Korean J Radiol.
2000 Jun;1(2):84-90. 10.3348/kjr.2000.1.2.84.
Cystic Lung Disease: a Comparison of C ystic Size, as Seen on Expira tory and Inspiratory HRCT Scans
- Affiliations
-
- 1Department of Diagnostic Radiology, Dong-A University College of Medicine, Pusan, Korea.
- KMID: 966478
- DOI: http://doi.org/10.3348/kjr.2000.1.2.84
Abstract
OBJECTIVE
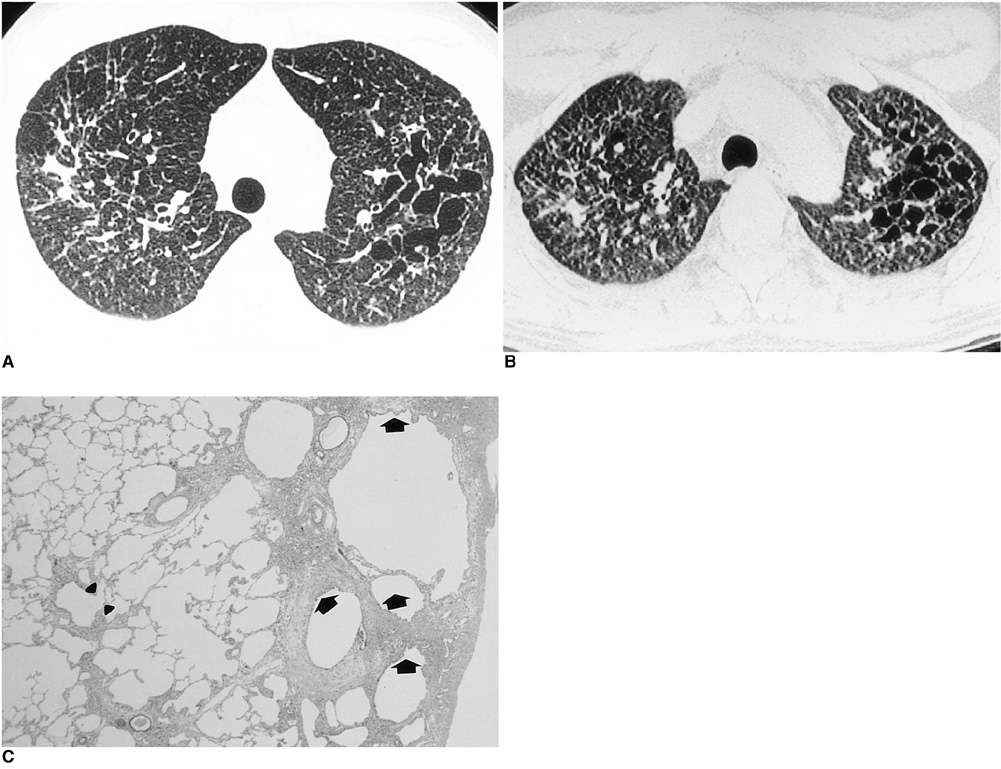
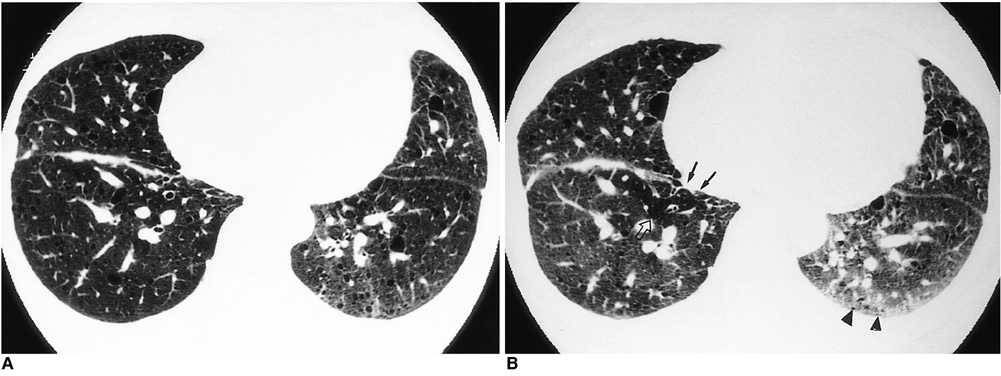
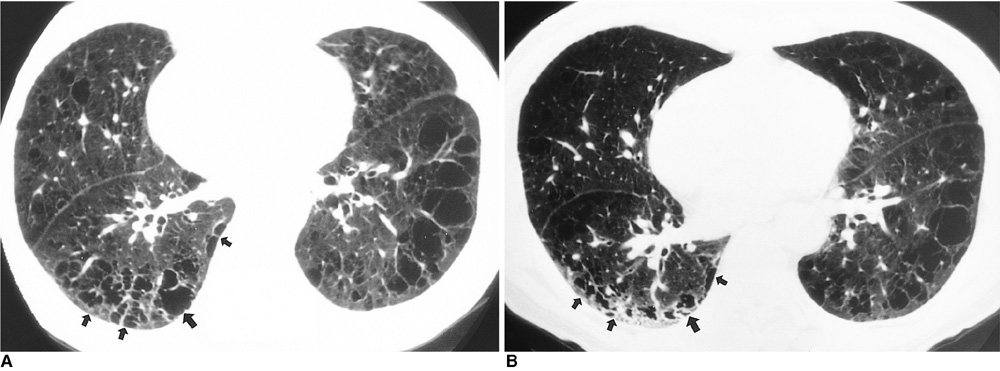
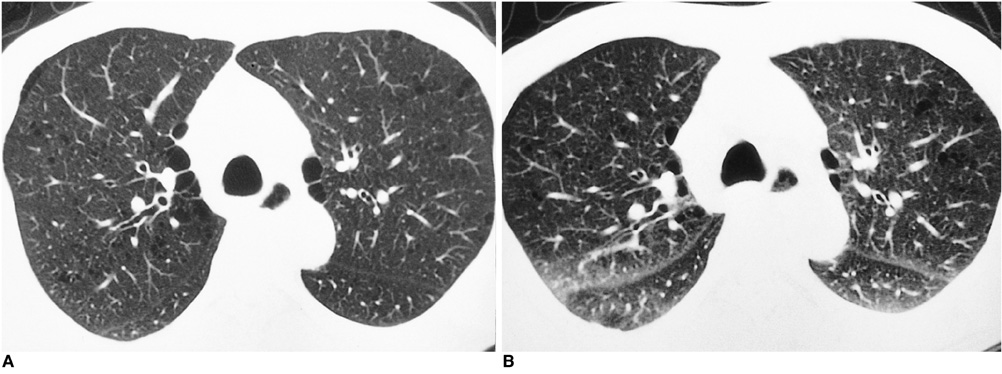
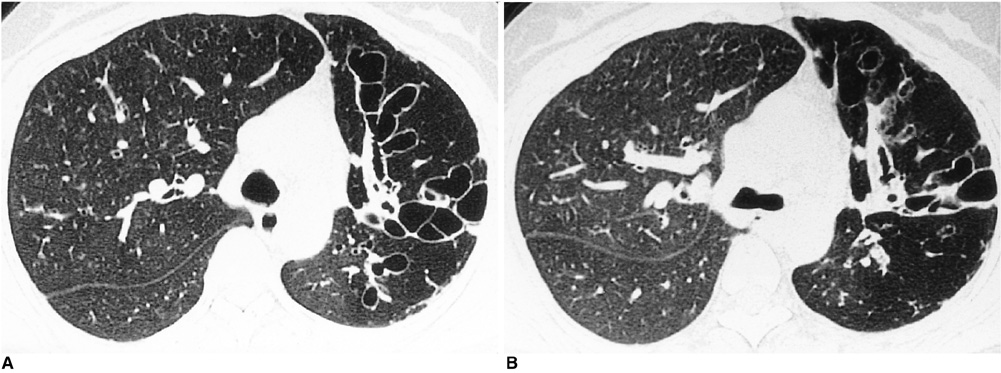
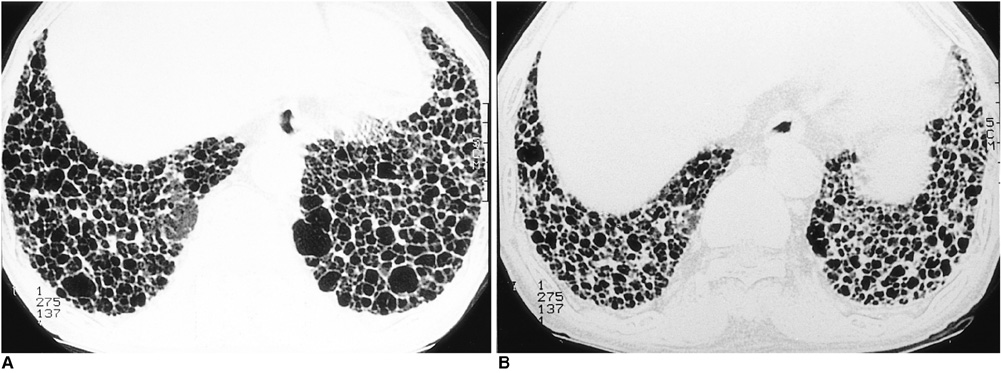
To determine the effects of respiration on the size of lung cysts by comparing inspiratory and expiratory high-resolution CT (HRCT) scans. MATERIALS AND METHODS: The authors evaluated the size of cystic lesions, as seen on paired inspiratory and expiratory HRCT scans, in 54 patients with Langerhans cell histiocytosis (n = 3), pulmonary lymphangiomyomatosis (n = 4),confluent centrilobular emphysema (n = 9), paraseptal emphysema and bullae (n= 16), cystic bronchiectasis (n = 13), and honeycombing (n = 9). Using paired inspiratory and expiratory HRCT scans obtained at the corresponding anatomic level, a total of 270 cystic lesions were selected simultaneously on the basis of five lesions per lung disease. Changes in lung cyst size observed during respiration were assessed by two radiologists. In a limited number of cases (n = 11), pathologic specimens