J Korean Med Sci.
2014 Nov;29(Suppl 3):S228-S236. 10.3346/jkms.2014.29.S3.S228.
Gene Therapy Using Hepatocyte Growth Factor Expressing Adenovirus Improves Skin Flap Survival in a Rat Model
- Affiliations
-
- 1Institute for Human Tissue Restoration, Department of Plastic & Reconstructive Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. pswjlee@yuhs.ac
- 2Department of Plastic & Reconstructive Surgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Bioengineering, College of Engineering, Hanyang University, Seoul, Korea.
- KMID: 2151418
- DOI: http://doi.org/10.3346/jkms.2014.29.S3.S228
Abstract
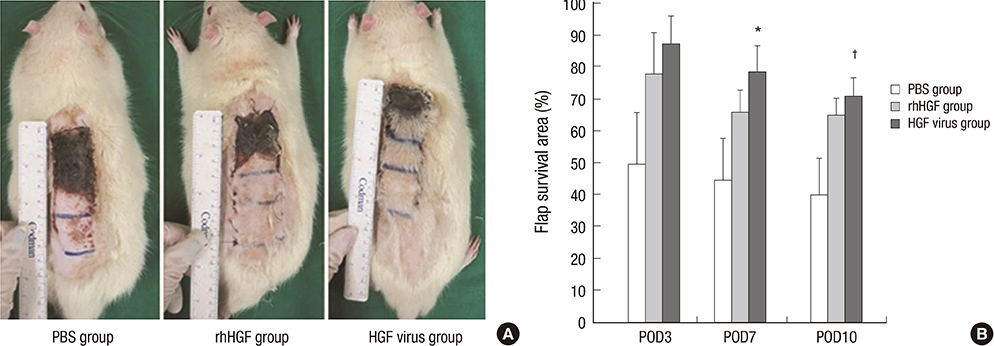
- Hepatocyte growth factor (HGF) is a potent angiogenic factor that can stimulate the production of blood vessels in ischemic tissue. We investigated whether gene therapy using HGF-expressing adenovirus could enhance skin flap survival. Sprague-Dawley rats were randomly divided into three groups. Rats were subdermally injected with HGF-expressing adenovirus (HGF virus group), recombinant HGF (rhHGF group), or phosphate buffered saline (PBS group) 2 days before and immediately after 3 x 9 cm caudal flap elevation. The survival area of the skin flap, the ratio of blood flow, CD31-positive vessels and, VEGF expression were examined. Skin flap viability was significantly increased in the HGF virus group compared to the rhHGF and PBS groups (71.4% +/- 5.9%, 63.8%+/- 6.4%, and 39.2% +/- 13.0%, respectively) (P = 0.025). Furthermore, the blood flow ratio was significantly increased in the HGF virus group. In the HGF virus group, the number of CD31-positive vessels and vascular endothelial growth factor (VEGF) expression were significantly increased. Gene therapy using HGF-expressing adenovirus increase VEGF expression, the number of viable capillaries, and blood flow to the flap, thereby improving skin flap survival.
Keyword
MeSH Terms
-
Adenoviridae/genetics
Animals
Genetic Therapy/*methods
Graft Survival/genetics
Hepatocyte Growth Factor/biosynthesis/*genetics
Male
Models, Animal
Neovascularization, Physiologic/*genetics
Random Allocation
Rats
Rats, Sprague-Dawley
Reconstructive Surgical Procedures
Skin Transplantation/*methods
Surgical Flaps/*surgery
Hepatocyte Growth Factor
Figure
Reference
-
1. Yoon TH, Yun IS, Rha DK, Lee WJ. Reconstruction of various perinasal defects using facial artery perforator-based nasolabial island flaps. Arch Plast Surg. 2013; 40:754–760.2. Nakagawa A, Makino H, Aoki M, Miyake T, Shiraya S, Nakamura T, Ogihara T, Kimata Y, Morishita R. Improvement of survival of skin flaps by combined gene transfer of hepatocyte growth factor and prostacyclin synthase. J Gene Med. 2007; 9:1087–1094.3. Khan A, Ashrafpour H, Huang N, Neligan PC, Kontos C, Zhong A, Forrest CR, Pang CY. Acute local subcutaneous VEGF165 injection for augmentation of skin flap viability: efficacy and mechanism. Am J Physiol Regul Integr Comp Physiol. 2004; 287:R1219–R1229.4. Scalise A, Tucci MG, Lucarini G, Giantomassi F, Orlando F, Pierangeli M, Pugnaloni A, Bertani A, Ricotti G, Biagini G. Local rh-VEGF administration enhances skin flap survival more than other types of rh-VEGF administration: a clinical, morphological and immunohistochemical study. Exp Dermatol. 2004; 13:682–690.5. Maldonado C, Stadelmann WK, Ramirez S, Quan EE, Barker JH. Preconditioning of latissimus dorsi muscle flaps with monophosphoryl lipid a. Plast Reconstr Surg. 2003; 111:267–274.6. Seify H, Bilkay U, Jones G. Improvement of TRAM flap viability using human VEGF-induced angiogenesis: a comparative study of delay techniques. Plast Reconstr Surg. 2003; 112:1032–1039.7. Huang N, Khan A, Ashrafpour H, Neligan PC, Forrest CR, Kontos CD, Pang CY. Efficacy and mechanism of adenovirus-mediated VEGF-165 gene therapy for augmentation of skin flap viability. Am J Physiol Heart Circ Physiol. 2006; 291:H127–H137.8. Hopper RA, Forrest CR, Xu H, Zhong A, He W, Rutka J, Neligan P, Pang CY. Role and mechanism of PKC in ischemic preconditioning of pig skeletal muscle against infarction. Am J Physiol Regul Integr Comp Physiol. 