J Cardiovasc Imaging.
2018 Sep;26(3):111-124. 10.4250/jcvi.2018.26.e11.
Strain Analysis of the Right Ventricle Using Two-dimensional Echocardiography
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea.
- 2Department of Cardiology in Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea. jaehpark@cnu.ac.kr
- KMID: 2429852
- DOI: http://doi.org/10.4250/jcvi.2018.26.e11
Abstract
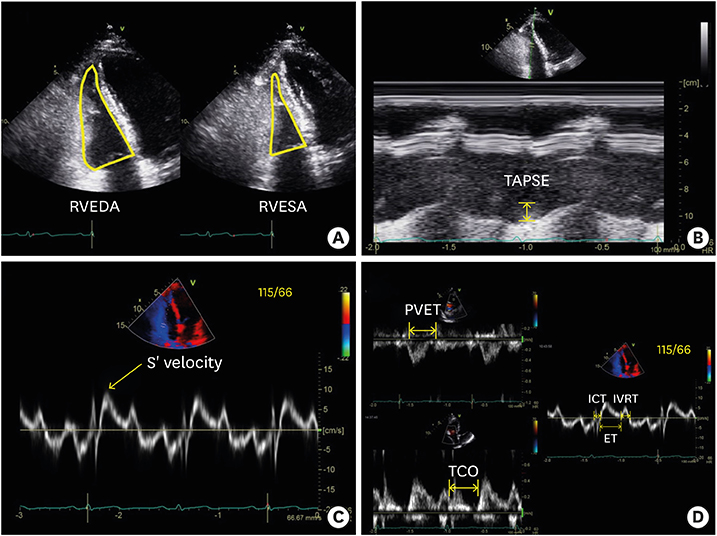
- Right ventricular (RV) systolic dysfunction has been identified as an independent prognostic marker of many cardiovascular diseases. However, there are problems in measuring RV systolic function objectively and identification of RV dysfunction using conventional echocardiography. Strain echocardiography is a new imaging modality to measure myocardial deformation. It can measure intrinsic myocardial function and has been used to measure regional and global left ventricular (LV) function. Although the RV has different morphologic characteristics than the LV, strain analysis of the RV is feasible. After strain echocardiography was introduced to measure RV systolic function, it became more popular and was incorporated into recent echocardiographic guidelines. Recent studies showed that RV global longitudinal strain (RVGLS) can be used as an objective index of RV systolic function with prognostic significance. In this review, we discuss RVGLS measurement, normal reference values, and the clinical importance of RVGLS.
Figure
Cited by 3 articles
-
Two-dimensional Echocardiographic Assessment of Myocardial Strain: Important Echocardiographic Parameter Readily Useful in Clinical Field
Jae-Hyeong Park
Korean Circ J. 2019;49(10):908-931. doi: 10.4070/kcj.2019.0200.Assessment of Right Ventricular Function in Pulmonary Hypertension with Multimodality Imaging
Hye Sun Seo, Heon Lee
J Cardiovasc Imaging. 2018;26(4):189-200. doi: 10.4250/jcvi.2018.26.e28.Echocardiographic Screening Methods for Pulmonary Hypertension: A Practical Review
Albert Youngwoo Jang, Mi-Seung Shin
J Cardiovasc Imaging. 2020;28(1):1-9. doi: 10.4250/jcvi.2019.0104.
Reference
-
1. de Groote P, Millaire A, Foucher-Hossein C, et al. Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol. 1998; 32:948–954.
Article2. Ghio S, Gavazzi A, Campana C, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001; 37:183–188.
Article3. Forfia PR, Fisher MR, Mathai SC, et al. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med. 2006; 174:1034–1041.
Article4. Tadic M. Multimodality evaluation of the right ventricle: an updated review. Clin Cardiol. 2015; 38:770–776.
Article5. Pirat B, McCulloch ML, Zoghbi WA. Evaluation of global and regional right ventricular systolic function in patients with pulmonary hypertension using a novel speckle tracking method. Am J Cardiol. 2006; 98:699–704.
Article6. Cho GY, Marwick TH, Kim HS, Kim MK, Hong KS, Oh DJ. Global 2-dimensional strain as a new prognosticator in patients with heart failure. J Am Coll Cardiol. 2009; 54:618–624.
Article7. Choi SW, Park JH, Sun BJ, et al. Impaired two-dimensional global longitudinal strain of left ventricle predicts adverse long-term clinical outcomes in patients with acute myocardial infarction. Int J Cardiol. 2015; 196:165–167.
