J Korean Neurosurg Soc.
2014 Oct;56(4):348-352. 10.3340/jkns.2014.56.4.348.
Endovascular Treatment of Symptomatic High-Flow Vertebral Arteriovenous Fistula as a Complication after C1 Screw Insertion
- Affiliations
-
- 1Department of Neurosurgery, Inha University School of Medicine and Hospital, Incheon, Korea. dro3@nate.com
- KMID: 2018088
- DOI: http://doi.org/10.3340/jkns.2014.56.4.348
Abstract
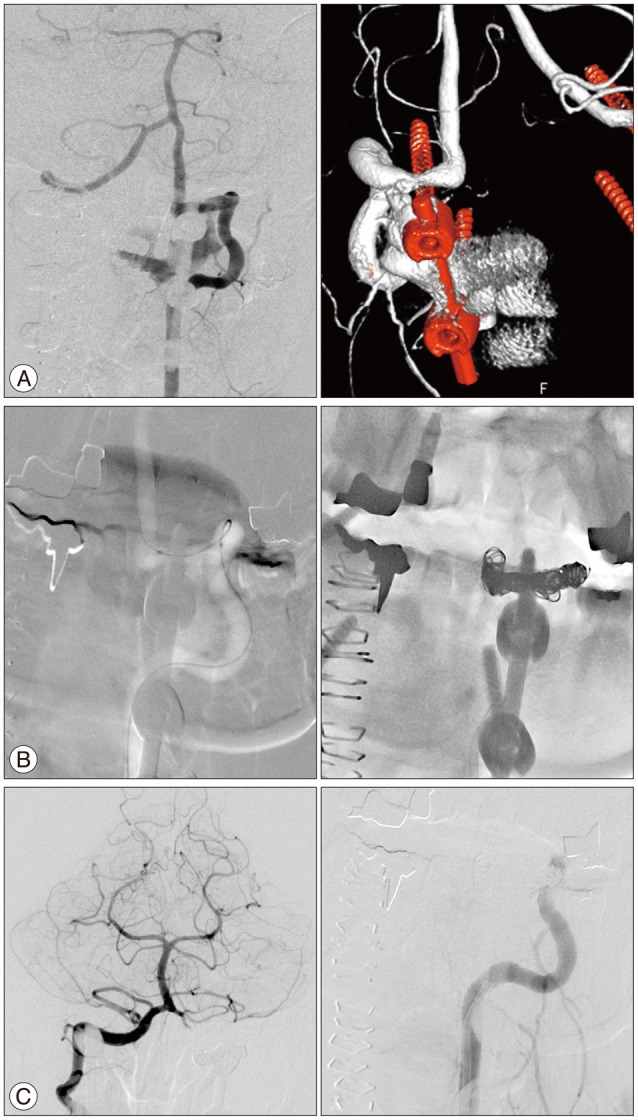
- High-flow vertebral arteriovenous fistulas (VAVF) are rare complications of cervical spine surgery and characterized by iatrogenic direct-communication of the extracranial vertebral artery (VA) to the surrounding venous plexuses. The authors describe two patients with VAVF presenting with ischemic presentation after C1 pedicle screw insertion for a treatment of C2 fracture and nontraumatic atlatoaxial subluxation. The first patient presented with drowsy consciousness with blurred vision. The diffusion MRI showed an acute infarction on bilateral cerebellum and occipital lobes. The second patient presented with pulsatile tinnitus, dysarthria and a subjective weakness and numbness of extremities. In both cases, digital subtraction angiography demonstrated high-flow direct VAVFs adjacent to C1 screws. The VAVF of the second case occurred near the left posterior inferior cerebellar artery originated from the persistent first intersegmental artery of the left VA. Both cases were successfully treated by complete occlusion of the fistulous portion and the involved segment of the left VA using endovascular coil embolization. The authors reviewed the VAVFs after the upper-cervical spine surgery including C1 screw insertion and the feasibility with the attention notes of its endovascular treatment.
MeSH Terms
Figure
Reference
-
1. Albuquerque FC, Javedan SP, McDougall CG. Endovascular management of penetrating vertebral artery injuries. J Trauma. 2002; 53:574–580. PMID: 12352501.
Article2. Briganti F, Tortora F, Elefante A, Volpe A, Bruno MC, Panagiotopoulos K. An unusual case of vertebral arteriovenous fistula treated with electrodetachable coil embolization. Minim Invasive Neurosurg. 2004; 47:386–388. PMID: 15674760.
Article3. Coric D, Branch CL Jr, Wilson JA, Robinson JC. Arteriovenous fistula as a complication of C1-2 transarticular screw fixation. Case report and review of the literature. J Neurosurg. 1996; 85:340–343. PMID: 8755766.
Article4. Crowley RW, Medel R, Dumont AS. Traumatic high flow vertebral-venous fistula presenting with delayed ischemic stroke: endovascular management with detachable coils and Amplatzer Vascular Plugs. Neurosurg Focus. 2009; 26:E5. PMID: 19249961.
