Korean J Urol.
2007 Mar;48(3):304-309. 10.4111/kju.2007.48.3.304.
Detection of Cryptic Microorganisms in Patients with Chronic Prostatitis by Multiplex Polymerase Chain Reaction
- Affiliations
-
- 1Department of Urology, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Laboratory Medicine, Chung-Ang University College of Medicine, Seoul, Korea. cpworld@cau.ac.kr
- KMID: 1997129
- DOI: http://doi.org/10.4111/kju.2007.48.3.304
Abstract
- PURPOSE
Chronic prostatitis frequently occurs in men of all ages. Recent studies suggest that fastidious microorganisms may play a role in chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). The aim of this study was to evaluate the usefulness and significance of multiplex polymerase chain reaction (PCR) in the diagnosis of CP/CPPS.
MATERIALS AND METHODS
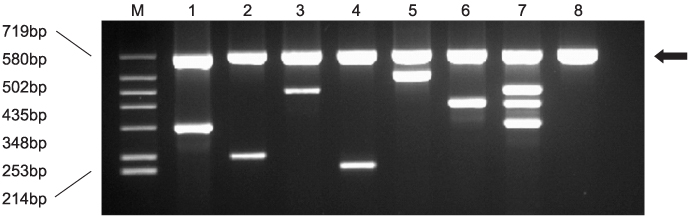
First voided urine (FVU) and/or expressed prostatic secretions (EPS) were collected from 92 patients. Multiplex PCR, using Dual Specificity Oligo (DSO(TM)) primers, was used to test for Chlamydia trachomatis (CT), Mycoplasma genitalium (MG), Mycoplasma hominis (MH), Neisseria gonorrhoeae (NG), Trichomonas vaginalis (TV) and Ureaplasma urealyticum (UU).
RESULTS
Multiplex PCR can be easily analyzed via visual comparison. Nine (39.1%) of the 23 CP/CPPS IIIa and 12 (17.4%) of the 69 IIIb patients had positive multiplex PCR, with a total of 27 microorganisms isolated, including CT, MH, MG, UU, TV and NG in 9, 7, 4, 4, 2 and 1 case, respectively. Co-infections with 2 or 3 organisms occurred in 5 cases. For the samples collected from 32 patients for both FVU and EPS, 68.7% gave the same results.
CONCLUSIONS
Multiplex PCR, using DSO(TM) primers, can be useful for the simple detection of fastidious microorganisms in CP/CPPS. To achieve reliable results with multiplex PCR, feasible guidelines and standardization are of major importance. Further studies will be required to define the usefulness of molecular tests for CP/CPPS in clinical practice.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
The Prevalence of Vaginal Microorganisms in Pregnant Women with Preterm Labor and Preterm Birth
Seong Jin Choi, Soon Deok Park, In Ho Jang, Young Uh, Anna Lee
Ann Lab Med. 2012;32(3):194-200. doi: 10.3343/alm.2012.32.3.194.Prevalence of
Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium, Ureaplasma urealyticum in Chronic Prostatitis Category IIIa and IIIb Patients Using Polymerase Chain Reaction
In-Chang Cho, Yoo Seok Kim, Sung Bin Kim, Soon Ki Kim, Gyeong In Lee, Seung Ki Min
Korean J Urogenit Tract Infect Inflamm. 2013;8(2):102-108. doi: 10.14777/kjutii.2013.8.2.102.
