowing network. Brain Behav Evol. 1984; 25:109–116. PMID: 6100081.
Article5. Hila A, Castell JA, Castell DO. Pharyngeal and upper esophageal sphincter manometry in the evaluation of dysphagia. J Clin Gastroenterol. 2001; 33:355–361. PMID: 11606849.
Article6. Khedr EM, Abo-Elfetoh N. Therapeutic role of rTMS on recovery of dysphagia in patients with lateral medullary syndrome and brainstem infarction. J Neurol Neurosurg Psychiatry. 2010; 81:495–499. PMID: 19828479.
Article7. Jefferson S, Mistry S, Michou E, Singh S, Rothwell JC, Hamdy S. Reversal of a virtual lesion in human pharyngeal motor cortex by high frequency contralesional brain stimulation. Gastroenterology. 2009; 137:841–849. PMID: 19427312.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Non-invasive Brain Stimulation on Dysphagia after Stroke
- Predictors of Response to Repetitive Transcranial Magnetic Stimulation in Depression: A Review of Recent Updates
- Repetitive Transcranial Magnetic Stimulation for Limb-Kinetic Apraxia in Parkinson's Disease
- Treatment-Resistant Depression Entering Remission Following a Seizure during the Course of Repetitive Transcranial Magnetic Stimulation
- Early Augmentation Response with Low-frequency Repetitive Transcranial Magnetic Stimulation in Treatment Resistant Depression