2000; 279:R666–R676.9. Nakamura T, Mizuno S. The discovery of hepatocyte growth factor (HGF) and its significance for cell biology, life sciences and clinical medicine. Proc Jpn Acad Ser B Phys Biol Sci. 2010; 86:588–610.10. Song MB, Yu XJ, Zhu GX, Chen JF, Zhao G, Huang L. Transfection of HGF gene enhances endothelial progenitor cell (EPC) function and improves EPC transplant efficiency for balloon-induced arterial injury in hypercholesterolemic rats. Vascul Pharmacol. 2009; 51:205–213.11. Lee KH, Kim JR. Hepatocyte growth factor induced up-regulations of VEGF through Egr-1 in hepatocellular carcinoma cells. Clin Exp Metastasis. 2009; 26:685–692.12. Mikroulis D, Papanas N, Maltezos E, Bougioukas G. Angiogenic growth factors in the treatment of peripheral arterial disease. Curr Vasc Pharmacol. 2007; 5:195–209.13. Cho KR, Choi JS, Hahn W, Kim DS, Park JS, Lee DS, Kim KB. Therapeutic angiogenesis using naked DNA expressing two isoforms of the hepatocyte growth factor in a porcine acute myocardial infarction model. Eur J Cardiothorac Surg. 2008; 34:857–863.14. Taniyama Y, Morishita R, Aoki M, Nakagami H, Yamamoto K, Yamazaki K, Matsumoto K, Nakamura T, Kaneda Y, Ogihara T. Therapeutic angiogenesis induced by human hepatocyte growth factor gene in rat and rabbit hindlimb ischemia models: preclinical study for treatment of peripheral arterial disease. Gene Ther. 2001; 8:181–189.15. Taniyama Y, Morishita R, Hiraoka K, Aoki M, Nakagami H, Yamasaki K, Matsumoto K, Nakamura T, Kaneda Y, Ogihara T. Therapeutic angiogenesis induced by human hepatocyte growth factor gene in rat diabetic hind limb ischemia model: molecular mechanisms of delayed angiogenesis in diabetes. Circulation. 2001; 104:2344–2350.16. Morishita R, Nakamura S, Hayashi S, Taniyama Y, Moriguchi A, Nagano T, Taiji M, Noguchi H, Takeshita S, Matsumoto K, et al. Therapeutic angiogenesis induced by human recombinant hepatocyte growth factor in rabbit hind limb ischemia model as cytokine supplement therapy. Hypertension. 1999; 33:1379–1384.17. Morishita R, Sakaki M, Yamamoto K, Iguchi S, Aoki M, Yamasaki K, Matsumoto K, Nakamura T, Lawn R, Ogihara T, et al. Impairment of collateral formation in lipoprotein(a) transgenic mice: therapeutic angiogenesis induced by human hepatocyte growth factor gene. Circulation. 2002; 105:1491–1496.18. Yang ZJ, Chen B, Sheng Z, Zhang DG, Jia EZ, Wang W, Ma DC, Zhu TB, Wang LS, Li CJ, et al. Improvement of heart function in postinfarct heart failure swine models after hepatocyte growth factor gene transfer: comparison of low-, medium- and high-dose groups. Mol Biol Rep. 2010; 37:2075–2081.19. Liu KX, Kato Y, Narukawa M, Kim DC, Hanano M, Higuchi O, Nakamura T, Sugiyama Y. Importance of the liver in plasma clearance of hepatocyte growth factors in rats. Am J Physiol. 1992; 263:G642–G649.20. Yang ZJ, Zhang YR, Chen B, Zhang SL, Jia EZ, Wang LS, Zhu TB, Li CJ, Wang H, Huang J, et al. Phase I clinical trial on intracoronary administration of Ad-hHGF treating severe coronary artery disease. Mol Biol Rep. 2009; 36:1323–1329.21. Lubiatowski P, Goldman CK, Gurunluoglu R, Carnevale K, Siemionow M. Enhancement of epigastric skin flap survival by adenovirus-mediated VEGF gene therapy. Plast Reconstr Surg. 2002; 109:1986–1993.22. Wu H, Yoon AR, Li F, Yun CO, Mahato RI. RGD peptide-modified adenovirus expressing hepatocyte growth factor and X-linked inhibitor of apoptosis improves islet transplantation. J Gene Med. 2011; 13:658–669.23. St George JA. Gene therapy progress and prospects: adenoviral vectors. Gene Ther. 2003; 10:1135–1141.24. Ghali S, Dempsey MP, Jones DM, Grogan RH, Butler PE, Gurtner GC. Plastic surgical delivery systems for targeted gene therapy. Ann Plast Surg. 2008; 60:323–332.25. Zheng Y, Yi C, Xia W, Ding T, Zhou Z, Han Y, Guo S. Mesenchymal stem cells transduced by vascular endothelial growth factor gene for ischemic random skin flaps. Plast Reconstr Surg. 2008; 121:59–69.26. Mack CA, Magovern CJ, Budenbender KT, Patel SR, Schwarz EA, Zanzonico P, Ferris B, Sanborn T, Isom P, Ferris B, et al. Salvage angiogenesis induced by adenovirus-mediated gene transfer of vascular endothelial growth factor protects against ischemic vascular occlusion. J Vasc Surg. 1998; 27:699–709.27. Lee WJ, Yun CO, Yun IS, Kim YO, Choi IK, Yun TJ, Rah DK. Augmentation of rat skin flap viability by relaxin-expressing adenovirus. Wound Repair Regen. 