Article8. Sarvari SI, Haugaa KH, Anfinsen OG, et al. Right ventricular mechanical dispersion is related to malignant arrhythmias: a study of patients with arrhythmogenic right ventricular cardiomyopathy and subclinical right ventricular dysfunction. Eur Heart J. 2011; 32:1089–1096.
Article9. Thomas JD, Popović ZB. Assessment of left ventricular function by cardiac ultrasound. J Am Coll Cardiol. 2006; 48:2012–2025.
Article10. Geyer H, Caracciolo G, Abe H, et al. Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr. 2010; 23:351–369.
Article11. Nahum J, Bensaid A, Dussault C, et al. Impact of longitudinal myocardial deformation on the prognosis of chronic heart failure patients. Circ Cardiovasc Imaging. 2010; 3:249–256.
Article12. Smiseth OA, Torp H, Opdahl A, Haugaa KH, Urheim S. Myocardial strain imaging: how useful is it in clinical decision making? Eur Heart J. 2016; 37:1196–1207.
Article13. Negishi K, Negishi T, Hare JL, Haluska BA, Plana JC, Marwick TH. Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr. 2013; 26:493–498.
Article14. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14.
Article15. Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: Anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008; 117:1436–1448.16. Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713.17. Potter E, Marwick TH. Assessment of left ventricular function by echocardiography: the case for routinely adding global longitudinal strain to ejection fraction. JACC Cardiovasc Imaging. 2018; 11:260–274.18. Jamal F, Bergerot C, Argaud L, Loufouat J, Ovize M. Longitudinal strain quantitates regional right ventricular contractile function. Am J Physiol Heart Circ Physiol. 2003; 285:H2842–7.
Article19. Lu KJ, Chen JX, Profitis K, et al. Right ventricular global longitudinal strain is an independent predictor of right ventricular function: a multimodality study of cardiac magnetic resonance imaging, real time three-dimensional echocardiography and speckle tracking echocardiography. Echocardiography. 2015; 32:966–974.
Article20. Wang J, Prakasa K, Bomma C, et al. Comparison of novel echocardiographic parameters of right ventricular function with ejection fraction by cardiac magnetic resonance. J Am Soc Echocardiogr. 2007; 20:1058–1064.
Article21. Vizzardi E, Bonadei I, Sciatti E, et al. Quantitative analysis of right ventricular (RV) function with echocardiography in chronic heart failure with no or mild RV dysfunction: comparison with cardiac magnetic resonance imaging. J Ultrasound Med. 2015; 34:247–255.22. Freed BH, Tsang W, Bhave NM, et al. Right ventricular strain in pulmonary arterial hypertension: a 2D echocardiography and cardiac magnetic resonance study. Echocardiography. 2015; 32:257–263.
Article23. Ho SY, Nihoyannopoulos P. Anatomy, echocardiography, and normal right ventricular dimensions. Heart. 2006; 92:Suppl 1. i2–13.
Article24. Park JH, Negishi K, Kwon DH, Popovic ZB, Grimm RA, Marwick TH. Validation of global longitudinal strain and strain rate as reliable markers of right ventricular dysfunction: comparison with cardiac magnetic resonance and outcome. J Cardiovasc Ultrasound. 2014; 22:113.
Article25. Focardi M, Cameli M, Carbone SF, et al. Traditional and innovative echocardiographic parameters for the analysis of right ventricular performance in comparison with cardiac magnetic resonance. Eur Heart J Cardiovasc Imaging. 2015; 16:47–52.
Article26. Lemarié J, Huttin O, Girerd N, et al. Usefulness of speckle-tracking imaging for right ventricular assessment after acute myocardial infarction: a magnetic resonance imaging/echocardiographic comparison within the relation between aldosterone and cardiac remodeling after myocardial infarction Study. J Am Soc Echocardiogr. 2015; 28:818–827.e4.
Article27. Park SJ, Park JH, Lee HS, et al. Impaired RV global longitudinal strain is associated with poor long-term clinical outcomes in patients with acute inferior STEMI. JACC Cardiovasc Imaging. 2015; 8:161–169.28. Meris A, Faletra F, Conca C, et al. Timing and magnitude of regional right ventricular function: a speckle tracking-derived strain study of normal subjects and patients with right ventricular dysfunction. J Am Soc Echocardiogr. 2010; 23:823–831.
Article29. Cho GY, Chan J, Leano R, Strudwick M, Marwick TH. Comparison of two-dimensional speckle and tissue velocity based strain and validation with harmonic phase magnetic resonance imaging. Am J Cardiol. 2006; 97:1661–1666.
Article30. Fine NM, Shah AA, Han IY, et al. Left and right ventricular strain and strain rate measurement in normal adults using velocity vector imaging: an assessment of reference values and intersystem agreement. Int J Cardiovasc Imaging. 2013; 29:571–580.
