Validation of Global Longitudinal Strain and Strain Rate as Reliable Markers of Right Ventricular Dysfunction: Comparison with Cardiac Magnetic Resonance and Outcome
- Affiliations
-
- 1Department of Cardiovascular Medicine, Cleveland Clinic, Cleveland, OH, USA. tom.marwick@utas.edu.au
- 2Cardiology Division of Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea.
- 3Menzies Research Institute Tasmania, Hobart, Australia.
- KMID: 2045426
- DOI: http://doi.org/10.4250/jcu.2014.22.3.113
Abstract
- BACKGROUND
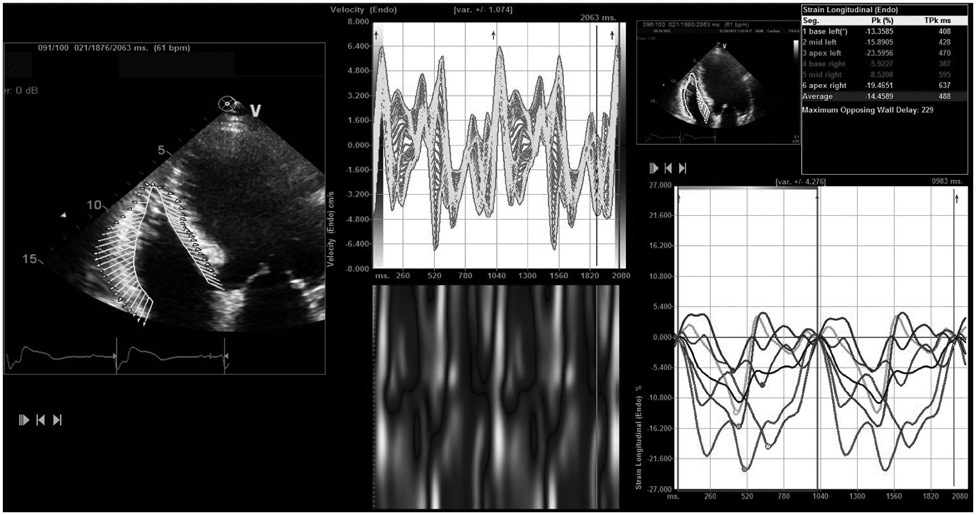
Right ventricular (RV) dysfunction in ischemic cardiomyopathy (ICM) is associated with poor prognosis, but RV assessment by conventional echocardiography remains difficult. We sought to validate RV global longitudinal strain (RVGLS) and global longitudinal strain rate (RVGLSR) against cardiac magnetic resonance (CMR) and outcome in ICM.
METHODS
In 57 patients (43 men, 64 +/- 12 years) with ICM who underwent conventional and strain echocardiography and CMR, RVGLS and RVGLSR were measured off-line. RV dysfunction was determined by CMR [RV ejection fraction (RVEF) < 50%]. Patients were followed over 15 +/- 9 months for a composite of death and hospitalization for worsening heart failure.
RESULTS
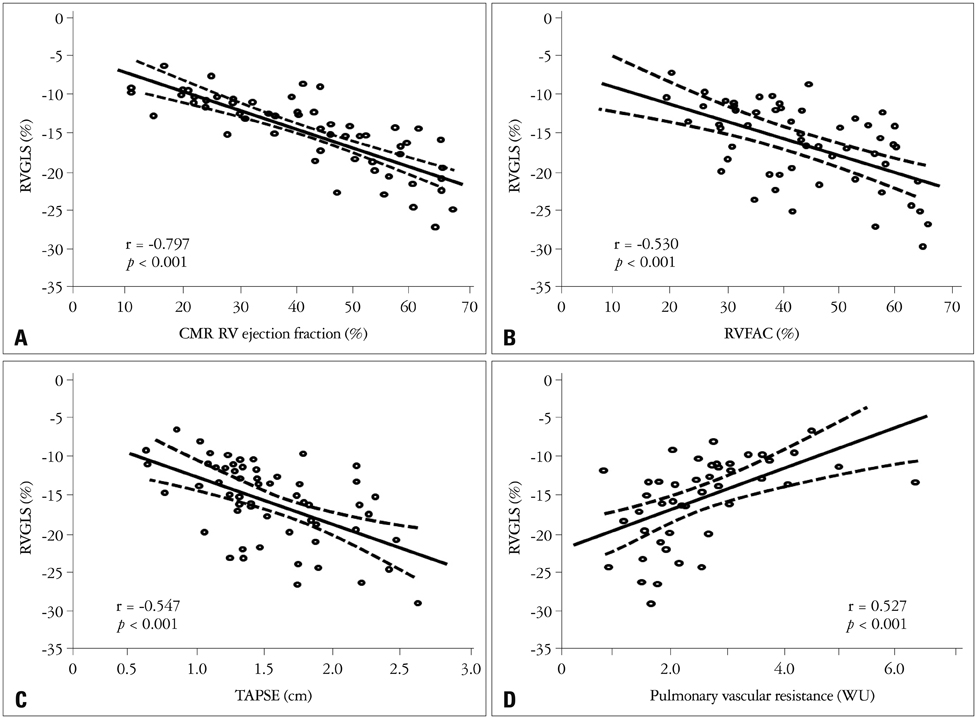
RVGLS showed significant correlations with CMR RVEF (r = -0.797, p < 0.01), RV fractional area change (RVFAC, r = -0.530, p < 0.01), and tricuspid annular plane systolic excursion (TAPSE, r = -0.547, p < 0.01). RVGLSR showed significant correlations between CMR RVEF (r = -0.668, p < 0.01), RVFAC (r = -0.394, p < 0.01), and TAPSE (r = -0.435, p < 0.01). RVGLS and RVGLSR showed significant correlations with pulmonary vascular resistance (r = 0.527 and r = 0.500, p < 0.01, respectively). The best cutoff value of RVGLS for detection of RV dysfunction was -15.4% [areas under the curve (AUC) = 0.955, p < 0.01] with a sensitivity of 81% and specificity 95%. The best cutoff value for RVGLSR was -0.94 s-1 (AUC = 0.871, p < 0.01), sensitivity 72%, specificity 86%. During follow-up, there were 12 adverse events. In Cox-proportional hazard regression analysis, impaired RVGLS [hazard ratio (HR) = 5.46, p = 0.030] and impaired RVGLSR (HR = 3.95, p = 0.044) were associated with adverse clinical outcome.