Article5. Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR Am J Roentgenol. 1988; 150:405–412. PMID: 3257333.
Article6. Herrera DA, Vargas SA, Dublin AB. Endovascular treatment of traumatic injuries of the vertebral artery. AJNR Am J Neuroradiol. 2008; 29:1585–1589. PMID: 18499790.
Article7. Heuer GG, Gabel BC, Bhowmick DA, Stiefel MF, Hurst RW, Schuster JM. Symptomatic high-flow arteriovenous fistula after a C-2 fracture. Case report. J Neurosurg Spine. 2008; 8:381–384. PMID: 18377324.8. John S, Jaffari N, Lu M, Hussain MS, Hui F. Spontaneous vertebral arteriovenous fistula causing cervical myelopathy and acute ischemic strokes treated by endovascular balloon-assisted coiling and Onyx embolization. J Clin Neurosci. 2014; 21:167–170. PMID: 23972561.
Article9. Li F, Song X, Liu C, Liu B, Zheng Y. Endovascular stent-graft treatment for a traumatic vertebrovertebral arteriovenous fistula with pseudoaneurysm. Ann Vasc Surg. 2014; 28:489. PMID: 24200138.
Article10. Luo CB, Teng MM, Chang FC, Chang CY. Endovascular treatment of intracranial high-flow arteriovenous fistulas by Guglielmi detachable coils. J Chin Med Assoc. 2006; 69:80–85. PMID: 16570575.
Article11. Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997; 86:961–968. PMID: 9171174.
Article12. Neo M, Fujibayashi S, Miyata M, Takemoto M, Nakamura T. Vertebral artery injury during cervical spine surgery: a survey of more than 5600 operations. Spine (Phila Pa 1976). 2008; 33:779–785. PMID: 18379405.13. Peng CW, Chou BT, Bendo JA, Spivak JM. Vertebral artery injury in cervical spine surgery: anatomical considerations, management, and preventive measures. Spine J. 2009; 9:70–76. PMID: 18504163.
Article14. Tenjin H, Kimura S, Sugawa N. Coil embolization of vertebro-vertebral arteriovenous fistula: a case report. Surg Neurol. 2005; 63:80–83. discussion 83. PMID: 15639536.
Article15. Uchino A, Saito N, Watadani T, Okada Y, Kozawa E, Nishi N, et al. Vertebral artery variations at the C1-2 level diagnosed by magnetic resonance angiography. Neuroradiology. 2012; 54:19–23. PMID: 21340577.
Article16. Umebayashi D, Hara M, Nakajima Y, Nishimura Y, Wakabayashi T. Posterior fixation for atlantoaxial subluxation in a case with complex anomaly of persistent first intersegmental artery and assimilation in the C1 vertebra. Neurol Med Chir (Tokyo). 2013; 53:882–886. PMID: 24097089.
Article17. Wakao N, Takeuchi M, Nishimura M, Riew KD, Kamiya M, Hirasawa A, et al. Vertebral artery variations and osseous anomaly at the C1-2 level diagnosed by 3D CT angiography in normal subjects. Neuroradiology. 2014; 56:843–849. PMID: 25001076.
Article18. Wang Q, Song D, Chen G. Endovascular treatment of high-flow cervical direct vertebro-vertebral arteriovenous fistula with detachable coils and Onyx liquid embolic agent. Acta Neurochir (Wien). 2011; 153:347–352. PMID: 21058042.
Article19. Wright NM, Lauryssen C. Vertebral artery injury in C1-2 transarticular screw fixation: results of a survey of the AANS/CNS section on disorders of the spine and peripheral nerves. American Association of NeurologiNeurological Surgeons/Congress of Neurological Surgeons. J Neurosurg. 1998; 88:634–640. PMID: 9525707.
Article20. Yamazaki M, Okawa A, Furuya T, Sakuma T, Takahashi H, Kato K, et al. Anomalous vertebral arteries in the extra- and intraosseous regions of the craniovertebral junction visualized by 3-dimensional computed tomographic angiography: analysis of 100 consecutive surgical cases and review of the literature. Spine (Phila Pa 1976). 2012; 37:E1389–E1397. PMID: 22825480.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extracranial vertebral arteriovenous fistula presenting as an osteolytic lesion of the axis: Case report
- Endovascular Treatment for Spontaneous Vertebral Arteriovenous Fistula in Neurofibromatosis Type 1: A Case Report
- Endovascular Stent-Graft Treatment of a Traumatic Vertebral Artery Pseudoaneurysm and Vertebrojugular Fistula
- Cervical spinal extradural arteriovenous fistula successfully treated using transarterial balloon-assisted coil embolization
- Coil Embolization of High-flow Pial Arteriovenous Fistula and Management of Hyperperfusion Syndrome: a Case Report