J Korean Bone Joint Tumor Soc.
2014 Jun;20(1):36-40. 10.5292/jkbjts.2014.20.1.36.
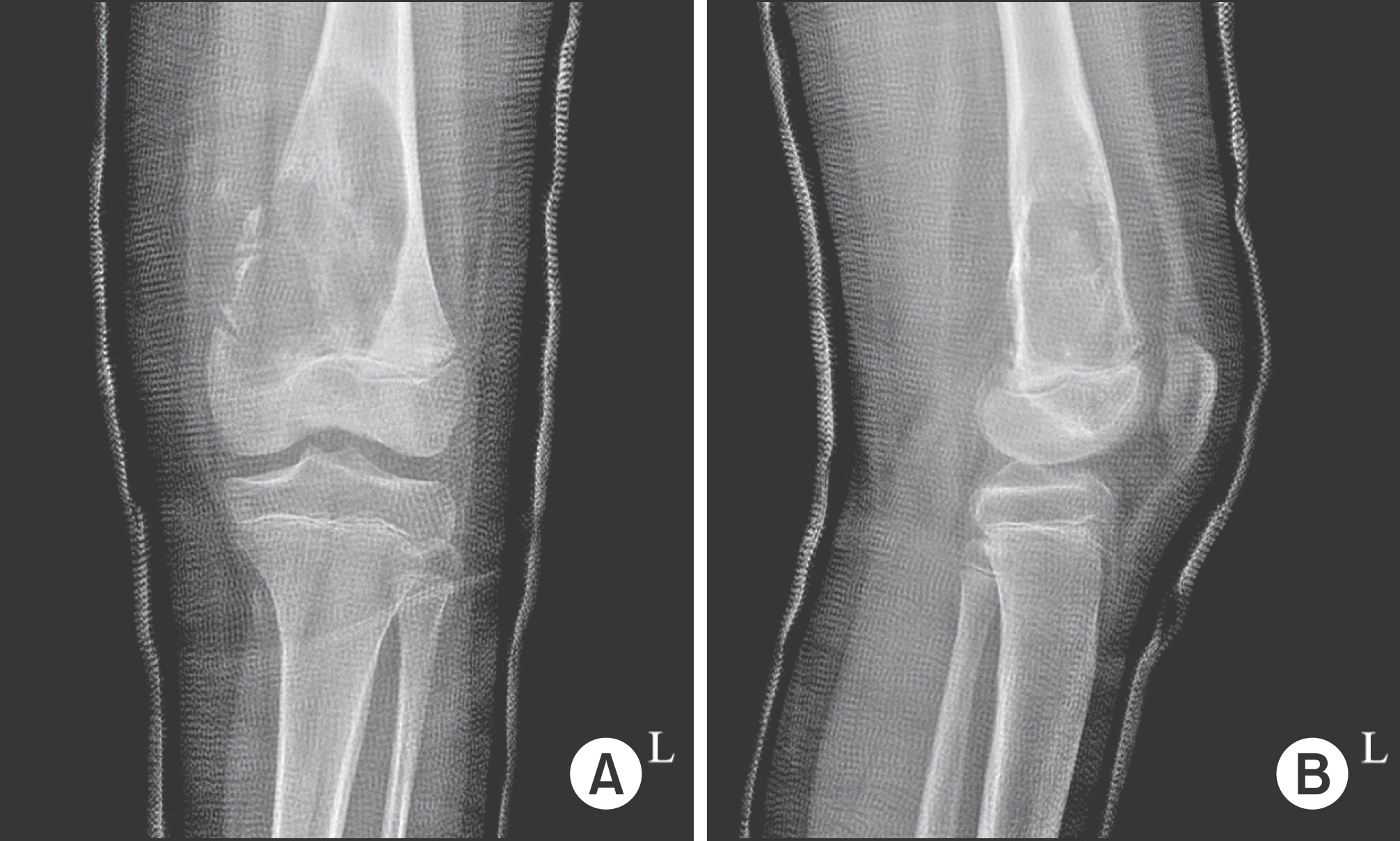
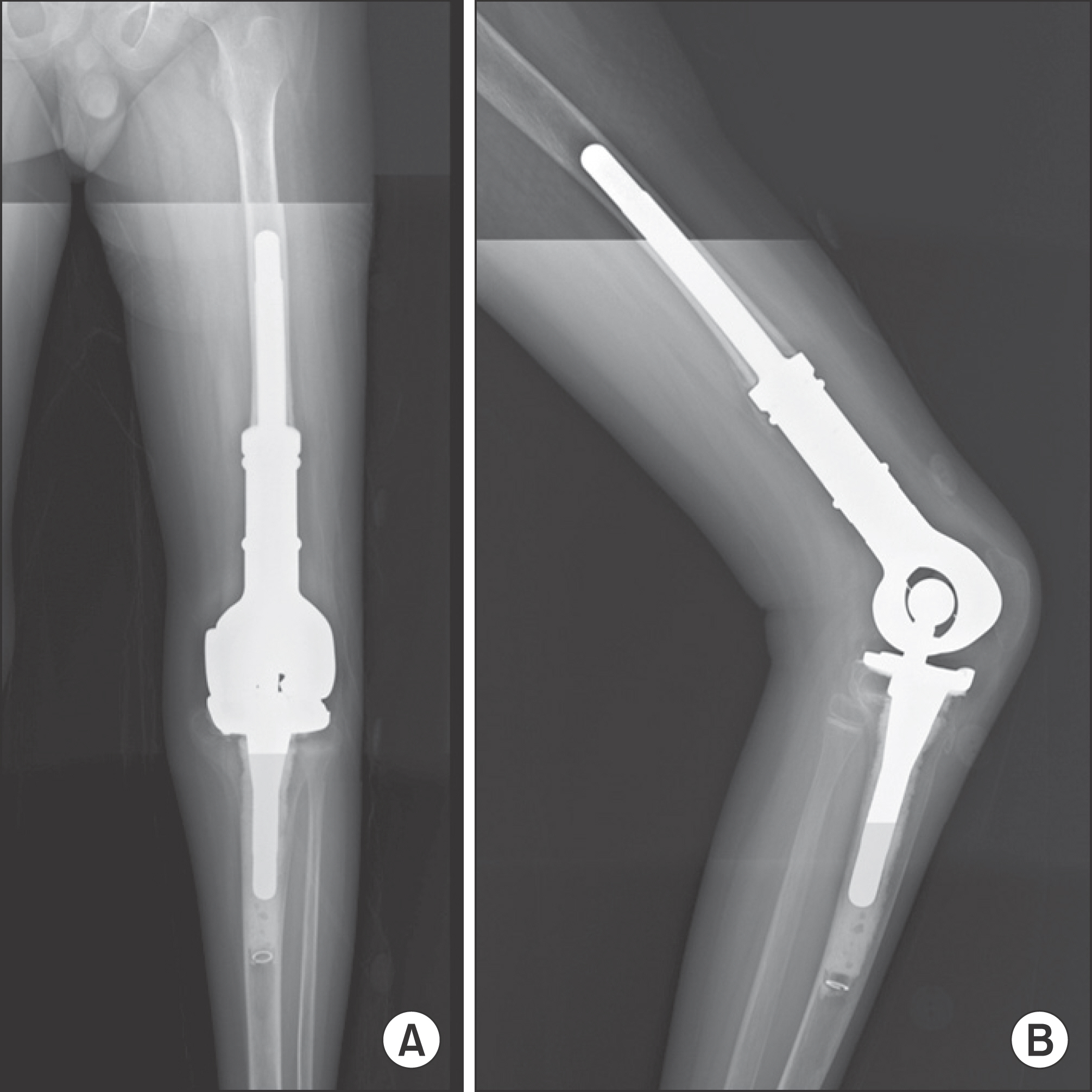
Non Blood Transfusion Limb Salvage Operation in the Distal Femur Osteosarcoma Patient: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea University Hospital, Seoul, Korea. pjh1964@hanmail.net
- KMID: 1707764
- DOI: http://doi.org/10.5292/jkbjts.2014.20.1.36
Abstract
- Limb salvage operations for osteosarcoma of the extremity usually consist of wide excision and skeletal reconstruction. Most osteosarcoma patients are anemic prior to the surgery as majority of them undergo preoperative neo-adjuvant chemotherapy; thus, it is necessary to treat anemia before and after the surgery since limb salvage operation tends to accompany significant blood loss. Despite the fact that blood transfusion has bad influence on prognosis, complication, and postoperative outcome of cancer patients, it is still considered as a standard management to fix anemia for limb salvage operations. We would like to present a case report in which the authors succeeded in performing limb salvage operations on patients with distal femur osteosarcoma without transfusion.
