Korean J Perinatol.
2013 Dec;24(4):322-325. 10.14734/kjp.2013.24.4.322.
Scalp Abscess Developing Dura Mater Extension in a Newborn Infant : A Case Eeport
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, Pusan National University, Busan, Korea. byun410@hanmail.net
- KMID: 2072311
- DOI: http://doi.org/10.14734/kjp.2013.24.4.322
Abstract
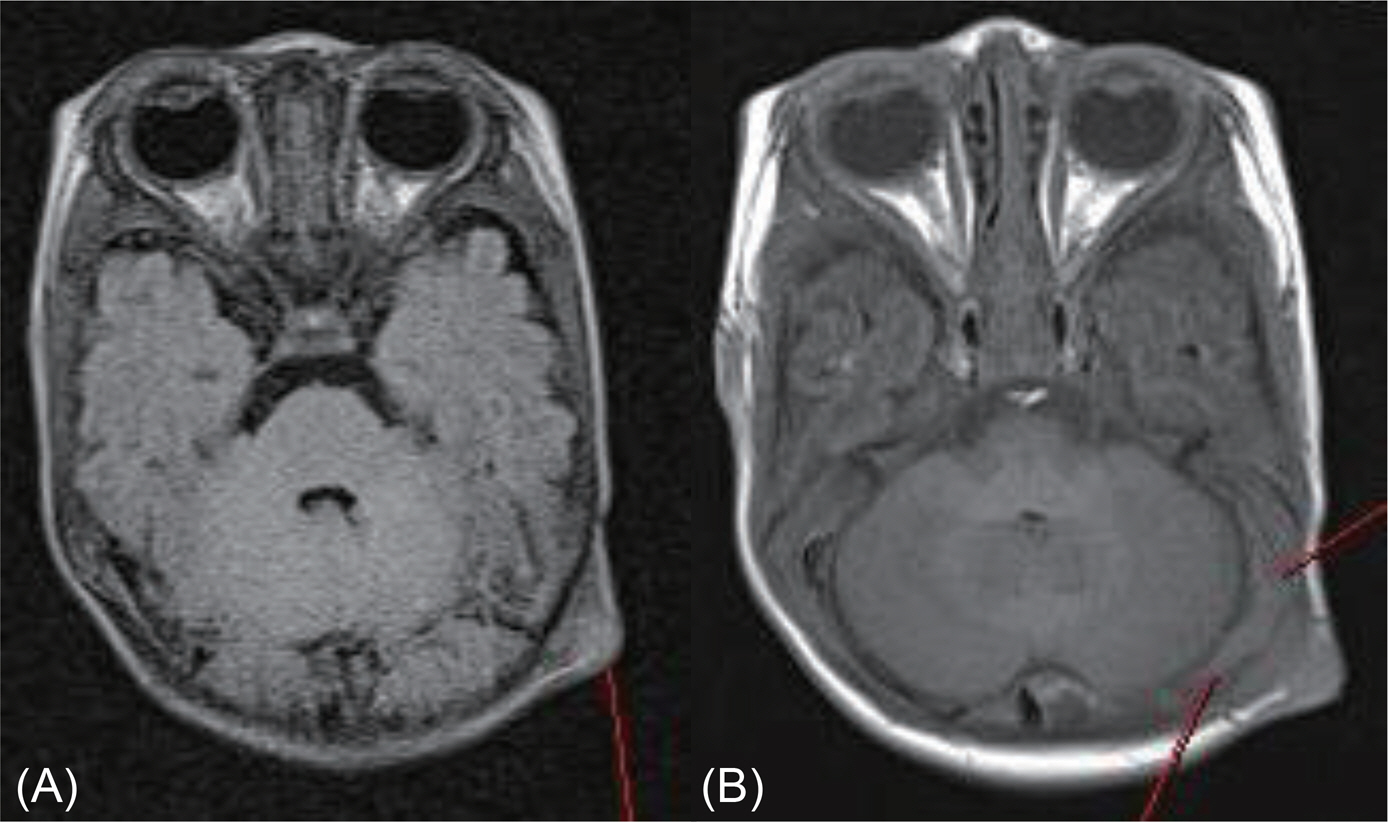
- The risk factors associated with neonatal scalp abscess include electrode insertion for fetal scalp monitoring, traumatic scalp lacerations, and sepsis or meningitis. We report a case of neonatal scalp abscess with extension to dura mater, although our patient had no known risk factors. A 18-day-old, full-term baby was referred to the our hospital to evaluate a swelling over his left occipital scalp. A full sepsis work-up was performed and all were negative. Cranial sonography revealed echogenic cystic mass with peripheral vascularity consistent with ruptured epidermoid cyst or scalp abscess. The computed tomography (CT) scan of head was performed because of possibility of ruptured epidermoid cyt and revealed 2.0x2.0 cm sized hyperattenuating mass with suspicious intracranial extension. The magnetic resonance imaging (MRI) of head revealed the presence of 1.4x1.1 cm sized peripheral rim enhancing mass at left occipital area consistent with scalp abscess. And also, the lesion was suspicious dural exposure at left temporal area. Clinicians should be aware that scalp abscess may occur without any risk factors and perform diagnostic workup including a complete sepsis evaluation, cerebrospinal fluid analysis (CSF), and cranial imaging study to screen for intracranial extension.
Keyword
MeSH Terms
Figure
Reference
-
1). Okada DM., Chow AW., Bruce VT. Neonatal scalp abscess and fetal monitoring: factors associated with infection. Am J Obstet Gynecol. 1977. 129:185–9.
Article2). Cordero L., Anderson CW., Zuspan FP. Scalp abscess: a benign and infrequent complication of fetal monitoring. Am J Obstet Gynecol. 1983. 146:126–30.
