J Korean Med Sci.
2015 Aug;30(8):1062-1067. 10.3346/jkms.2015.30.8.1062.
Clinical Significance of Persistent Tumor in Bone Marrow during Treatment of High-risk Neuroblastoma
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kwsped@skku.edu
- 2Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2164500
- DOI: http://doi.org/10.3346/jkms.2015.30.8.1062
Abstract
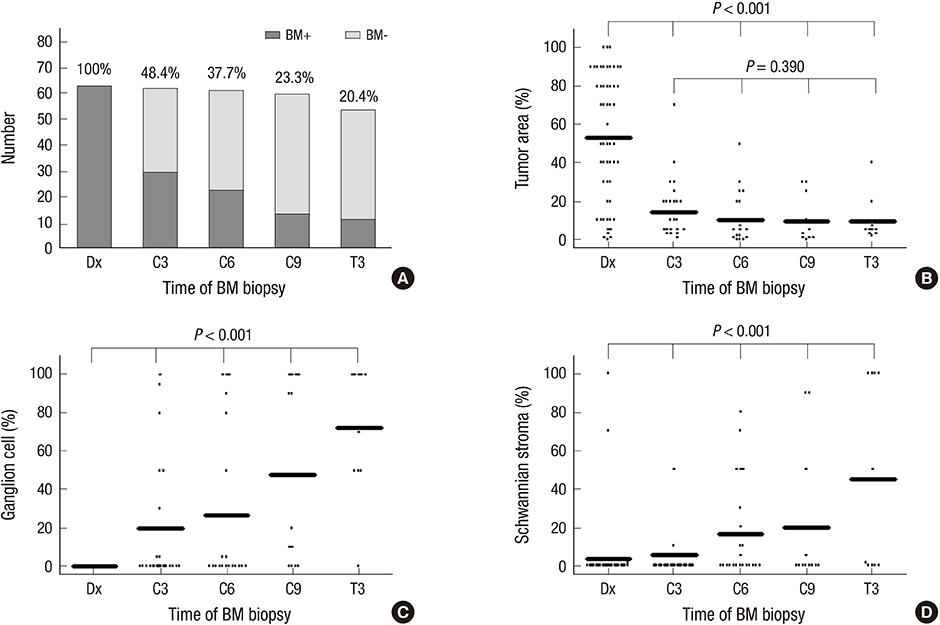
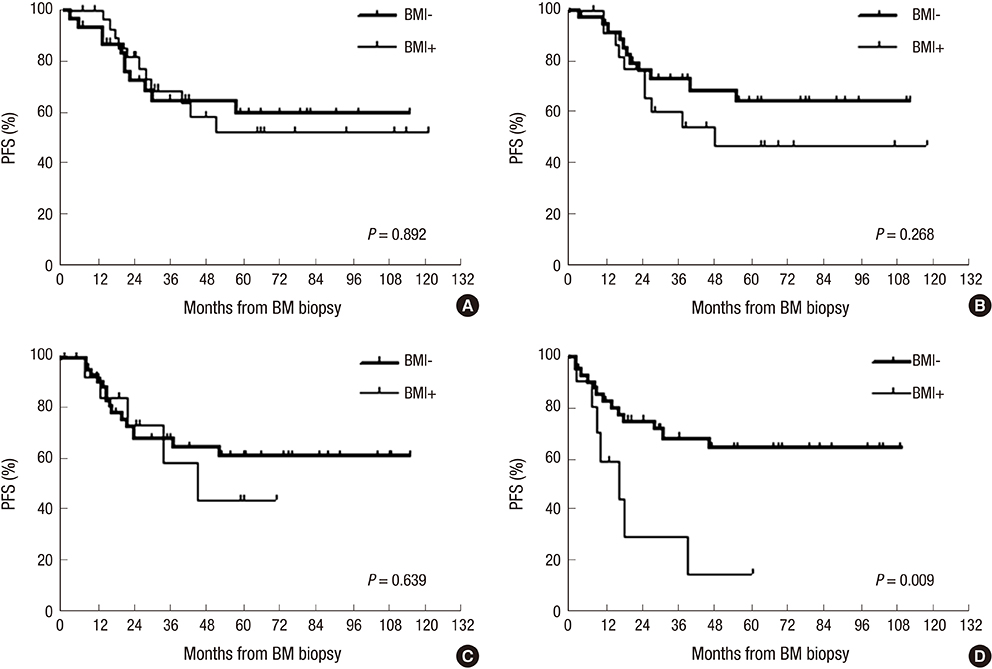
- The records of 63 high-risk neuroblastoma patients with bone marrow (BM) tumors at diagnosis were retrospectively reviewed. All patients received nine cycles of induction chemotherapy followed by tandem high-dose chemotherapy and autologous stem cell transplantation (HDCT/auto-SCT). Follow-up BM examination was performed every three cycles during induction chemotherapy and every three months for one year after the second HDCT/auto-SCT. BM tumor cells persisted in 48.4%, 37.7%, 23.3%, and 20.4% of patients after three, six, and nine cycles of induction chemotherapy and three months after the second HDCT/auto-SCT, respectively. There was no difference in progression-free survival (PFS) rate between patients with persistent BM tumor and those without during the induction treatment. However, after tandem HDCT/auto-SCT, the PFS rate was worse in patients with persistent BM tumor than in those without (probability of 5-yr PFS 14.7% +/- 13.4% vs. 64.2% +/- 8.3%, P = 0.009). Persistent BM tumor during induction treatment is not associated with a worse prognosis when intensive tandem HDCT/auto-SCT is given as consolidation treatment. However, persistent BM tumor after tandem HDCT/auto-SCT is associated with a worse prognosis. Therefore, further treatment might be needed in patients with persistent BM tumor after tandem HDCT/auto-SCT.