CONCLUSION
Compared with conventional echocardiographic parameters, RVGLS and RVGLSR correlate better with CMR RVEF and outcome.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Two-dimensional Echocardiographic Assessment of Myocardial Strain: Important Echocardiographic Parameter Readily Useful in Clinical Field
Jae-Hyeong Park
Korean Circ J. 2019;49(10):908-931. doi: 10.4070/kcj.2019.0200.Accurate and Reproducible Measurements of Right Ventricular Function in Daily Practice
Eui-Young Choi
J Cardiovasc Ultrasound. 2014;22(3):111-112. doi: 10.4250/jcu.2014.22.3.111.Strain Analysis of the Right Ventricle Using Two-dimensional Echocardiography
Ju-Hee Lee, Jae-Hyeong Park
J Cardiovasc Imaging. 2018;26(3):111-124. doi: 10.4250/jcvi.2018.26.e11.Assessment of Right Ventricular Function in Pulmonary Hypertension with Multimodality Imaging
Hye Sun Seo, Heon Lee
J Cardiovasc Imaging. 2018;26(4):189-200. doi: 10.4250/jcvi.2018.26.e28.
Reference
-
1. Di Salvo TG, Mathier M, Semigran MJ, Dec GW. Preserved right ventricular ejection fraction predicts exercise capacity and survival in advanced heart failure. J Am Coll Cardiol. 1995; 25:1143–1153.
Article2. Juillière Y, Barbier G, Feldmann L, Grentzinger A, Danchin N, Cherrier F. Additional predictive value of both left and right ventricular ejection fractions on long-term survival in idiopathic dilated cardiomyopathy. Eur Heart J. 1997; 18:276–280.
Article3. de Groote P, Millaire A, Foucher-Hossein C, Nugue O, Marchandise X, Ducloux G, Lablanche JM. Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol. 1998; 32:948–954.
Article4. Zornoff LA, Skali H, Pfeffer MA, St John Sutton M, Rouleau JL, Lamas GA, Plappert T, Rouleau JR, Moyé LA, Lewis SJ, Braunwald E, Solomon SD. SAVE Investigators. Right ventricular dysfunction and risk of heart failure and mortality after myocardial infarction. J Am Coll Cardiol. 2002; 39:1450–1455.
Article5. Oldershaw P. Assessment of right ventricular function and its role in clinical practice. Br Heart J. 1992; 68:12–15.
Article6. Tandri H, Daya SK, Nasir K, Bomma C, Lima JA, Calkins H, Bluemke DA. Normal reference values for the adult right ventricle by magnetic resonance imaging. Am J Cardiol. 2006; 98:1660–1664.
Article7. Mannaerts HF, van der Heide JA, Kamp O, Stoel MG, Twisk J, Visser CA. Early identification of left ventricular remodelling after myocardial infarction, assessed by transthoracic 3D echocardiography. Eur Heart J. 2004; 25:680–687.
Article8. Kjaergaard J, Petersen CL, Kjaer A, Schaadt BK, Oh JK, Hassager C. Evaluation of right ventricular volume and function by 2D and 3D echocardiography compared to MRI. Eur J Echocardiogr. 2006; 7:430–438.
Article9. Jamal F, Bergerot C, Argaud L, Loufouat J, Ovize M. Longitudinal strain quantitates regional right ventricular contractile function. Am J Physiol Heart Circ Physiol. 2003; 285:H2842–H2847.
Article10. Pirat B, McCulloch ML, Zoghbi WA. Evaluation of global and regional right ventricular systolic function in patients with pulmonary hypertension using a novel speckle tracking method. Am J Cardiol. 2006; 98:699–704.
Article11. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713. quiz 786-8.