Article31. Longobardo L, Suma V, Jain R, et al. Role of two-dimensional speckle-tracking echocardiography strain in the assessment of right ventricular systolic function and comparison with conventional parameters. J Am Soc Echocardiogr. 2017; 30:937–946.e6.32. Muraru D, Onciul S, Peluso D, et al. Sex- and method-specific reference values for right ventricular strain by 2-dimensional speckle-tracking echocardiography. Circ Cardiovasc Imaging. 2016; 9:e003866.
Article33. Park JH, Choi JO, Park SW, et al. Normal references of right ventricular strain values by two-dimensional strain echocardiography according to the age and gender. Int J Cardiovasc Imaging. 2018; 34:177–183.
Article34. Fine NM, Chen L, Bastiansen PM, et al. Reference values for right ventricular strain in patients without cardiopulmonary disease: a prospective evaluation and meta-analysis. Echocardiography. 2015; 32:787–796.
Article35. Zornoff LA, Skali H, Pfeffer MA, et al. Right ventricular dysfunction and risk of heart failure and mortality after myocardial infarction. J Am Coll Cardiol. 2002; 39:1450–1455.
Article36. Rajagopalan N, Simon MA, Shah H, Mathier MA, López-Candales A. Utility of right ventricular tissue Doppler imaging: correlation with right heart catheterization. Echocardiography. 2008; 25:706–711.
Article37. Puwanant S, Park M, Popović ZB, et al. Ventricular geometry, strain, and rotational mechanics in pulmonary hypertension. Circulation. 2010; 121:259–266.
Article38. Park JH, Park YS, Park SJ, et al. Midventricular peak systolic strain and Tei index of the right ventricle correlated with decreased right ventricular systolic function in patients with acute pulmonary thromboembolism. Int J Cardiol. 2008; 125:319–324.
Article39. Park JH, Park YS, Kim YJ, et al. Differentiation between acute and chronic cor pulmonales with midventricular systolic strain of the right ventricle in the emergency department. Heart Vessels. 2011; 26:435–439.
Article40. Ikeda S, Tsuneto A, Kojima S, et al. Longitudinal strain of right ventricular free wall by 2-dimensional speckle-tracking echocardiography is useful for detecting pulmonary hypertension. Life Sci. 2014; 111:12–17.
Article41. Park JH, Kusunose K, Kwon DH, et al. Relationship between right ventricular longitudinal strain, invasive hemodynamics, and functional assessment in pulmonary arterial hypertension. Korean Circ J. 2015; 45:398–407.
Article42. Motoji Y, Tanaka H, Fukuda Y, et al. Efficacy of right ventricular free-wall longitudinal speckle-tracking strain for predicting long-term outcome in patients with pulmonary hypertension. Circ J. 2013; 77:756–763.
Article43. Fukuda Y, Tanaka H, Sugiyama D, et al. Utility of right ventricular free wall speckle-tracking strain for evaluation of right ventricular performance in patients with pulmonary hypertension. J Am Soc Echocardiogr. 2011; 24:1101–1108.
Article44. Fine NM, Chen L, Bastiansen PM, et al. Outcome prediction by quantitative right ventricular function assessment in 575 subjects evaluated for pulmonary hypertension. Circ Cardiovasc Imaging. 2013; 6:711–721.
Article45. Lee JH, Park JH, Park KI, et al. A comparison of different techniques of two-dimensional speckle-tracking strain measurements of right ventricular systolic function in patients with acute pulmonary embolism. J Cardiovasc Ultrasound. 2014; 22:65–71.
Article46. D'Andrea A, Stanziola A, D'Alto M, et al. Right ventricular strain: An independent predictor of survival in idiopathic pulmonary fibrosis. Int J Cardiol. 2016; 222:908–910.47. Mukherjee M, Chung SE, Ton VK, et al. Unique abnormalities in right ventricular longitudinal strain in systemic sclerosis patients. Circ Cardiovasc Imaging. 2016; 9:pii: e003792.
Article48. Holman WL, Kormos RL, Naftel DC, et al. Predictors of death and transplant in patients with a mechanical circulatory support device: a multi-institutional study. J Heart Lung Transplant. 2009; 28:44–50.
Article49. Argiriou M, Kolokotron SM, Sakellaridis T, et al. Right heart failure post left ventricular assist device implantation. J Thorac Dis. 2014; 6:Suppl 1. S52–S59.50. Vivo RP, Cordero-Reyes AM, Qamar U, et al. Increased right-to-left ventricle diameter ratio is a strong predictor of right ventricular failure after left ventricular assist device. J Heart Lung Transplant. 2013; 32:792–799.