were obtained by open lung biopsy or lobectomy. RESULTS: All cystic lesions in patients with Langerhans cell histiocytosis, lymphangiomyomatosis, cystic bronchiectasis, honeycombing, and confluent centrilobular emphysema became smaller on expiration, but in two cases of paraseptal emphysema and bullae there was no change. CONCLUSION: In cases in which expiratory CT scans indicate that cysts have become smaller, cystic lesions may communicate with the airways. To determine whether, for cysts and cystic lesions, this connection does in fact exist, paired inspiratory and expiratory HRCT scans are necessary.
MeSH Terms
Figure
Reference
-
1. Stern EJ, Webb WR, Golden JA, et al. Cystic lung disease associated with eosinophilic granuloma and tuberous sclerosis: air trapping at dynamic ultrafast high resolution CT. Radiology. 1992. 182:325–329.2. Worthy SA, Brown MJ, Müller NL. Technical report: air spaces in the lung: change in size on expiratory high-resolution CT in 23 patients. Clin Radiol. 1998. 53:515–519.3. Marti-Bonmati L, Catala FJ, Ruiz-Perales F. Computed tomography differentiation between cystic bronchiectasis and bullae. J Thorac Imaging. 1991. 7:83–85.4. Aquinno SL, Webb WR, Zaloudek CJ, Stern EJ. Lung cysts associated with honeycombing: change in size on expiratory CT scans. AJR. 1994. 162:583–584.5. Kuhlman JE, Reyes BL, Hruban RH, et al. Abnormal air-filled spaces in the lung. RadioGraphics. 1993. 