MeSH Terms
Figure
Reference
-
References
1. Dunne JR, Malone D, Tracy JK, Gannon C, Napolitano LM. Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. J Surg Res. 2002; 102:237–44.
Article2. Sugezawa A, Kaibara N, Sumi K, et al. Blood transfusion and the prognosis of patients with gastric cancer. J Surg Oncol. 1989; 42:113–6.
Article3. Wells AW, Mounter PJ, Chapman CE, Stainsby D, Wallis JP. Where does blood go? Prospective observational study of red cell transfusion in north England. BMJ. 2002; 325:803–6.
Article4. Gombotz H, Rehak PH, Shander A, Hofmann A. Blood use in elective surgery: the Austrian benchmark study. Transfusion. 2007; 47:1468–80.
Article5. Speiss BD. Transfusion and outcome in heart surgery. Ann Thorac Surg. 2002; 74:986–7.
Article6. Seeber P, Shander A. Basics of blood management. 2nd ed.West Sussex: Wiley-Blackwell;2012. 148.7. Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J. Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res. 2008; 466:1710–5.
Article8. Pape A, Habler O. Alternatives to allogeneic blood transfusions. Best Pract Res Clin Anaesthesiol. 2007; 21:221–39.
Article9. Kiss H, Raffl M, Neumann D, Hutter J, Dorn U. Epinephrine-augmented hypotensive epidural anesthesia replaces tourniquet use in total knee replacement. Clin Orthop Relat Res. 2005; 436:184–9.
Article10. Ong SM, Taylor GJ. Can knee position save blood following total knee replacement? Knee. 2003; 10:81–5.
Article11. Bock M, Müller J, Bach A, Böhrer H, Martin E, Motsch J. Effects of preinduction and intraoperative warming during major laparotomy. Br J Anaesth. 1998; 80:159–63.
Article12. Waters JH, Donnenberg AD. Blood salvage and cancer surgery: should we do it? Transfusion. 2009; 49:2016–8.13. Yoo YC, Shim JK, Kim JC, Jo YY, Lee JH, Kwak YL. Effect of single recombinant human erythropoietin injection on transfusion requirements in preoperatively anemic patients undergoing valvular heart surgery. Anesthesiology. 2011; 115:929–37.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Limb Salvage Surgery in a Rare Case of Recurrent Parosteal Osteosarcoma with Vascular Graft Thrombosis
- Functional Evaluation of Tumor Prosthetic Arthroplasty for the Malignant Bone Tumor around the Knee: Interim Report
- Spontaneous Pneumothorax as a Complication of Pulmonary Metastasis of Osteosarcoma A case report
- Reconstructive Arthrodesis using a Non-living Fibular Graft with an Attached Periosteal Sleeve for Osteosarcoma of the Distal Tibia: A Case Report
- Treatment of Malignant Bone Tumors by Tumor Prosthesis