Keyword
MeSH Terms
-
Adolescent
Antineoplastic Combined Chemotherapy Protocols/administration & dosage
Bone Marrow Neoplasms/pathology/*secondary/*therapy
Child
Child, Preschool
Combined Modality Therapy/methods
Female
Humans
Induction Chemotherapy/methods
Infant
Infant, Newborn
Male
Neoplasms, Multiple Primary/pathology/*therapy
Neuroblastoma/*pathology/*therapy
Prognosis
Retrospective Studies
Risk Factors
Stem Cell Transplantation/*methods
Treatment Outcome
Young Adult
Figure
Cited by 1 articles
-
Clinical Significance of Segmental Chromosomal Aberrations in Patients with Neuroblastoma: First Report in Korean Population
Hana Lim, Meong Hi Son, Ju Kyung Hyun, Hee Won Cho, Hee Young Ju, Ji Won Lee, Keon Hee Yoo, Ki Woong Sung, Hong Hoe Koo
J Korean Med Sci. 2020;35(14):e82. doi: 10.3346/jkms.2020.35.e82.
Reference
-
1. Seeger RC, Reynolds CP, Gallego R, Stram DO, Gerbing RB, Matthay KK. Quantitative tumor cell content of bone marrow and blood as a predictor of outcome in stage IV neuroblastoma: a Children's Cancer Group Study. J Clin Oncol. 2000; 18:4067–4076.2. Fukuda M, Miyajima Y, Miyashita Y, Horibe K. Disease outcome may be predicted by molecular detection of minimal residual disease in bone marrow in advanced neuroblastoma: a pilot study. J Pediatr Hematol Oncol. 2001; 23:10–13.3. Cai JY, Pan C, Tang YJ, Chen J, Ye QD, Zhou M, Xue H, Tang JY. Minimal residual disease is a prognostic marker for neuroblastoma with bone marrow infiltration. Am J Clin Oncol. 2012; 35:275–278.4. Sung KW, Lee SH, Yoo KH, Jung HL, Cho EJ, Koo HH, Lee SK, Kim J, Lim DH, Suh YL, et al. Tandem high-dose chemotherapy and autologous stem cell rescue in patients over 1 year of age with stage 4 neuroblastoma. Bone Marrow Transplant. 2007; 40:37–45.5. Brodeur GM, Pritchard J, Berthold F, Carlsen NL, Castel V, Castelberry RP, De Bernardi B, Evans AE, Favrot M, Hedborg F, et al. Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin Oncol. 1993; 11:1466–1477.6. Peuchmaur M, d'Amore ES, Joshi VV, Hata J, Roald B, Dehner LP, Gerbing RB, Stram DO, Lukens JN, Matthay KK, et al. Revision of the International Neuroblastoma Pathology Classification: confirmation of favorable and unfavorable prognostic subsets in ganglioneuroblastoma, nodular. Cancer. 2003; 98:2274–2281.7. Sung KW, Son MH, Lee SH, Yoo KH, Koo HH, Kim JY, Cho EJ, Lee SK, Choi YS, Lim DH, et al. Tandem high-dose chemotherapy and autologous stem cell transplantation in patients with high-risk neuroblastoma: results of SMC NB-2004 study. Bone Marrow Transplant. 2013; 48:68–73.8. Ahn S, Lee JJ, Ha SY, Sung CO, Kim J, Han J. Clinicopathological analysis of 21 thymic neuroendocrine tumors. Korean J Pathol. 2012; 46:221–225.9. Lee SS, Kang M, Ha SY, An J, Roh MS, Ha CW, Han J. Morphologic analysis of pulmonary neuroendoscrine tumors. Korean J Pathol. 2013; 47:16–20.10. Lee ST, Suh YL, Ko YH, Ki CS, Sung KW, Kim HJ, Kim JW, Kim SH, Chueh H, Lee SH, et al. Measurement of tyrosine hydroxylase transcripts in bone marrow using biopsied tissue instead of aspirates for neuroblastoma. Pediatr Blood Cancer. 2010; 55:273–278.11. Yoo SY, Kim JS, Sung KW, Jeon TY, Choi JY, Moon SH, Son MH, Lee SH, Yoo KH, Koo HH. The degree of tumor volume reduction during the early phase of induction chemotherapy is an independent prognostic factor in patients with high-risk neuroblastoma. Cancer. 2013; 119:656–664.12. Burchill SA, Kinsey SE, Picton S, Roberts P, Pinkerton CR, Selby P, Lewis IJ. Minimal residual disease at the time of peripheral blood stem cell harvest in patients with advanced neuroblastoma. Med Pediatr Oncol. 2001; 36:213–219.13. Moss TJ, Cairo M, Santana VM, Weinthal J, Hurvitz C, Bostrom B. Clonogenicity of circulating neuroblastoma cells: implications regarding peripheral blood stem cell transplantation. Blood. 1994; 83:3085–3089.