Korean J Radiol.
2015 Jun;16(3):632-640. 10.3348/kjr.2015.16.3.632.
Quantitative Assessment of Global and Regional Air Trappings Using Non-Rigid Registration and Regional Specific Volume Change of Inspiratory/Expiratory CT Scans: Studies on Healthy Volunteers and Asthmatics
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea. seojb@amc.seoul.kr
- KMID: 2155534
- DOI: http://doi.org/10.3348/kjr.2015.16.3.632
Abstract
OBJECTIVE
The purpose of this study was to compare air trapping in healthy volunteers with asthmatics using pulmonary function test and quantitative data, such as specific volume change from paired inspiratory CT and registered expiratory CT.
MATERIALS AND METHODS
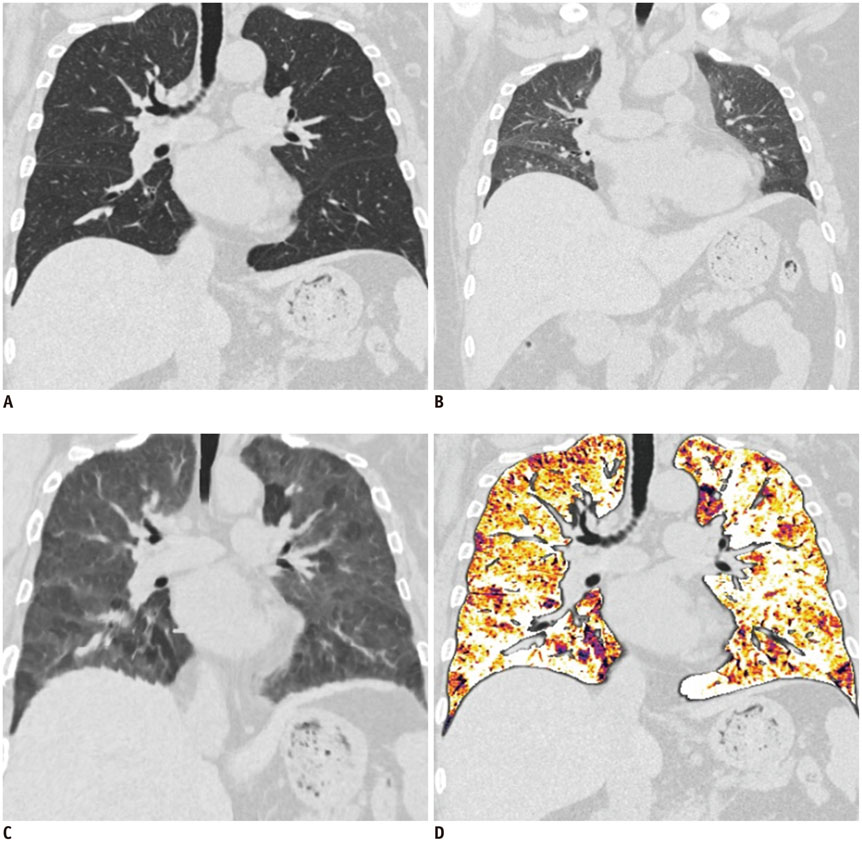
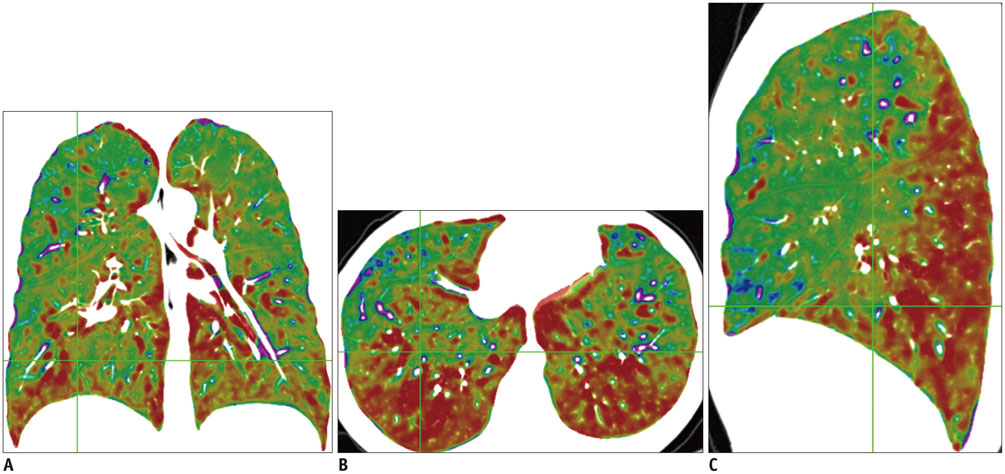
Sixteen healthy volunteers and 9 asthmatics underwent paired inspiratory/expiratory CT. DeltaSV, which represents the ratio of air fraction released after exhalation, was measured with paired inspiratory and anatomically registered expiratory CT scans. Air trapping indexes, DeltaSV0.4 and DeltaSV0.5, were defined as volume fraction of lung below 0.4 and 0.5 DeltaSV, respectively. To assess the gravity effect of air-trapping, DeltaSV values of anterior and posterior lung at three different levels were measured and DeltaSV ratio of anterior lung to posterior lung was calculated. Color-coded DeltaSV map of the whole lung was generated and visually assessed. Mean DeltaSV, DeltaSV0.4, and DeltaSV0.5 were compared between healthy volunteers and asthmatics. In asthmatics, correlation between air trapping indexes and clinical parameters were assessed.
