J Korean Med Sci.
2013 Apr;28(4):631-635. 10.3346/jkms.2013.28.4.631.
Fibrocartilaginous Intramedullary Bone Forming Tumor of the Distal Femur Mimicking Osteosarcoma
- Affiliations
-
- 1Department of Orthopaedic Surgery, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 2Institute for rare diseases and Department of Orthopaedic Surgery, Korea University Medical Center, Guro Hospital, Seoul, Korea.
- 3Department of Orthopaedic Surgery, Korea University Medical Center, Anam Hospital, Seoul, Korea. pjh1964@hanmail.net
- KMID: 1786976
- DOI: http://doi.org/10.3346/jkms.2013.28.4.631
Abstract
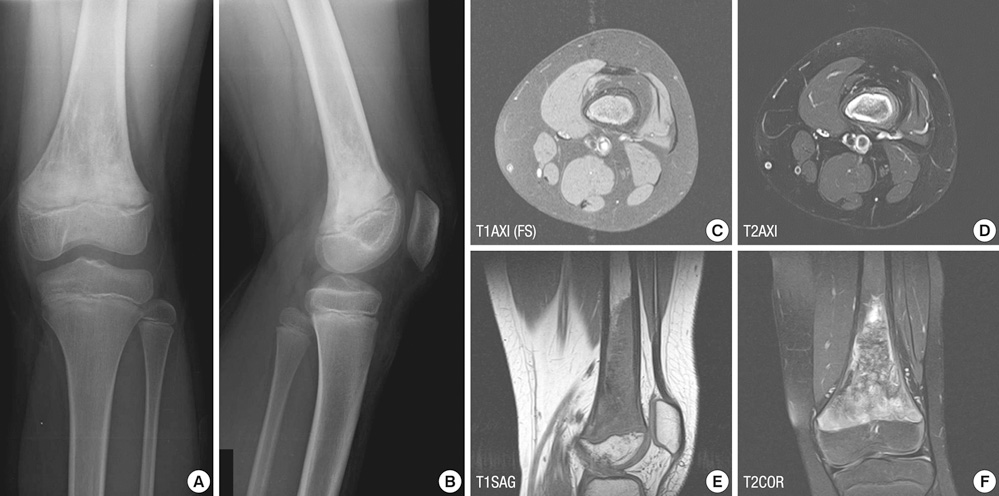
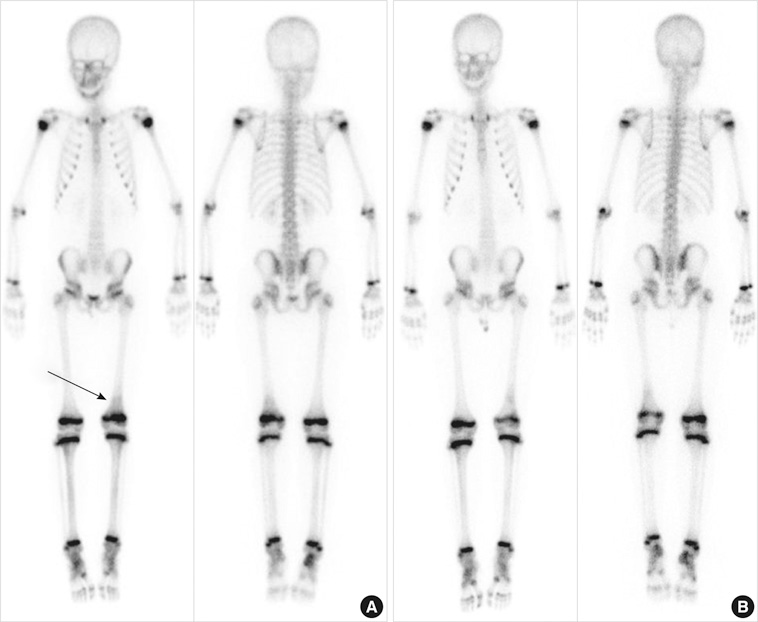
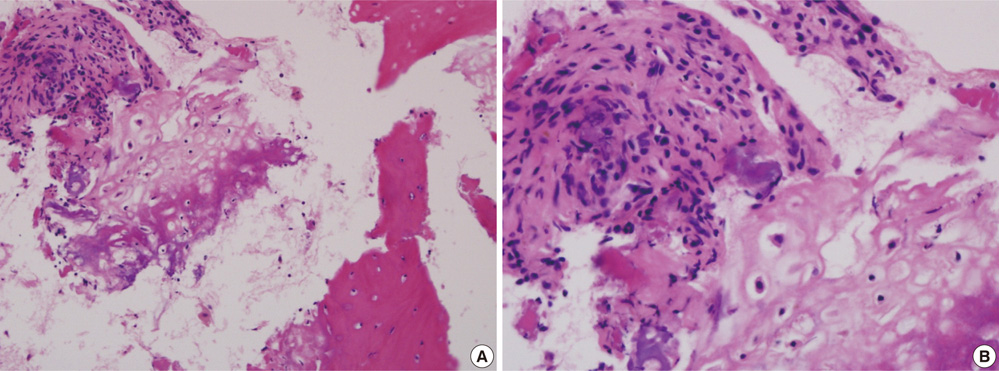
- Fibrocartilaginous dysplasia (FCD) has occasionally led to a misdiagnosis and wrong decision which can significantly alter the outcome of the patients. A 9-yr-old boy presented with pain on his left distal thigh for 6 months without any trauma history. Initial radiographs showed moth eaten both osteolytic and osteosclerotic lesions and biopsy findings showed that the lesion revealed many irregular shaped and sclerotic mature and immature bony trabeculae. Initial diagnostic suggestions were varied from the conventional osteosarcoma to low grade central osteosarcoma or benign intramedullary bone forming lesion, but close observation was done. This study demonstrated a case of unusual fibrocartilaginous intramedullary bone forming tumor mimicking osteosarcoma, so that possible misdiagnosis might be made and unnecessary extensive surgical treatment could be performed. In conclusion, the role of orthopaedic oncologist as a decision maker is very important when the diagnosis is uncertain.