Reference
-
1. Domingue GJ Sr, Hellstrom WJ. Prostatitis. Clin Microbiol Rev. 1998. 11:604–613.2. Collins MM, Stafford RS, O'Leary MP, Barry MJ. How common is prostatitis? A national survey of physician visits. J Urol. 1998. 159:1224–1228.3. Drach GW, Fair WR, Meares EM, Stamey TA. Classification of benign diseases associated with prostatic pain: prostatitis or prostatodynia? J Urol. 1978. 120:266.4. Krieger NJ, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999. 282:236–237.5. de la Rosette JJ, Hubregtse MR, Meuleman EJ, Stolk-Engelaar MV, Debruyne FM. Diagnosis and treatment of 409 patients with prostatitis syndromes. Urology. 1993. 41:301–307.6. Roberts RO, Lieber MM, Bostwick DG, Jacobsen SJ. A review of clinical and pathological prostatitis syndromes. Urology. 1997. 49:809–821.7. Berger RE, Krieger JN, Rothman I, Muller CH, Hillier SL. Bacteria in the prostate tissue of men with idiopathic prostatic inflammation. J Urol. 1997. 157:863–865.8. Ponniah S, Arah I, Alexander RB. PSA is a candidate self-antigen in autoimmune chronic prostatitis/chronic pelvic pain syndrome. Prostate. 2000. 44:49–54.9. Zermann DH, Ishigooka M, Doggweiler R, Schmidt RA. Neurourological insights into the etiology of genitourinary pain in men. J Urol. 1999. 161:903–908.10. Mehik A, Hellstrom P, Sarpola A, Lukkarinen O, Jarvelin MR. Fears, sexual disturbances and personality features in men with prostatitis: a population-based cross-sectional study in Finland. BJU Int. 2001. 88:35–38.11. Krieger JN, Riley DE. Chronic prostatitis: Charlottesville to Seattle. J Urol. 2004. 172:2557–2560.12. Ha JS, Kim SW, Cho YH. Detection of cryptic microorganism by polymerase chain reaction assay in chronic pelvic pain syndrome. Korean J Urol. 2002. 43:396–401.13. Seegene Inc.PCT/KR2006/000746. Processes using Dual Specificity Oligonucleotide and Dual Specificity Oligonucleotide. 2006.14. Elnifro EM, Ashshi AM, Cooper RJ, Klapper PE. Multiplex PCR: optimization and application in diagnostic virology. Clin Microbiol Rev. 2000. 13:559–570.15. Chamberlain JS, Gibbs RA, Ranier JE, Nguyen PN, Caskey CT. Deletion screening of the Duchenne muscular dystrophy locus via multiplex DNA amplification. Nucleic Acids Res. 1988. 16:11141–11156.16. Rithidech KN, Dunn JJ, Gordon CR. Combining multiplex and touchdown PCR to screen murine microsatellite polymorphisms. Biotechniques. 1997. 23:36–45.17. Zimmermann K, Schogl D, Plaimauer B, Mannhalter JW. Quantitative multiple competitive PCR of HIV-1 DNA in a single reaction tube. Biotechniques. 1996. 21:480–484.18. Zou S, Stansfield C, Bridge J. Identification of new influenza B virus variants by multiplex reverse transcription-PCR and the heteroduplex mobility assay. J Clin Microbiol. 1998. 36:1544–1548.19. Markoulatos P, Siafakas N, Moncany M. Multiplex polymerase chain reaction: a practical approach. J Clin Lab Anal. 2002. 16:47–51.20. Markoulatos P, Siafakas N, Katsorchis T, Moncany M. Multiplex PCR: rapid DNA cycling in a conventional thermal cycler. J Clin Lab Anal. 2003. 17:108–112.21. Stellrecht KA, Woron AM, Mishrik NG, Venezia RA. Comparison of multiplex PCR assay with culture for detection of genital mycoplasmas. J Clin Microbiol. 2004. 42:1528–1533.22. Palladino S, Pearman JW, Kay ID, Smith DW, Harnett GB, Woods M, et al. Diagnosis of Chlamydia trachomatis and Neisseria gonorrhoeae. Genitourinary infections in males by the Amplicor PCR assay of urine. Diagn Microbiol Infect Dis. 1999. 33:141–146.23. Radonjic IV, Dzamic AM, Mitrovic SM, Arsic Arsenijevic VS, Popadic DM, Kranjcic Zec IF. Diagnosis of Trichomonas vaginalis infection: the sensitivities and specificities of microscopy, culture and PCR assay. Eur J Obstet Gynecol Reprod Biol. 2006. 126:116–120.24. Skerk V, Krhen I, Schonwald S, Cajic V, Markovinovic L, Roglic S, et al. The role of unusual pathogens in prostatitis syndrome. Int J Antimicrob Agents. 2004. 24:Suppl 1. S53–S56.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Results of Microorganism Detection by Multiplex Polymerase Chain Reaction in Patients with Chronic Pelvic Pain Syndrome
- Detection of Cryptic Microorganisms by Polymerase Chain Reaction Assay in Chronic Pelvic Pain Syndrome
- The Diagnostic Values of the Polymerase Chain Reaction in Prostatitis
- Diagnostic Value of Polymerase Chain Reaction in Patients with Chronic Pelvic Pain Syndrome: using Semen as a Specimen
- Rapid Diagnosis of Duchenne Muscular Dystrophy DMD by Multiplex Polymerase Chain Reaction PCR using Uncultured Amniocytes