13:47–75.6. Moore AD, Godwin JD, Müller NL, et al. Pulmonary histiocytosis X: comparison of radiographic and CT findings. Radiology. 1989. 172:249–254.7. Brauner MW, Grenier P, Mouelhi MM, et al. Pulmonary histiocytosis X: evaluation with high resolution CT. Radiology. 1989. 172:255–258.8. Carrington CB, Cugell DW, Gaensler EA, et al. Lymphangioleiomyomatosis: physilologic-pathologic-radiologic correlations. Am Rev Respir Dis. 1977. 116:977–995.9. Fukuda Y, Kawamoto M, Yamamoto A, et al. Role of elastic fiber degradation in emphysema-like lesions of pulmonary lymphangiomyomatosis. Hum Pathol. 1990. 21:1252–1261.10. Fraser RS, Müller NL, Colman N, Pare PD. Chronic obstructive lung disease. Diagnosis of disease of the chest. 1999. 4th ed. Philadelphia: Saunders;2168–2263.11. Naidich DP, Webb WR, Müller NL, Krinsky GA, Zerhouni EA, Siegelman SS. Computed tomography and magnetic resonance of the thorax. 1999. Philadelphia: Lippincott-Raven;381–464.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bronchiectasis with Decreased Attenuation Areas on HRCT: Correlation with Pulmonary Function Test
- DILD (diffuse infiltrative lung disease); Radiologic Diagnostic Approach According to High-Resolution CT Pattern
- Late Lung Parenchymal Changes on HRCT in Children with mycoplasma Pneumonia
- High-Resolution Computed Tomography(HRCT)Findings of the Lung in Asthmatic Children and Their Correlation with Clinical Characteristics
- Diagnosis of idiopathic pulmonary fibrosis