MeSH Terms
Figure
Reference
-
1. Meyers PA, Gorlick R. Osteosarcoma. Pediatr Clin North Am. 1997. 44:973–989.2. Savitskaya YA, Rico-Martínez G, Linares-González LM, Delgado-Cedillo EA, Téllez-Gastelum R, Alfaro-Rodríguez AB, Redón-Tavera A, Ibarra-Ponce de León JC. Serum tumor markers in pediatric osteosarcoma: a summary review. Clin Sarcoma Res. 2012. 2:9.3. Rosenberg ZS, Lev S, Schmahmann S, Steiner GC, Beltran J, Present D. Osteosarcoma: subtle, rare, and misleading plain film features. AJR Am J Roentgenol. 1995. 165:1209–1214.4. Campanacci M, Cervellati G. Osteosarcoma: a review of 345 cases. Ital J Orthop Traumatol. 1975. 1:5–22.5. Kumar A, Varshney MK, Khan SA, Rastogi S, Safaya R. Low grade central osteosarcoma: a diagnostic dilemma. Joint Bone Spine. 2008. 75:613–615.6. Pelzmann KS, Nagel DZ, Salyer WR. Case report 114. Skeletal Radiol. 1980. 5:116–118.7. Ishida T, Dorfman HD. Massive chondroid differentiation in fibrous dysplasia of bone (fibrocartilaginous dysplasia). Am J Surg Pathol. 1993. 17:924–930.8. De Smet AA, Travers H, Neff JR. Chondrosarcoma occurring in a patient with polyostotic fibrous dysplasia. Skeletal Radiol. 1981. 7:197–201.9. Reigel DH, Larson SJ, Sances A Jr, Hoffman NE, Switala KJ. A gastric acid inhibitor of cerebral origin. Surgery. 1971. 70:161–168.10. Kyriakos M, McDonald DJ, Sundaram M. Fibrous dysplasia with cartilaginous differentiation ("fibrocartilaginous dysplasia"): a review, with an illustrative case followed for 18 years. Skeletal Radiol. 2004. 33:51–62.11. Bianco P, Riminucci M, Majolagbe A, Kuznetsov SA, Collins MT, Mankani MH, Corsi A, Bone HG, Wientroub S, Spiegel AM, et al. Mutations of the GNAS1 gene, stromal cell dysfunction, and osteomalacic changes in non-McCune-Albright fibrous dysplasia of bone. J Bone Miner Res. 2000. 15:120–128.12. Sanerkin NG, Watt I. Enchondromata with annular calcification in association with fibrous dysplasia. Br J Radiol. 1981. 54:1027–1033.13. Harris WH, Dudley HR Jr, Barry RJ. The natural history of fibrous dysplasia. An orthopaedic, pathological, and roentgenographic study. J Bone Joint Surg Am. 1962. 44-A:207–233.14. Hermann G, Klein M, Abdelwahab IF, Kenan S. Fibrocartilaginous dysplasia. Skeletal Radiol. 1996. 25:509–511.15. Drolshagen LF, Reynolds WA, Marcus NW. Fibrocartilaginous dysplasia of bone. Radiology. 1985. 156:32.16. Taoka T, Mayr NA, Lee HJ, Yuh WT, Simonson TM, Rezai K, Berbaum KS. Factors influencing visualization of vertebral metastases on MR imaging versus bone scintigraphy. AJR Am J Roentgenol. 2001. 176:1525–1530.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteosarcoma of the Patella (1 Case)
- Intraosseous Well Differentiated Osteosarcoma: A case report
- FDG-PET/CT Complements Bone Scan with Respect to the Detection of Skip Metastasis of Osteosarcoma: A Case Report
- Non Blood Transfusion Limb Salvage Operation in the Distal Femur Osteosarcoma Patient: A Case Report
- Spontaneous osteosarcoma of the femur in a non-obese diabetic mouse