2011; 19:709–717.28. Nakamura Y, Morishita R, Higaki J, Kida I, Aoki M, Moriguchi A, Yamada K, Hayashi S, Yo Y, Nakano H, et al. Hepatocyte growth factor is a novel member of the endothelium-specific growth factors: additive stimulatory effect of hepatocyte growth factor with basic fibroblast growth factor but not with vascular endothelial growth factor. J Hypertens. 1996; 14:1067–1072.29. Birukova AA, Alekseeva E, Mikaelyan A, Birukov KG. HGF attenuates thrombin-induced endothelial permeability by Tiam1-mediated activation of the Rac pathway and by Tiam1/Rac-dependent inhibition of the Rho pathway. FASEB J. 2007; 21:2776–2786.30. Makiuchi A, Yamaura K, Mizuno S, Matsumoto K, Nakamura T, Amano J, Ito K. Hepatocyte growth factor prevents pulmonary ischemia-reperfusion injury in mice. J Heart Lung Transplant. 2007; 26:935–943.31. Ito W, Kanehiro A, Matsumoto K, Hirano A, Ono K, Maruyama H, Kataoka M, Nakamura T, Gelfand EW, Tanimoto M. Hepatocyte growth factor attenuates airway hyperresponsiveness, inflammation, and remodeling. Am J Respir Cell Mol Biol. 2005; 32:268–280.32. Kamimoto M, Mizuno S, Matsumoto K, Nakamura T. Hepatocyte growth factor prevents multiple organ injuries in endotoxemic mice through a heme oxygenase-1-dependent mechanism. Biochem Biophys Res Commun. 2009; 380:333–337.33. Liu PY, Wang XT, Badiavas E, Rieger-Christ K, Tang JB, Summerhayes I. Enhancement of ischemic flap survival by prefabrication with transfer of exogenous PDGF gene. J Reconstr Microsurg. 2005; 21:273–279.34. Jung H, Gurunluoglu R, Scharpf J, Siemionow M. Adenovirus-mediated angiopoietin-1 gene therapy enhances skin flap survival. Microsurgery. 2003; 23:374–380.35. Chung KI, Kim HK, Kim WS, Bae TH. The effects of polydeoxyribonucleotide on the survival of random pattern skin flaps in rats. Arch Plast Surg. 2013; 40:181–186.36. Makino H, Aoki M, Hashiya N, Yamasaki K, Hiraoka K, Shimizu H, Azuma J, Kurinami H, Ogihara T, Morishita R. Increase in peripheral blood flow by intravenous administration of prostaglandin E1 in patients with peripheral arterial disease, accompanied by up-regulation of hepatocyte growth factor. Hypertens Res. 2004; 27:85–91.37. Aoki M, Morishita R, Hayashi S, Jo N, Matsumoto K, Nakamura T, Kaneda Y, Ogihara T. Inhibition of neointimal formation after balloon injury by cilostazol, accompanied by improvement of endothelial dysfunction and induction of hepatocyte growth factor in rat diabetes model. Diabetologia. 2001; 44:1034–1042.38. Tsai JW, Ayubi FS, Hart KL, Baur DA, Parham MA, Moon JK, Vazquez R, Chasen AB, Zhang Z, Pizarro JM. Evaluation of the effect of sildenafil and vascular endothelium growth factor combination treatment on skin flap survival in rats. Aesthetic Plast Surg. 2008; 32:624–631.39. Ahi YS, Bangari DS, Mittal SK. Adenoviral vector immunity: its implications and circumvention strategies. Curr Gene Ther. 2011; 11:307–320.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Relaxin Expressing Adenovirus for Rat Skin Flap Viability
- Improvement of the Inferior Epigastric Artery Flap Viability Using Adenovirus-mediated VEGF and COMP-angiopoietin-1
- Enhancement of Transduction Efficiency and Antitumor Effects of IL-12N220L-expressing Adenovirus by Co-delivery of DOTAP
- Adenoviral mediated hepatocyte growth factor gene attenuates hyperglycemia and beta cell destruction in overt diabetic mice
- Effect of fractional ablative carbon dioxide laser with lidocaine spray on skin flap survival in rats