Korean J Urol.
2012 Sep;53(9):657-661. 10.4111/kju.2012.53.9.657.
Malignant Inflammatory Myofibroblastic Tumor of the Bladder with Rapid Progression
- Affiliations
-
- 1Department of Urology, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. hongkooha@pusan.ac.kr
- 2Medical Research Institute, Pusan National University Hospital, Busan, Korea.
- 3Department of Urology, Kosin University College of Medicine, Busan, Korea.
- KMID: 2061707
- DOI: http://doi.org/10.4111/kju.2012.53.9.657
Abstract
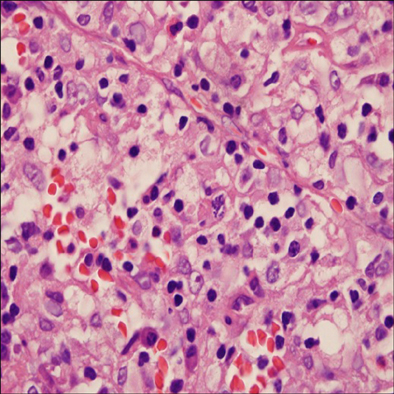
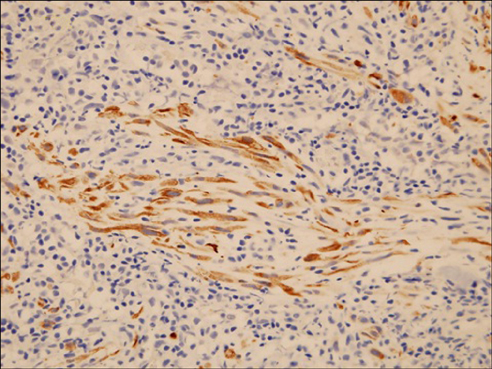
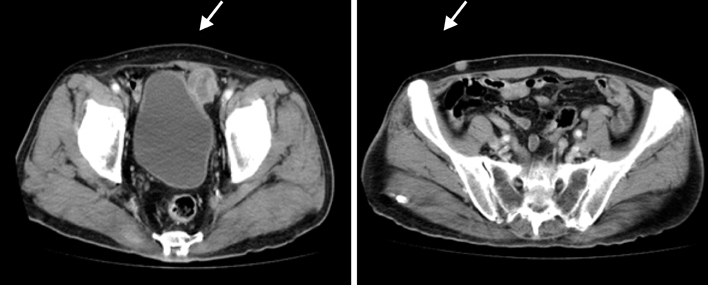
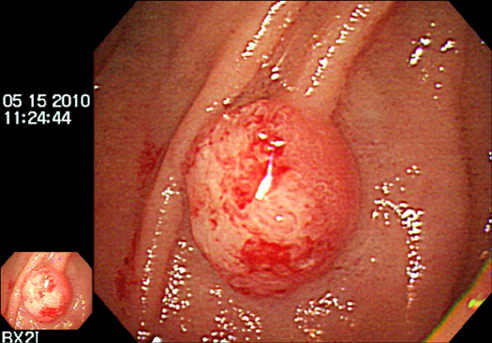
- A 71-year-old man was referred for painless hematuria and a bladder tumor. Cystoscopy and computed tomography revealed a 3-cm oval nodular mass on the left lateral side of the bladder. The patient underwent a complete transurethral resection of the lesion and histology showed a proliferation of atypical spindle cells with inflammation consistent with a myofibroblastic tumor. After 4 and 7 months, follow-up cystoscopy demonstrated nodular mass lesions and transurethral resection of bladder tumor was done, which showed chronic cystitis and a recurred myofibroblastic tumor, respectively. Five months later, multiple lymph node, bone, and soft tissue metastases were found by positron emission tomography. The patient was treated first with palliative chemotherapy, including doxorubicin and cisplatin. After that, radiologic studies showed disease progression but the patient refused further treatment and died 6 months later.
MeSH Terms
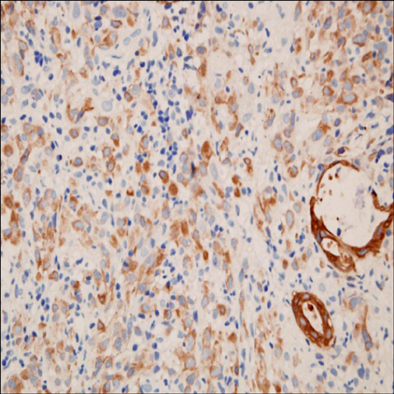
Figure
Reference
-
1. Coffin CM, Watterson J, Priest JR, Dehner LP. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol. 1995. 19:859–872.2. Dishop MK, Warner BW, Dehner LP, Kriss VM, Greenwood MF, Geil JD, et al. Successful treatment of inflammatory myofibroblastic tumor with malignant transformation by surgical resection and chemotherapy. J Pediatr Hematol Oncol. 2003. 25:153–158.3. Roth JA. Reactive pseudosarcomatous response in urinary bladder. Urology. 1980. 16:635–637.4. Young RH. Pseudoneoplastic lesions of the urinary bladder and urethra: a selective review with emphasis on recent information. Semin Diagn Pathol. 1997. 14:133–146.5. Li HB, Xu YM, Yu JJ. Diagnostic puzzle of inflammatory pseudotumor of the urinary bladder: a case report with brief literature review. South Med J. 2010. 103:563–566.6. Fujiwara T, Sugimura K, Imaoka I, Igawa M. Inflammatory pseudotumor of the bladder: MR findings. J Comput Assist Tomogr. 1999. 23:558–561.7. Arber DA, Weiss LM, Chang KL. Detection of Epstein-Barr virus in inflammatory pseudotumor. Semin Diagn Pathol. 1998. 15:155–160.8. Yamamoto H, Oda Y, Saito T, Sakamoto A, Miyajima K, Tamiya S, et al. p53 Mutation and MDM2 amplification in inflammatory myofibroblastic tumours. Histopathology. 2003. 42:431–439.9. Montgomery EA, Shuster DD, Burkart AL, Esteban JM, Sgrignoli A, Elwood L, et al. Inflammatory myofibroblastic tumors of the urinary tract: a clinicopathologic study of 46 cases, including a malignant example inflammatory fibrosarcoma and a subset associated with high-grade urothelial carcinoma. Am J Surg Pathol. 2006. 30:1502–1512.10. Lu CH, Huang HY, Chen HK, Chuang JH, Ng SH, Ko SF. Huge pelvi-abdominal malignant inflammatory myofibroblastic tumor with rapid recurrence in a 14-year-old boy. World J Gastroenterol. 2010. 16:2698–2701.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory Myofibroblastic Tumor of the Bladder: Report of Two Cases
- Inflammatory Myofibroblastic Tumor of Nasal Septum after Septoplasty: A Case Report
- Inflammatory Myofibroblastic Tumor of Kidney
- Inflammatory Myofibroblastic Tumor of the Urinary Bladder in a Young Patient With Gross Hematuria: A Case Report
- A Case of Inflammatory Myofibroblastic Tumor of the Urethra with Overactive Bladder