Article12. Abbas AE, Fortuin FD, Schiller NB, Appleton CP, Moreno CA, Lester SJ. A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol. 2003; 41:1021–1027.
Article13. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982; 143:29–36.
Article14. Biancari F, Vasques F, Mikkola R, Martin M, Lahtinen J, Heikkinen J. Validation of EuroSCORE II in patients undergoing coronary artery bypass surgery. Ann Thorac Surg. 2012; 93:1930–1935.
Article15. Risk stratification and survival after myocardial infarction. N Engl J Med. 1983; 309:331–336.16. Kaul S, Tei C, Hopkins JM, Shah PM. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J. 1984; 107:526–531.
Article17. Schenk P, Globits S, Koller J, Brunner C, Artemiou O, Klepetko W, Burghuber OC. Accuracy of echocardiographic right ventricular parameters in patients with different end-stage lung diseases prior to lung transplantation. J Heart Lung Transplant. 2000; 19:145–154.
Article18. Hinderliter AL, Willis PW 4th, Long WA, Clarke WR, Ralph D, Caldwell EJ, Williams W, Ettinger NA, Hill NS, Summer WR, de Boisblanc B, Koch G, Li S, Clayton LM, Jöbsis MM, Crow JW. PPH Study Group. Frequency and severity of tricuspid regurgitation determined by Doppler echocardiography in primary pulmonary hypertension. Am J Cardiol. 2003; 91:1033–1037. A9
Article19. Beygui F, Furber A, Delépine S, Helft G, Metzger JP, Geslin P, Le Jeune JJ. Routine breath-hold gradient echo MRI-derived right ventricular mass, volumes and function: accuracy, reproducibility and coherence study. Int J Cardiovasc Imaging. 2004; 20:509–516.
Article20. Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennell DJ. Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J. 2004; 147:218–223.
Article21. Bleeker GB, Steendijk P, Holman ER, Yu CM, Breithardt OA, Kaandorp TA, Schalij MJ, van der Wall EE, Nihoyannopoulos P, Bax JJ. Assessing right ventricular function: the role of echocardiography and complementary technologies. Heart. 2006; 92:Suppl 1. i19–i26.
Article22. Amundsen BH, Helle-Valle T, Edvardsen T, Torp H, Crosby J, Lyseggen E, Støylen A, Ihlen H, Lima JA, Smiseth OA, Slørdahl SA. Noninvasive myocardial strain measurement by speckle tracking echocardiography: validation against sonomicrometry and tagged magnetic resonance imaging. J Am Coll Cardiol. 2006; 47:789–793.
Article23. Toyoda T, Baba H, Akasaka T, Akiyama M, Neishi Y, Tomita J, Sukmawan R, Koyama Y, Watanabe N, Tamano S, Shinomura R, Komuro I, Yoshida K. Assessment of regional myocardial strain by a novel automated tracking system from digital image files. J Am Soc Echocardiogr. 2004; 17:1234–1238.
Article24. Stanton T, Leano R, Marwick TH. Prediction of all-cause mortality from global longitudinal speckle strain: comparison with ejection fraction and wall motion scoring. Circ Cardiovasc Imaging. 2009; 2:356–364.
Article25. Verhaert D, Mullens W, Borowski A, Popović ZB, Curtin RJ, Thomas JD, Tang WH. Right ventricular response to intensive medical therapy in advanced decompensated heart failure. Circ Heart Fail. 2010; 3:340–346.
Article26. Puwanant S, Park M, Popović ZB, Tang WH, Farha S, George D, Sharp J, Puntawangkoon J, Loyd JE, Erzurum SC, Thomas JD. Ventricular geometry, strain, and rotational mechanics in pulmonary hypertension. Circulation. 2010; 121:259–266.
Article27. Cresci SG, Goldstein JA. Hemodynamic manifestations of ischemic right heart dysfunction. Cathet Cardiovasc Diagn. 1992; 27:28–33. discussion 33-4.
Article28. Popović ZB, Grimm RA, Ahmad A, Agler D, Favia M, Dan G, Lim P, Casas F, Greenberg NL, Thomas JD. Longitudinal rotation: an unrecognised motion pattern in patients with dilated cardiomyopathy. Heart. 2008; 94:e11.
Article29. Motoki H, Dahiya A, Bhargava M, Wazni OM, Saliba WI, Marwick TH, Klein AL. Assessment of left atrial mechanics in patients with atrial fibrillation: comparison between two-dimensional speckle-based strain and velocity vector imaging. J Am Soc Echocardiogr. 2012; 25:428–435.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Principles and Clinical Applications of Feature-Tracking Cardiac Magnetic Resonance Imaging: A Literature Review
- Cardiac Strain Analysis Using Cine Magnetic Resonance Imaging and Computed Tomography
- Prognostic value of left ventricular apical four-chamber longitudinal strain after heart valve surgery in real-world practice
- Evaluation of the left venticular systolic function with the measurement of global longitudinal strain by Speckle tracking echocardiography in anaphylaxis
- Strain Analysis of the Right Ventricle Using Two-dimensional Echocardiography