RESULTS
Mean DeltaSV, DeltaSV0.4, and DeltaSV0.5 in asthmatics were significantly higher than those in healthy volunteer group (all p < 0.05). DeltaSV values in posterior lung in asthmatics were significantly higher than those in healthy volunteer group (p = 0.049). In asthmatics, air trapping indexes, such as DeltaSV0.5 and DeltaSV0.4, showed negative strong correlation with FEF25-75, FEV1, and FEV1/FVC. DeltaSV map of asthmatics showed abnormal geographic pattern in 5 patients (55.6%) and disappearance of anterior-posterior gradient in 3 patients (33.3%).
CONCLUSION
Quantitative assessment of DeltaSV (the ratio of air fraction released after exhalation) shows the difference in extent of air trapping between health volunteers and asthmatics.
MeSH Terms
Figure
Reference
-
1. National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007; 120:5 Suppl. S94–S138.2. Grant EN, Wagner R, Weiss KB. Observations on emerging patterns of asthma in our society. J Allergy Clin Immunol. 1999; 104(2 Pt 2):S1–S9.3. Anandan C, Nurmatov U, van Schayck OC, Sheikh A. Is the prevalence of asthma declining? Systematic review of epidemiological studies. Allergy. 2010; 65:152–167.4. Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001-2010. NCHS Data Brief. 2012; (94):1–8.5. Austin JH, Müller NL, Friedman PJ, Hansell DM, Naidich DP, Remy-Jardin M, et al. Glossary of terms for CT of the lungs: recommendations of the Nomenclature Committee of the Fleischner Society. Radiology. 1996; 200:327–331.6. Stern EJ, Frank MS. Small-airway diseases of the lungs: findings at expiratory CT. AJR Am J Roentgenol. 1994; 163:37–41.7. Arakawa H, Webb WR. Air trapping on expiratory high-resolution CT scans in the absence of inspiratory scan abnormalities: correlation with pulmonary function tests and differential diagnosis. AJR Am J Roentgenol. 1998; 170:1349–1353.8. Laurent F, Latrabe V, Raherison C, Marthan R, Tunon-de-Lara JM. Functional significance of air trapping detected in moderate asthma. Eur Radiol. 2000; 10:1404–1410.9. Park SW, Park JS, Jeong SH, Lee YN, Hwangbo Y, Park JS, et al. Air trapping is a major determinant of persistent airway obstruction in asthmatics. Respir Med. 2012; 106:786–793.10. Sorkness RL, Bleecker ER, Busse WW, Calhoun WJ, Castro M, Chung KF, et al. Lung function in adults with stable but severe asthma: air trapping and incomplete reversal of obstruction with bronchodilation. J Appl Physiol (1985). 2008; 104:394–403.11. Matsuoka S, Kurihara Y, Yagihashi K, Hoshino M, Watanabe N, Nakajima Y. Quantitative assessment of air trapping in chronic obstructive pulmonary disease using inspiratory and expiratory volumetric MDCT. AJR Am J Roentgenol. 2008; 190:762–769.12. Lee YK, Oh YM, Lee JH, Kim EK, Lee JH, Kim N, et al. Quantitative assessment of emphysema, air trapping, and airway thickening on computed tomography. Lung. 2008; 186:157–165.13. Mets OM, Isgum I, Mol CP, Gietema HA, Zanen P, Prokop M, et al. Variation in quantitative CT air trapping in heavy smokers on repeat CT examinations. Eur Radiol. 2012; 22:2710–2717.14. Mets OM, van Hulst RA, Jacobs C, van Ginneken B, de Jong PA. Normal range of emphysema and air trapping on CT in young men. AJR Am J Roentgenol. 2012; 199:336–340.15. Lee J, Kim N, Seo JB, Lee H, Shin YG. Automatic non-rigid lung registration method for the visualization of regional air trapping in chest CT scans. New York: The First International Workshop on Pulmonary Image Processing;2008. p. 195–201.16. Barbosa EM Jr, Song G, Tustison N, Kreider M, Gee JC, Gefter WB, et al. Computational analysis of thoracic multidetector row HRCT for segmentation and quantification of small airway air trapping and emphysema in obstructive pulmonary disease. Acad Radiol. 2011; 18:1258–1269.17. Kim EY, Seo JB, Lee HJ, Kim N, Lee E, Lee SM, et al. Detailed analysis of the density change on chest CT of COPD using non-rigid registration of inspiration/expiration CT scans. Eur Radiol. 2015; 25:541–549.18. Tanaka N, Matsumoto T, Miura G, Emoto T, Matsunaga N, Ueda K, et al. Air trapping at CT: high prevalence in asymptomatic subjects with normal pulmonary function. Radiology. 2003; 227:776–785.19. Fuld MK, Easley RB, Saba OI, Chon D, Reinhardt JM, Hoffman EA, et al. CT-measured regional specific volume change reflects regional ventilation in supine sheep. J Appl Physiol (1985). 