Article51. Grant AD, Smedira NG, Starling RC, Marwick TH. Independent and incremental role of quantitative right ventricular evaluation for the prediction of right ventricular failure after left ventricular assist device implantation. J Am Coll Cardiol. 2012; 60:521–528.
Article52. Goldraich L, Kawajiri H, Foroutan F, et al. Tricuspid valve annular dilation as a predictor of right ventricular failure after implantation of a left ventricular assist device. J Card Surg. 2016; 31:110–116.
Article53. Cameli M, Lisi M, Righini FM, et al. Right ventricular longitudinal strain correlates well with right ventricular stroke work index in patients with advanced heart failure referred for heart transplantation. J Card Fail. 2012; 18:208–215.
Article54. Lisi M, Cameli M, Righini FM, et al. RV longitudinal deformation correlates with myocardial fibrosis in patients with end-stage heart failure. JACC Cardiovasc Imaging. 2015; 8:514–522.55. Morris DA, Krisper M, Nakatani S, et al. Normal range and usefulness of right ventricular systolic strain to detect subtle right ventricular systolic abnormalities in patients with heart failure: a multicentre study. Eur Heart J Cardiovasc Imaging. 2017; 18:212–223.
Article56. Teske AJ, Cox MG, Te Riele AS, et al. Early detection of regional functional abnormalities in asymptomatic ARVD/C gene carriers. J Am Soc Echocardiogr. 2012; 25:997–1006.
Article57. Vitarelli A, Cortes Morichetti M, Capotosto L, et al. Utility of strain echocardiography at rest and after stress testing in arrhythmogenic right ventricular dysplasia. Am J Cardiol. 2013; 111:1344–1350.
Article58. Aneq MÅ, Engvall J, Brudin L, Nylander E. Evaluation of right and left ventricular function using speckle tracking echocardiography in patients with arrhythmogenic right ventricular cardiomyopathy and their first degree relatives. Cardiovasc Ultrasound. 2012; 10:37.
Article59. D'Andrea A, Caso P, Bossone E, et al. Right ventricular myocardial involvement in either physiological or pathological left ventricular hypertrophy: an ultrasound speckle-tracking two-dimensional strain analysis. Eur J Echocardiogr. 2010; 11:492–500.60. D'Andrea A, Limongelli G, Baldini L, et al. Exercise speckle-tracking strain imaging demonstrates impaired right ventricular contractile reserve in hypertrophic cardiomyopathy. Int J Cardiol. 2017; 227:209–216.61. Negishi K, Lucas S, Negishi T, Hamilton J, Marwick TH. What is the primary source of discordance in strain measurement between vendors: imaging or analysis? Ultrasound Med Biol. 2013; 39:714–720.
Article62. Park JH, Kusunose K, Motoki H, et al. Assessment of right ventricular longitudinal strain in patients with ischemic cardiomyopathy: head-to-head comparison between two-dimensional speckle-based strain and velocity vector imaging using volumetric assessment by cardiac magnetic resonance as a “gold standard”. Echocardiography. 2015; 32:956–965.63. Yang H, Marwick TH, Fukuda N, et al. Improvement in strain concordance between two major vendors after the strain standardization initiative. J Am Soc Echocardiogr. 2015; 28:642–8.e7.
Article64. Badano LP, Kolias TJ, Muraru D, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2018; 19:591–600.
Article65. van der Zwaan HB, Geleijnse ML, Soliman OI, et al. Test-retest variability of volumetric right ventricular measurements using real-time three-dimensional echocardiography. J Am Soc Echocardiogr. 2011; 24:671–679.
Article66. Schwarz K, Singh S, Dawson D, Frenneaux MP. Right ventricular function in left ventricular disease: pathophysiology and implications. Heart Lung Circ. 2013; 22:507–511.
Article67. Belenkie I, Horne SG, Dani R, Smith ER, Tyberg JV. Effects of aortic constriction during experimental acute right ventricular pressure loading. Further insights into diastolic and systolic ventricular interaction. Circulation. 1995; 92:546–554.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two-dimensional Echocardiographic Assessment of Myocardial Strain: Important Echocardiographic Parameter Readily Useful in Clinical Field
- 2-Dimensional Strain Analysis of Regional Change in Right Ventricular Function after Treadmill Exercise
- The Usefulness of 4D Echocardiographic Modality for Assessing RV Affection in Uncontrolled Hypertensive Patients
- Assessment of Right Ventricular Structure and Function in Pulmonary Hypertension
- Horseshoe-like Shaped Atrial Septal Defects Confirmed on Three-Dimensional Transesophageal Echocardiography