Chonnam Med J.
2013 Dec;49(3):118-124. 10.4068/cmj.2013.49.3.118.
Effect of Atorvastatin-Eluting Stents in a Rabbit Iliac Artery Restenosis Model
- Affiliations
-
- 1Korea Cardiovascular Stent Institute of Chonnam National University, Gwangju, Korea. myungho@chollian.net
- 2Cardiovascular Research Center, Chonnam National University Hospital, Gwangju, Korea.
- 3Regeneromics Research Center, Chonnam National University, Gwangju, Korea.
- KMID: 2048816
- DOI: http://doi.org/10.4068/cmj.2013.49.3.118
Abstract
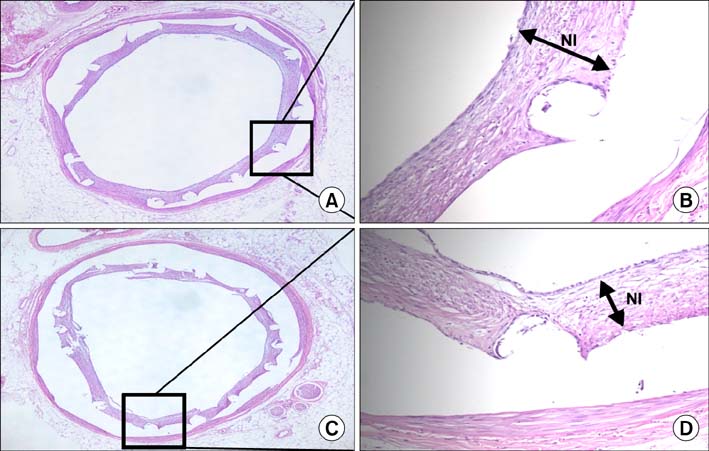
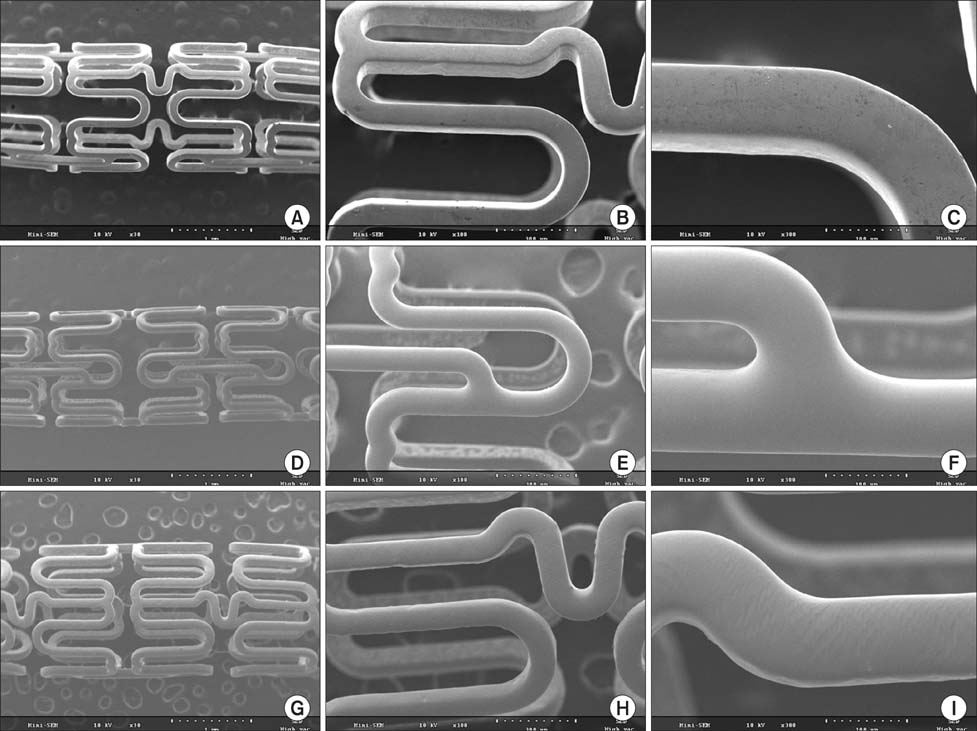
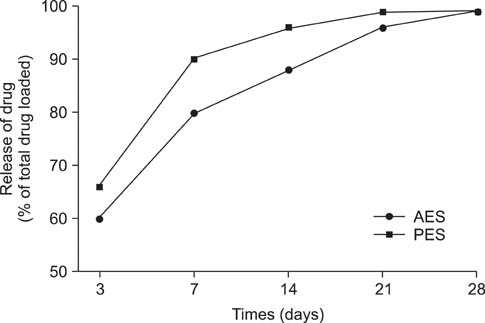
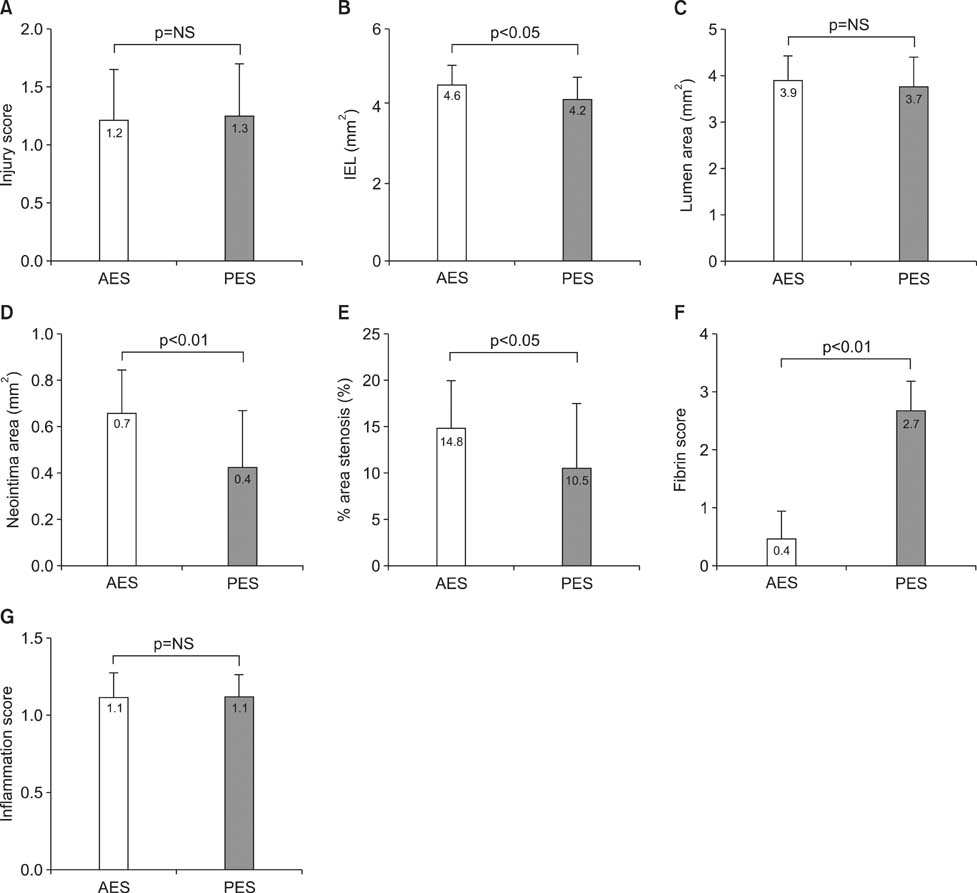
- Statins have pleiotropic effects, which include the inhibition of neointima hyperplasia, the inhibition of vascular inflammation, and platelet inhibition. The aim of this study was to examine the effect of an atorvastatin-eluting stent (AES) in a rabbit iliac artery overstretch restenosis model. Ten rabbits were used in this study (10 rabbits, 10 iliac arteries for each stent). An AES and paclitaxel-eluting stent (PES) were implanted in the left and right iliac arteries in a rabbit (2 stents in each rabbit). The stents were deployed with oversizing (stent/artery ratio 1.3:1), and histopathologic analysis was assessed at 28 days after stenting. There were no significant differences in the injury score, lumen area, or inflammation score. There were significant differences in the neointimal area (0.7+/-0.18 mm2 in the AES group vs. 0.4+/-0.25 mm2 in the PES group, p<0.01), in the percentage stenosis area (14.8+/-5.06% in the AES group vs. 10.5+/-6.80% in the PES group, p<0.05), and in the fibrin score (0.4+/-0.51 in the AES group vs. 2.7+/-0.48 in the PES group, p<0.001). Although the AES did not suppress neointimal hyperplasia compared with the PES, it showed a superior arterial healing effect in a rabbit iliac artery overstretch restenosis model.