Article3). Chang HY., Cheug KS., Liu YP., Hung HF., Fu HW. Neonatal infected subgaleal hematoma: an unusual complication of early-onset E. coli sepsis. Pediatr Neonatol. 2013. xx:1–3.
Article4). Sola A., Bednarek FJ., Davidson R., Griffin BE. Meningitis, ventriculitis, and hydrocephalus: a complication of fetal monitoring. Obstet Gynecol. 1980. 56:663–5.5). Listinsky JL., Wood BP., Ekholm SE. Parietal osteomyelitis and epidural abscess: a delayed complication of fetal monitoring. Pediatr Radiol. 1986. 16:150–1.
Article6). Freedman RM., Baltimore R. Fetal Streptococcus viridians septicemia and meningitis: relationship to fetal scalp electrode monitoring. J Perinatol. 1990. 10:272–4.7). Jonkhoff-Slok TW., Weyerman ME. Scalp electrode associated neonatal Escherichia coli meningitis-a case report. J Perinat Med. 1991. 19:217–9.8). Beier KH., Heegaard W., Rusnak RA. Acute neonatal scalp abscess and E coli bacteremia in the ED. Am J Emerg Med. 1999. 17:241–3.
Article9). Koot RW., Reedijk B., Tan WF. De Sonnaville-De Roy Van Zuide. Neonatal brain abscess: complication of fetal monitoring. Obstet Gynecol. 1999. 93:857.
Article10). Plavidal FJ., Werch A. Fetal scalp abscess secondary to intrauterine monitoring. Am J Obstet Gynecol. 1975. 125:65–70.
Article11). Weiner EJ., Mclntosh MS., Joseph MM., Maraga N., Davis PG. Neonatal scalp abscess: is it benign disease? J Emerg Med. 2011. 40:97–101.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Fibrous Histiocytoma of the Pericranium with Intracranial Extension: A Case Report
- The Treatment for The Intractable Epidural Abscess Using Tensor Fascia Lata Graft and Anterolateral Thigh Free Flap
- A case of scalp abscess caused by Achromobacter xylosoxidans after vacuum delivery
- Aggressive Squamous Cell Carcinoma of the Scalp with Invasion into the Skull and Dura Mater
- Lyophilized Dura Mater Patch Graft in Glaucoma Valve Implantation