2008; 104:1177–1184.20. Gevenois PA, de Maertelaer V, De Vuyst P, Zanen J, Yernault JC. Comparison of computed density and macroscopic morphometry in pulmonary emphysema. Am J Respir Crit Care Med. 1995; 152:653–657.21. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008; 31:143–178.22. Silva CI, Colby TV, Müller NL. Asthma and associated conditions: high-resolution CT and pathologic findings. AJR Am J Roentgenol. 2004; 183:817–824.23. Lynch DA, Newell JD, Tschomper BA, Cink TM, Newman LS, Bethel R. Uncomplicated asthma in adults: comparison of CT appearance of the lungs in asthmatic and healthy subjects. Radiology. 1993; 188:829–833.24. Park CS, Müller NL, Worthy SA, Kim JS, Awadh N, Fitzgerald M. Airway obstruction in asthmatic and healthy individuals: inspiratory and expiratory thin-section CT findings. Radiology. 1997; 203:361–367.25. Regan EA, Hokanson JE, Murphy JR, Make B, Lynch DA, Beaty TH, et al. Genetic epidemiology of COPD (COPDGene) study design. COPD. 2010; 7:32–43.26. Yoon SH, Goo JM, Jung J, Hong H, Park EA, Lee CH, et al. Computer-aided classification of visual ventilation patterns in patients with chronic obstructive pulmonary disease at two-phase xenon-enhanced CT. Korean J Radiol. 2014; 15:386–396.27. Yin Y, Hoffman EA, Lin CL. Mass preserving nonrigid registration of CT lung images using cubic B-spline. Med Phys. 2009; 36:4213–4222.28. Torigian DA, Gefter WB, Affuso JD, Emami K, Dougherty L. Application of an optical flow method to inspiratory and expiratory lung MDCT to assess regional air trapping: a feasibility study. AJR Am J Roentgenol. 2007; 188:W276–W280.29. Simon BA. Non-invasive imaging of regional lung function using x-ray computed tomography. J Clin Monit Comput. 2000; 16:433–442.30. Fujita H, Morita M, Kusaka M. [Study of a CT scanning method that improves gravity effects to enable differentiation of inflammatory diseases in chest CT]. Nihon Hoshasen Gijutsu Gakkai Zasshi. 2008; 64:707–713.31. Volpe J, Storto ML, Lee K, Webb WR. High-resolution CT of the lung: determination of the usefulness of CT scans obtained with the patient prone based on plain radiographic findings. AJR Am J Roentgenol. 1997; 169:369–374.32. Bankier AA, Estenne M, Kienzl D, Müller-Mang C, Van Muylem A, Gevenois PA. Gravitational gradients in expiratory computed tomography examinations of patients with small airways disease: effect of body position on extent of air trapping. J Thorac Imaging. 2010; 25:311–319.33. West JB, Dollery CT. Distribution of blood flow and ventilation-perfusion ratio in the lung, measured with radioactive carbon dioxide. J Appl Physiol. 1960; 15:405–410.34. Galvin I, Drummond GB, Nirmalan M. Distribution of blood flow and ventilation in the lung: gravity is not the only factor. Br J Anaesth. 2007; 98:420–428.35. Moore WC, Bleecker ER, Curran-Everett D, Erzurum SC, Ameredes BT, Bacharier L, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. J Allergy Clin Immunol. 2007; 119:405–413.36. Tgavalekos NT, Musch G, Harris RS, Vidal Melo MF, Winkler T, Schroeder T, et al. Relationship between airway narrowing, patchy ventilation and lung mechanics in asthmatics. Eur Respir J. 2007; 29:1174–1181.37. Boon AW, Ward-McQuaid JM, Milner AD, Hopkin IE. Thoracic gas volume, helium functional residual capacity and air-trapping in the first six hours of life: the effect of oxygen administration. Early Hum Dev. 1981; 5:157–166.38. Chae EJ, Seo JB, Lee J, Kim N, Goo HW, Lee HJ, et al. Xenon ventilation imaging using dual-energy computed tomography in asthmatics: initial experience. Invest Radiol. 2010; 45:354–361.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation between Expiratory Increase of Lung Attenuation and Age and Smoking in the Subjects with Normal Inspiratory Low Dose CT and Pulmonary Function Test
- Cystic Lung Disease: a Comparison of C ystic Size, as Seen on Expira tory and Inspiratory HRCT Scans
- New Method for Combined Quantitative Assessment of Air-Trapping and Emphysema on Chest Computed Tomography in Chronic Obstructive Pulmonary Disease: Comparison with Parametric Response Mapping
- Measurement of Lung Volumes: Usefulness of Spiral CT
- Global and Regional Ventilation during High Flow Nasal Cannula in Patients with Hypoxia