Keyword
MeSH Terms
Figure
Reference
-
1. Vorpahl M, Yazdani SK, Nakano M, Ladich E, Kolodgie FD, Finn AV, et al. Pathobiology of stent thrombosis after drug-eluting stent implantation. Curr Pharm Des. 2010; 16:4064–4071.
Article2. Wolfrum S, Jensen KS, Liao JK. Endothelium-dependent effects of statins. Arterioscler Thromb Vasc Biol. 2003; 23:729–736.
Article3. Dimmeler S, Aicher A, Vasa M, Mildner-Rihm C, Adler K, Tiemann M, et al. HMG-CoA reductase inhibitors (statins) increase endothelial progenitor cells via the PI 3-kinase/Akt pathway. J Clin Invest. 2001; 108:391–397.
Article4. Werner N, Priller J, Laufs U, Endres M, Böhm M, Dirnagl U, et al. Bone marrow-derived progenitor cells modulate vascular reendothelialization and neointimal formation: effect of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibition. Arterioscler Thromb Vasc Biol. 2002; 22:1567–1572.
Article5. Fukumoto Y, Libby P, Rabkin E, Hill CC, Enomoto M, Hirouchi Y, et al. Statins alter smooth muscle cell accumulation and collagen content in established atheroma of watanabe heritable hyperlipidemic rabbits. Circulation. 2001; 103:993–999.
Article6. Lim KS, Bae IH, Kim JH, Park DS, Kim JM, Kim JH, et al. Mechanical and histopathological comparison between commercialized and newly designed coronary bare metal stents in a porcine coronary restenosis model. Chonnam Med J. 2013; 49:7–13.
Article7. Kim DM, Lee BS, Park CH, Park KD, Son TI, Jeong MH, et al. Metal surface coating using electrospray of biodegradable polymers and -lipoic acid release behavior for drug-eluting stents. Polym Korea. 2010; 34:178–183.
Article8. Garasic JM, Edelman ER, Squire JC, Seifert P, Williams MS, Rogers C. Stent and artery geometry determine intimal thickening independent of arterial injury. Circulation. 2000; 101:812–818.
Article9. Rogers C, Edelman ER. Endovascular stent design dictates experimental restenosis and thrombosis. Circulation. 1995; 91:2995–3001.
Article10. Schwartz RS, Huber KC, Murphy JG, Edwards WD, Camrud AR, Vlietstra RE, et al. Restenosis and the proportional neointimal response to coronary artery injury: results in a porcine model. J Am Coll Cardiol. 1992; 19:267–274.
Article11. Schwartz RS, Edelman E, Virmani R, Carter A, Granada JF, Kaluza GL, et al. Drug-eluting stents in preclinical studies: updated consensus recommendations for preclinical evaluation. Circ Cardiovasc Interv. 2008; 1:143–153.12. Kolodgie FD, John M, Khurana C, Farb A, Wilson PS, Acampado E, et al. Sustained reduction of in-stent neointimal growth with the use of a novel systemic nanoparticle paclitaxel. Circulation. 2002; 106:1195–1198.
Article13. LaDisa JF Jr, Meier HT, Olson LE, Kersten JR, Warltier DC, Pagel PS. Antegrade iliac artery stent implantation for the temporal and spatial examination of stent-induced neointimal hyperplasia and alterations in regional fluid dynamics. J Pharmacol Toxicol Methods. 2005; 51:115–121.
Article14. Veillard NR, Mach F. Statins: the new aspirin? Cell Mol Life Sci. 2002; 59:1771–1786.
Article15. Werner N, Nickenig G, Laufs U. Pleiotropic effects of HMG-CoA reductase inhibitors. Basic Res Cardiol. 2002; 97:105–116.
Article16. Fukuda D, Enomoto S, Shirakawa I, Nagai R, Sata M. Fluvastatin accelerates re-endothelialization impaired by local sirolimus treatment. Eur J Pharmacol. 2009; 612:87–92.
Article17. Mihos CG, Salas MJ, Santana O. The pleiotropic effects of the hydroxy-methyl-glutaryl-CoA reductase inhibitors in cardiovascular disease: a comprehensive review. Cardiol Rev. 2010; 18:298–304.
Article18. Serruys PW, de Feyter P, Macaya C, Kokott N, Puel J, Vrolix M, et al. Lescol Intervention Prevention Study (LIPS) Investigators. Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. JAMA. 2002; 287:3215–3222.
Article19. Pasceri V, Patti G, Nusca A, Pristipino C, Richichi G, Di Sciascio G. ARMYDA Investigators. Randomized trial of atorvastatin for reduction of myocardial damage during coronary intervention: results from the ARMYDA (Atorvastatin for Reduction of MYocardial Damage during Angioplasty) study. Circulation. 2004; 110:674–678.
Article20. Mobarrez F, He S, Bröijersen A, Wiklund B, Antovic A, Antovic J, et al. Atorvastatin reduces thrombin generation and expression of tissue factor, P-selectin and GPIIIa on platelet-derived microparticles in patients with peripheral arterial occlusive disease. Thromb Haemost. 2011; 106:344–352.
Article21. Pendyala L, Yin X, Li J, Shinke T, Xu Y, Chen JP, et al. Polymer-free cerivastatin-eluting stent shows superior neointimal inhibitionwith preserved vasomotor function compared to polymer-based paclitaxel-eluting stent in rabbit iliac arteries. EuroIntervention. 2010; 6:126–133.
Article22. Jaschke B, Michaelis C, Milz S, Vogeser M, Mund T, Hengst L, et al. Local statintherapy differentially interferes with smooth muscle and endothelial cell proliferation and reduces neointima on a drug-eluting stent platform. Cardiovasc Res. 2005; 68:483–492.
Article23. Miyauchi K, Kasai T, Yokayama T, Aihara K, Kurata T, Kajimoto K, et al. Effectiveness of statin-eluting stent on early inflammatory response and neointimal thickness in a porcine coronary model. Circ J. 2008; 72:832–838.
Article24. Kaesemeyer WH, Caldwell RB, Huang J, Caldwell RW. Pravastatin sodium activates endothelial nitric oxide synthase independent of its cholesterol-lowering actions. J Am Coll Cardiol. 1999; 33:234–241.
Article25. Stone GW, Ellis SG, Cox DA, Hermiller J, O'Shaughnessy C, Mann JT, et al. TAXUS-IV Investigators. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med. 2004; 350:221–231.
Article26. Grube E, Lansky A, Hauptmann KE, Di Mario C, Di Sciascio G, Colombo A, et al. SCORE Randomized Trial. High-dose 7-hexanoyltaxol-eluting stent with polymer sleeves for coronary revascularization: one-year results from the SCORE randomized trial. J Am Coll Cardiol. 2004; 44:1368–1372.
Article27. Lim SY, Jeong MH, Hong SJ, Lim do S, Moon JY, Hong YJ, et al. Inflammation and delayed endothelization with overlapping drug-eluting stents in a porcine model of in-stent restenosis. Circ J. 2008; 72:463–468.
Article28. Andrié RP, Bauriedel G, Braun P, Höpp HW, Nickenig G, Skowasch D. Increased expression of C-reactive protein and tissue factor in acute coronary syndrome lesions: Correlation with serum C-reactive protein, angioscopic findings, and modification by statins. Atherosclerosis. 2009; 202:135–143.
Article29. Malik N, Gunn J, Holt CM, Shepherd L, Francis SE, Newman CM, et al. Intravascular stents: a new technique for tissue processing for histology, immunohistochemistry, and transmission electron microscopy. Heart. 1998; 80:509–516.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drug-Eluting Stent Strut Fracture as a Cause of Restenosis
- Systemic drug therapy and restenosis after drug-eluting stent implantation
- Coronary Restenosis after Drug-Eluting Stent Implantation in Diabetic Patients
- Drug-Eluting Stent Used to Treat a Case of Recurrent Right Coronary Artery In-Stent Restenoses often Accompanied by Acute Inferior Wall Myocardial Infarction
- MDCT Application for Coronary Artery Intervention